Differentiation between Benign and Malignant Solid Thyroid Nodules Using an US Classification System
- Affiliations
-
- 1Department of Radiology, Busan Paik Hospital, Inje University College of Medicine, Busan 614-725, Korea. dwultra@lycos.co.kr
- 2Department of General Surgery (Thyroid & Breast Clinic), Busan Paik Hospital, Inje University College of Medicine, Busan 614-725, Korea.
- 3Department of Otorhinolaryngology-Head & Neck Surgery, Busan Paik Hospital, Inje University College of Medicine, Busan 614-725, Korea.
- 4Department of Pathology, Busan Paik Hospital, Inje University College of Medicine, Busan 614-725, Korea.
- 5Department of Radiology, Cancer Center, Dongnam Institute of Radiological and Medical Science, Busan 619-953, Korea.
- 6Department of Radiology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul 110-746, Korea.
- KMID: 1116441
- DOI: http://doi.org/10.3348/kjr.2011.12.5.559
Abstract
OBJECTIVE
To evaluate the diagnostic accuracy of a new ultrasound (US) classification system for differentiating between benign and malignant solid thyroid nodules.
MATERIALS AND METHODS
In this study, we enrolled 191 consecutive patients who received real-time US and subsequent US diagnoses for solid thyroid nodules, and underwent US-guided fine-needle aspiration. Each thyroid nodule was prospectively classified into 1 of 5 diagnostic categories by real-time US: "malignant," "suspicious for malignancy," "borderline," "probably benign," and "benign". We evaluated the diagnostic accuracy of thyroid US and the cut-off US criteria by comparing the US diagnoses of thyroid nodules with cytopathologic results.
RESULTS
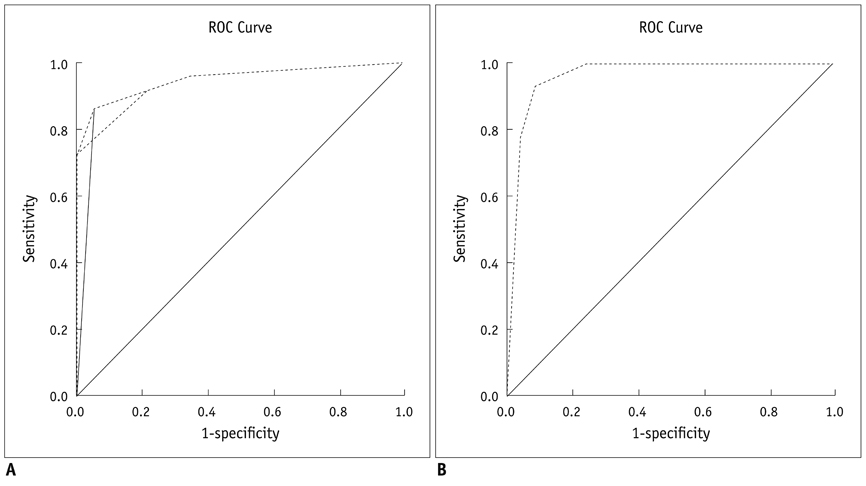
Of the 191 solid nodules, 103 were subjected to thyroid surgery. US categories for these 191 nodules were malignant (n = 52), suspicious for malignancy (n = 16), borderline (n = 23), probably benign (n = 18), and benign (n = 82). A receiver-operating characteristic curve analysis revealed that the US diagnosis for solid thyroid nodules using the 5-category US classification system was very good. The sensitivity, specificity, positive and negative predictive values, and accuracy of US diagnosis were 86%, 95%, 91%, 92%, and 92%, respectively, when benign, probably benign, and borderline categories were collectively classified as benign (negative).
CONCLUSION
The diagnostic accuracy of thyroid US for solid thyroid nodules is high when the above-mentioned US classification system is applied.
MeSH Terms
Figure
Cited by 2 articles
-
Primary Imaging Test and Appropriate Biopsy Methods for Thyroid Nodules: Guidelines by Korean Society of Radiology and National Evidence-Based Healthcare Collaborating Agency
Eun Ju Ha, Hyun Kyung Lim, Jung Hyun Yoon, Jung Hwan Baek, Kyung Hyun Do, Miyoung Choi, Jin A Choi, Min Lee, Dong Gyu Na,
Korean J Radiol. 2018;19(4):623-631. doi: 10.3348/kjr.2018.19.4.623.Guidelines for Primary Imaging Test and Biopsy Methods in the Diagnosis of Thyroid Nodules: Joint Report by the Korean Society of Radiology and National Evidence-Based Healthcare Collaborating Agency
Hyun Kyung Lim, Eun Ju Ha, In Young Youn, Jung Hyun Yoon, Jung Hwan Baek, Kyung Hyun Do, Miyoung Choi, Jin A Choi, Min Lee, Dong Gyu Na
J Korean Soc Radiol. 2018;79(1):1-10. doi: 10.3348/jksr.2018.79.1.1.
Reference
-
1. Kim EK, Park CS, Chung WY, Oh KK, Kim DI, Lee JT, et al. New sonographic criteria for recommending fine-needle aspiration biopsy of nonpalpable solid nodules of the thyroid. AJR Am J Roentgenol. 2002. 178:687–691.2. Cappelli C, Castellano M, Pirola I, Cumetti D, Agosti B, Gandossi E, et al. The predictive value of ultrasound findings in the management of thyroid nodules. QJM. 2007. 100:29–35.3. Salmaslioglu A, Erbil Y, Dural C, Issever H, Kapran Y, Ozarmagan S, et al. Predictive value of sonographic features in preoperative evaluation of malignant thyroid nodules in a multinodular goiter. World J Surg. 2008. 32:1948–1954.4. Horvath E, Majlis S, Rossi R, Franco C, Niedmann JP, Castro A, et al. An ultrasonogram reporting system for thyroid nodules stratifying cancer risk for clinical management. J Clin Endocrinol Metab. 2009. 94:1748–1751.5. Papini E, Guglielmi R, Bianchini A, Crescenzi A, Taccogna S, Nardi F, et al. Risk of malignancy in nonpalpable thyroid nodules: predictive value of ultrasound and color-Doppler features. J Clin Endocrinol Metab. 2002. 87:1941–1946.6. Iannuccilli JD, Cronan JJ, Monchik JM. Risk for malignancy of thyroid nodules as assessed by sonographic criteria: the need for biopsy. J Ultrasound Med. 2004. 23:1455–1464.7. Frates MC, Benson CB, Doubilet PM, Cibas ES, Marqusee E. Can color Doppler sonography aid in the prediction of malignancy of thyroid nodules? J Ultrasound Med. 2003. 22:127–131. quiz 132-134.8. Shimura H, Haraguchi K, Hiejima Y, Fukunari N, Fujimoto Y, Katagiri M, et al. Distinct diagnostic criteria for ultrasonographic examination of papillary thyroid carcinoma: a multicenter study. Thyroid. 2005. 15:251–258.9. Moon WJ, Jung SL, Lee JH, Na DG, Baek JH, Lee YH, et al. Benign and malignant thyroid nodules: US differentiation--multicenter retrospective study. Radiology. 2008. 247:762–770.10. Tae HJ, Lim DJ, Baek KH, Park WC, Lee YS, Choi JE, et al. Diagnostic value of ultrasonography to distinguish between benign and malignant lesions in the management of thyroid nodules. Thyroid. 2007. 17:461–466.11. Katz JF, Kane RA, Reyes J, Clarke MP, Hill TC. Thyroid nodules: sonographic-pathologic correlation. Radiology. 1984. 151:741–745.12. Brander A, Viikinkoski P, Nickels J, Kivisaari L. Thyroid gland: US screening in a random adult population. Radiology. 1991. 181:683–687.13. Wienke JR, Chong WK, Fielding JR, Zou KH, Mittelstaedt CA. Sonographic features of benign thyroid nodules: interobserver reliability and overlap with malignancy. J Ultrasound Med. 2003. 22:1027–1031.14. Brkljacic B, Cuk V, Tomic-Brzac H, Bence-Zigman Z, Delic-Brkljacic D, Drinkovic I. Ultrasonic evaluation of benign and malignant nodules in echographically multinodular thyroids. J Clin Ultrasound. 1994. 22:71–76.15. Kim DW, Lee EJ, In HS, Kim SJ. Sonographic differentiation of partially cystic thyroid nodules: a prospective study. AJNR Am J Neuroradiol. 2010. 31:1961–1966.16. Lee MJ, Kim EK, Kwak JY, Kim MJ. Partially cystic thyroid nodules on ultrasound: probability of malignancy and sonographic differentiation. Thyroid. 2009. 19:341–346.17. Frates MC, Benson CB, Charboneau JW, Cibas ES, Clark OH, Coleman BG, et al. Management of thyroid nodules detected at US: Society of Radiologists in Ultrasound consensus conference statement. Radiology. 2005. 237:794–800.18. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009. 19:1167–1214.19. Moon WJ, Baek JH, Jung SL, Kim DW, Kim EK, Kim JY, et al. Ultrasonography and the ultrasound-based management of thyroid nodules: consensus statement and recommendations. Korean J Radiol. 2011. 12:1–14.20. Kessler A, Rappaport Y, Blank A, Marmor S, Weiss J, Graif M. Cystic appearance of cervical lymph nodes is characteristic of metastatic papillary thyroid carcinoma. J Clin Ultrasound. 2003. 31:21–25.21. Ying M, Ahuja A, Metreweli C. Diagnostic accuracy of sonographic criteria for evaluation of cervical lymphadenopathy. J Ultrasound Med. 1998. 17:437–445.22. Kakkos SK, Scopa CD, Chalmoukis AK, Karachalios DA, Spiliotis JD, Harkoftakis JG, et al. Relative risk of cancer in sonographically detected thyroid nodules with calcifications. J Clin Ultrasound. 2000. 28:347–352.23. Kwak MS, Baek JH, Kim YS, Jeong HJ. Patterns and Significance of Peripheral Calcifications of Thyroid Tumors seen on Ultrasound. J Korean Radiol Soc. 2005. 53:401–405.24. Wang N, Xu Y, Ge C, Guo R, Guo K. Association of sonographically detected calcification with thyroid carcinoma. Head Neck. 2006. 28:1077–1083.25. Kim BM, Kim MJ, Kim EK, Kwak JY, Hong SW, Son EJ, et al. Sonographic differentiation of thyroid nodules with eggshell calcifications. J Ultrasound Med. 2008. 27:1425–1430.26. Park M, Shin JH, Han BK, Ko EY, Hwang HS, Kang SS, et al. Sonography of thyroid nodules with peripheral calcifications. J Clin Ultrasound. 2009. 37:324–328.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Thyroid Nodule
- US findings of thyroid carcinomas developed in multinodular goiters
- Ultrasound Elastography in Differential Diagnosis of Benign and Malignant Thyroid Nodules
- Natural Course of Cytologically Diagnosed Benign Thyroid Nodules
- Ultrasonographic Findings of Thyroid Nodules: Differentiation between Malignant and Benign Nodules