Anatomic Variation in Intrahepatic Bile Ducts: an Analysis of Intraoperative Cholangiograms in 300 Consecutive Donors for Living Donor Liver Transplantation
- Affiliations
-
- 1Department of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. tkkim@amc.seoul.kr
- KMID: 1118810
- DOI: http://doi.org/10.3348/kjr.2003.4.2.85
Abstract
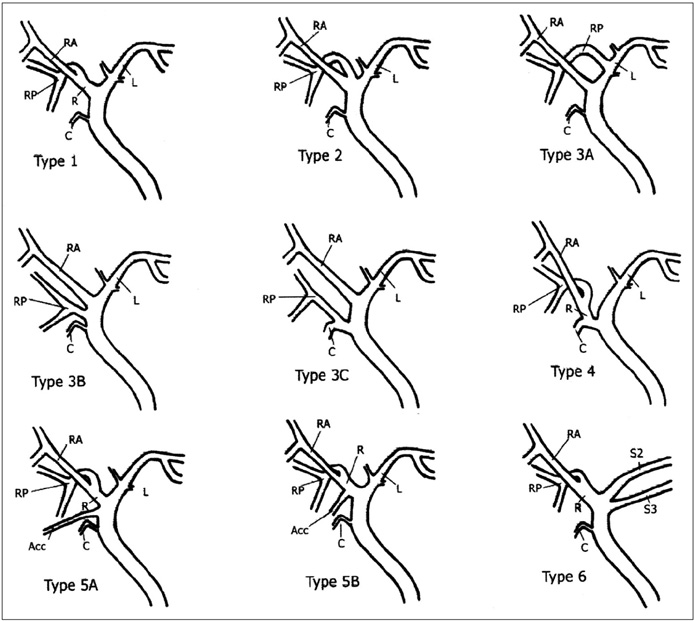
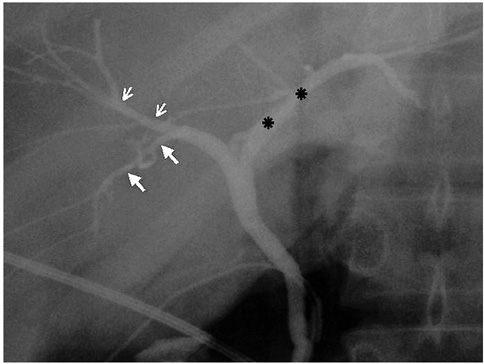
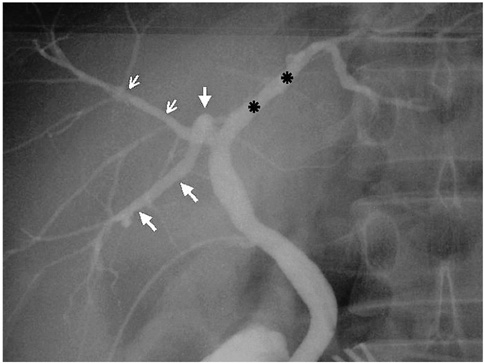
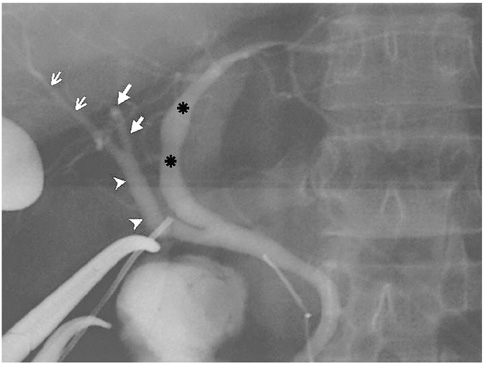
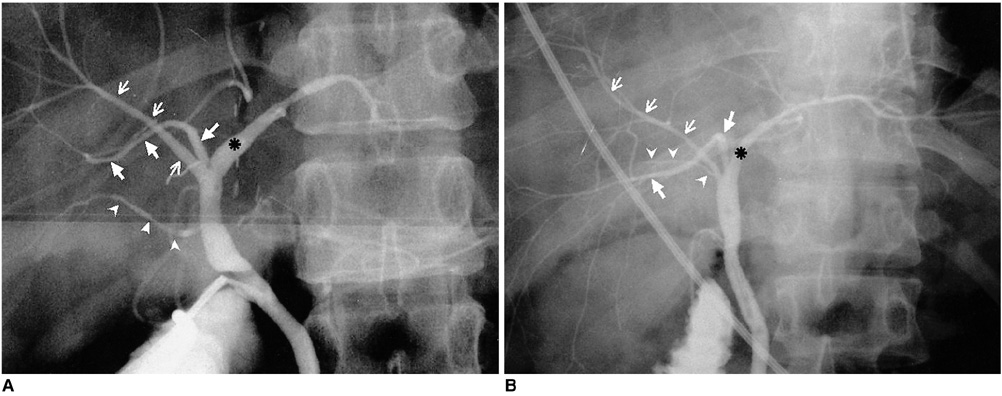
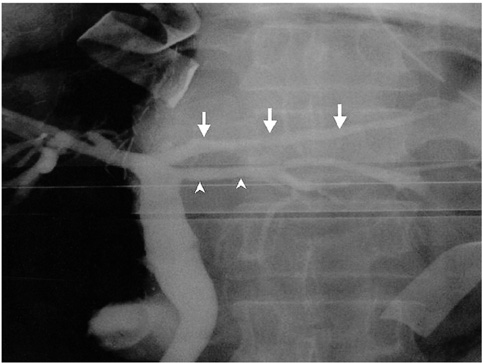
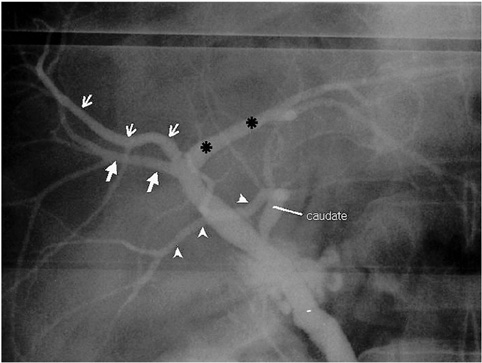
OBJECTIVE
To describe the anatomical variation occurring in intrahepatic bile ducts (IHDs) in terms of their branching patterns, and to determine the frequency of each variation. MATERIALS AND METHODS: The study group consisted of 300 consecutive donors for liver transplantation who underwent intraoperative cholangiography. Anatomical variation in IHDs was classified according to the branching pattern of the right anterior and right posterior segmental duct (RASD and RPSD, respectively), and the presence or absence of the first-order branch of the left hepatic duct (LHD), and of an accessory hepatic duct. RESULTS: The anatomy of the intrahepatic bile ducts was typical in 63% of cases (n=188), showed triple confluence in 10% (n=29), anomalous drainage of the RPSD into the LHD in 11% (n=34), anomalous drainage of the RPSD into the common hepatic duct (CHD) in 6% (n=19), anomalous drainage of the RPSD into the cystic duct in 2% (n=6), drainage of the right hepatic duct (RHD) into the cystic duct (n=1), the presence of an accessory duct leading to the CHD or RHD in 5% (n=16), individual drainage of the LHD into the RHD or CHD in 1% (n=4), and unclassified or complex variation in 1% (n=3). CONCLUSION: The branching pattern of IHDs was atypical in 37% of cases. The two most common variations were drainage of the RPSD into the LHD (11%) and triple confluence of the RASD, RPSD and LHD (10%).
Figure
Cited by 3 articles
-
Isolated aberrant right cysticohepatic duct injury during laparoscopic cholecystectomy: Evaluation and treatment challenges of a severe postoperative complication associated with an extremely rare anatomical variant
Konstantinos Vasiliadis, Elena Moschou, Sofia Papaioannou, Panagiotis Tzitzis, Albion Totsi, Stamatia Dimou, Eleni Lazaridou, Dimitrios Kapetanos, Christos Papavasiliou
Ann Hepatobiliary Pancreat Surg. 2020;24(2):221-227. doi: 10.14701/ahbps.2020.24.2.221.Cystic duct patch closure of remnant bile duct in living donor hepatectomy when primary closure is difficult: An easy solution
Subash Gupta, Rajasekhar Kandagaddala, Shaleen Agarwal, Rajesh Dey, Selvakumar Naganathan, Peeyush Varshney, Nilesh Patil
Ann Hepatobiliary Pancreat Surg. 2020;24(4):513-517. doi: 10.14701/ahbps.2020.24.4.513.The Variation of Hepatic Duct Confluence and Asymptomatic Common Bile Duct Stone with Routine Intraoperative Cholangiogram during Laparoscopic Cholecystectomy
Se Young Kim, Ki Ho Kim, Il Dong Kim, Byung Sun Suh, Dong Woo Shin, Sang Wook Kim, Jin Soo Park, Hye In Lim
Korean J Gastroenterol. 2011;58(6):338-345. doi: 10.4166/kjg.2011.58.6.338.
Reference
-
1. Clemett AR. Berk BN, Clemett AR, editors. Operative and postoperative cholangiography. Radiology of the gallbladder and bile ducts. 1977. 1st ed. Philadelphia: Saunders;272–284.2. Huang TL, Cheng YF, Chen CL, Chen TY, Lee TY. Variants of the bile ducts: clinical application in the potential donor of living-related hepatic transplantation. Transplant Proc. 1996. 28:1669–1670.3. Cheng YF, Huang TL, Chen CL, Chen YS, Lee TY. Variants of the intrahepatic bile ducts: application in living-related liver transplantation and splitting liver transplantation. Clin Transplant. 1997. 11:337–340.4. Mortele KJ, Ros PR. Anatomic variants of the biliary tree: MR cholangiographic findings and clinical applications. AJR Am J Roentgenol. 2001. 177:389–394.5. Nery JR, Fragulidis GP, Scagnelli T, et al. Donor biliary variation: an overlooked problem? Clin Transplant. 1997. 11:582–587.6. Gulliver DJ, Cotton PB, Baillie J. Anatomic variants and artifacts in ERCP interpretation. AJR Am J Roentgenol. 1991. 156:975–980.7. Gazelle GS, Lee MJ, Mueller PR. Cholangiographic segmental anatomy of the liver. RadioGraphics. 1994. 14:1005–1013.8. Puente SG, Bannura GC. Radiological anatomy of the biliary tract: variation and congenital abnormalities. World J Surg. 1983. 7:271–276.9. Kim MH, Sekijima J, Lee SF. Primary intrahepatic stones. Am J Gastroenterol. 1995. 90:540–548.10. Kim HJ, Kim MH, Lee SK, et al. Normal structure, variations and anomalies of the pancreaticobiliary ducts of Koreans: a nationwide cooperative prospective study. Gastrointest Endosc. 2002. 55:889–896.11. Turner MA, Fulcher AS. The cystic duct: normal anatomy and disease processes. RadioGraphics. 2001. 21:3–22.12. Champetier J, Letoublon C, Alnaasan I, Charvin B. The cysticohepatic ducts: surgical implications. Surg Radiol Anat. 1991. 13:203–211.13. Hamlin JA. Berci G, Hamlin JA, editors. Biliary ductal anomalies. Operative biliary radiology. 1981. 1st ed. Baltimore: Williams & Wilkins;110–116.14. Reid SH, Cho SR, Shaw CI, Turner MA. Anomalous hepatic duct inserting into the cystic duct. AJR Am J Roentgenol. 1986. 147:1181–1182.15. Park CH, Cho HJ, Kwack EY, Choi CS, Kang IW, Yoon JS. Intrahepatic biliary duct anatomy and its variations. J Korean Radiol Soc. 1991. 27:827–831.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Role of Bile Duct Probe for Bile Duct Division during Donor Right Hemihepatectomy
- Two Cases of Percutaneous Transhepatic Choledochoscopy Treatment of Intrahepatic Duct Stones that Occurred after Living Donor Liver Transplantation
- Endoscopic management of anastomotic stricture after living-donor liver transplantation
- Hyperthermia associated with biliary obstruction during living donor liver transplantation
- Single Center Experience of Biliary Reconstruction in Living Donor Liver Transplantation: Duct-to-Duct Anastomosis