Korean J Radiol.
2005 Sep;6(3):185-195. 10.3348/kjr.2005.6.3.185.
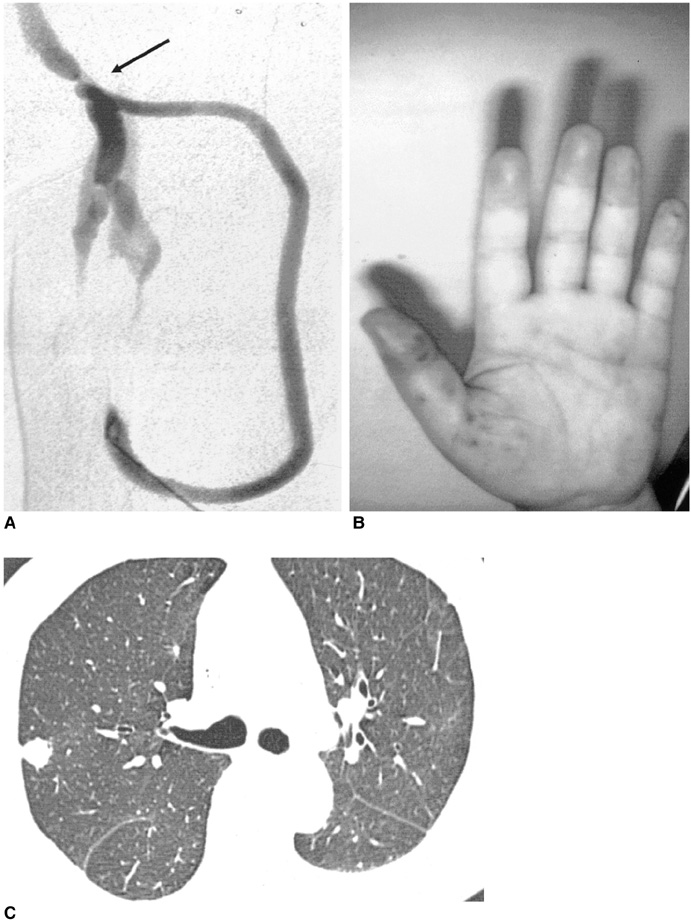
Endovascular Management of Immediate Procedure-Related Complications of Failed Hemodialysis Access Recanalization
- Affiliations
-
- 1Department of Radiology, Chosun University Hospital, Korea. dhk1107@hanmail.net
- 2Department of Radiology, Soonchunhyang University Hospital, Korea.
- 3Department of General Surgery, Soonchunhyang University Hospital, Korea.
- KMID: 1102716
- DOI: http://doi.org/10.3348/kjr.2005.6.3.185
Abstract
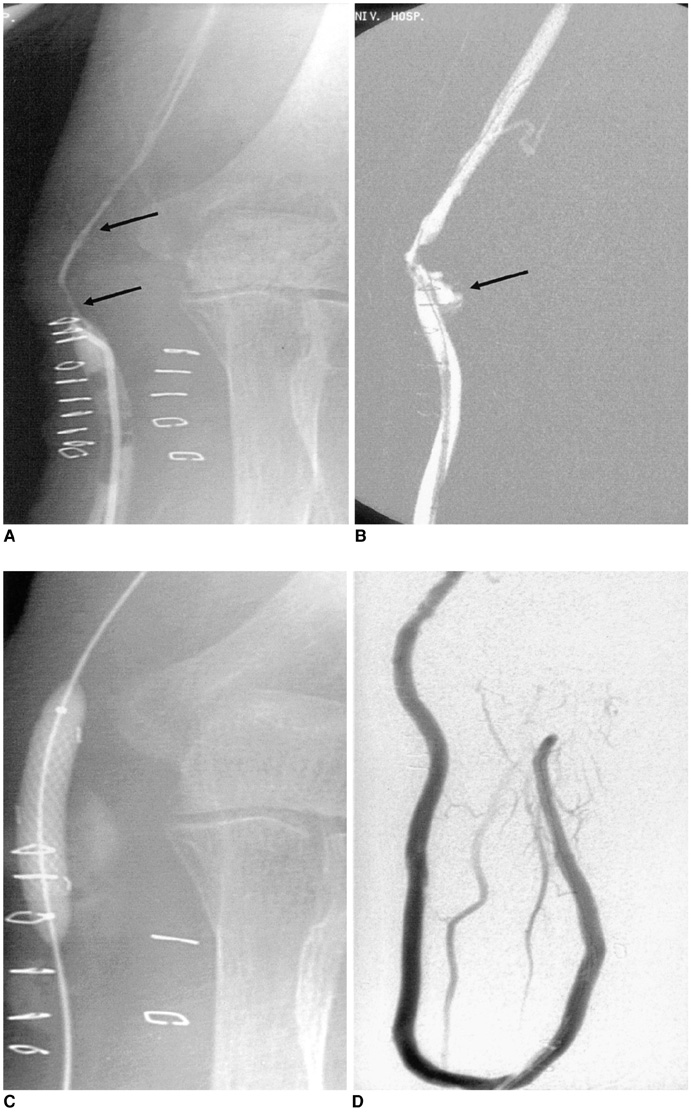
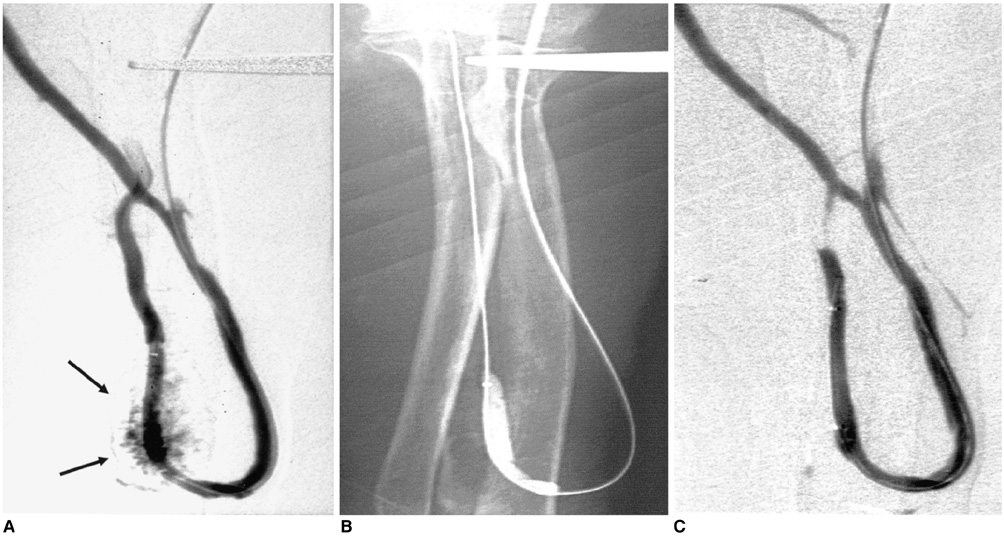
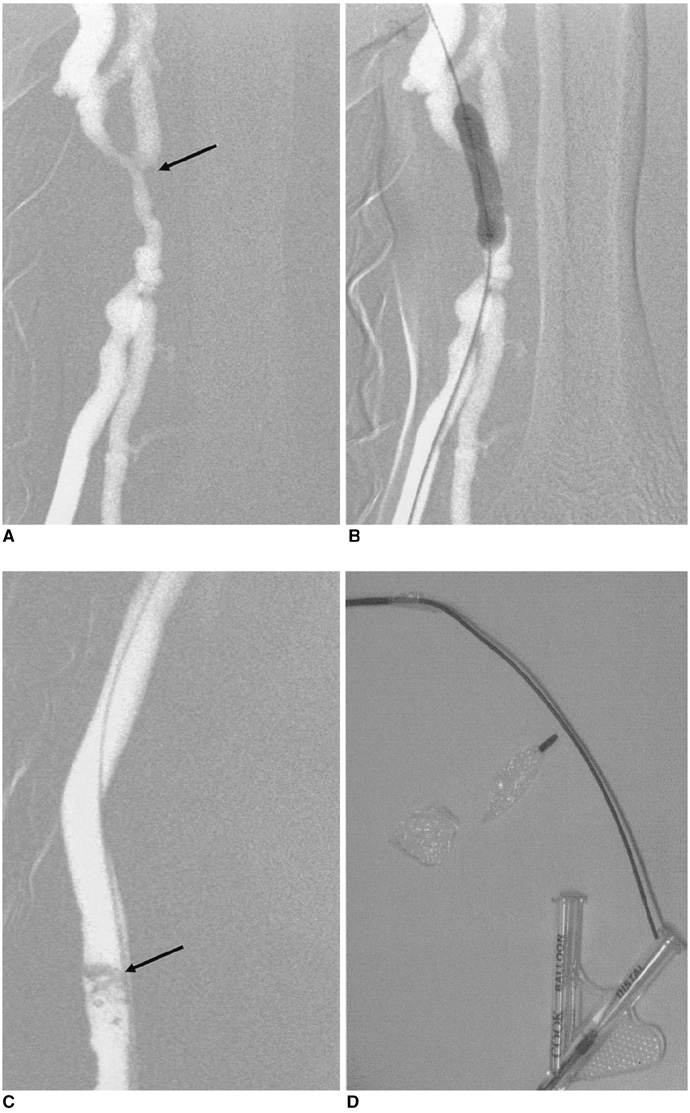
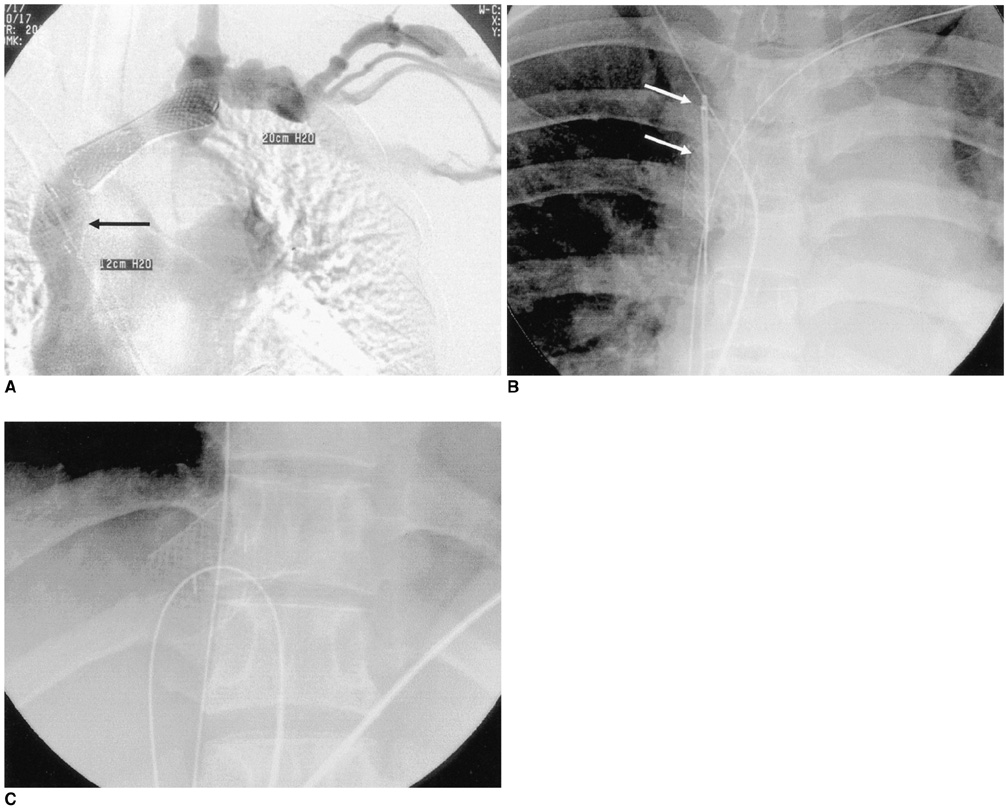
- Endovascular procedures are becoming the standard type of care for the management of hemodialysis vascular access dysfunction. As with any type of medical procedure, these techniques can result in procedure-related complications, although the expected number of complications is low. The clinical extent of these complications varies from case to case. Management of these cases depends on the clinical presentation. Major complications such as vein rupture, arterial embolism, remote site bleeding or hematoma, symptomatic pulmonary embolism and puncture site complications necessitating treatment require major therapy. Minor complications such as non-flow compromising small puncture site hematoma or pseudoaneurysms require little or no therapy. It is essential that the interventionist be prepared to manage these complications appropriately when they arise.
Keyword
MeSH Terms
Figure
Reference
-
1. Sacks D, Marinelli DL, Martin LG, Spies JB. Society of Interventional Radiology Technology Assessment Committee. Reporting standards for clinical evaluation of new peripheral arterial revascularization devices. J Vasc Interv Radiol. 2003. 14(9Pt2):S395–S404.2. Sullivan KL, Besarab A, Bonn J, Shapiro MJ, Gardiner GA Jr, Moritz MJ. Hemodynamics of failing dialysis grafts. Radiology. 1993. 186:867–872.3. Weng FL, Berns JS. Complications of percutaneous treatment of thrombosed hemodialysis access grafts. Semin Dial. 2003. 16:257–262.4. Sofocleous CT, Schur I, Koh E, Hinrichs C, Cooper SG, Welber A, et al. Percutaneous treatment of complications occurring during hemodialysis graft recanalization. Eur J Radiol. 2003. 47:237–246.5. Trerotola SO, Lund GB, Scheel PJ Jr, Savader SJ, Venbrux AC, Osterman FA Jr. Thrombosed dialysis access grafts: percutaneous mechanical declotting without urokinase. Radiology. 1994. 191:721–726.6. Valji K, Bookstein JJ, Roberts AC, Davis GB. Pharmacomechanical thrombolysis and angioplasty in the management of clotted hemodialysis grafts: early and late clinical results. Radiology. 1991. 178:243–247.7. Beathard GA. Percutaneous transvenous angioplasty in the treatment of vascular access stenosis. Kidney Int. 1992. 42:1390–1397.8. Turmel-Rodriguez L, Pengloan J, Blanchier D, et al. Insufficient dialysis shunts: improved long-term patency rates with close hemodynamic monitoring, repeated percutaneous balloon angioplasty and stent placement. Radiology. 1993. 187:273–278.9. Beathard GA. Angioplasty for arteriovenous grafts and fistulae. Semin Nephrol. 2002. 22:202–210.10. Rundback JH, Leonardo RF, Poplausky MR, Rozenblit G. Venous rupture complicating hemodialysis access angioplasty: percutaneous treatment and outcomes in seven patients. AJR Am J Roentgenol. 1998. 171:1081–1084.11. Funaki B, Szymski GX, Leef JA, Rosenblum JD, Burke R, Hackworth CA. Wallstent deployment to salvage dialysis graft thrombolysis complicated by venous rupture: early and intermediate results. AJR Am J Roentgenol. 1997. 169:1435–1437.12. Beathard GA, Welch BR, Maidment HJ. Mechanical thrombolysis for the treatment of thrombosed hemodialysis access grafts. Radiology. 1996. 200:711–716.13. Trerotola SO, Johnson MS, Shah H, Namyslowski J. Backbleeding technique for treatment of arterial emboli resulting from dialysis graft thrombolysis. J Vasc Interv Radiol. 1998. 9(1Pt1):141–143.14. Cohen MA, Kumpe DA, Durham JD, Zwerdlinger SC. Improved treatment of thrombosed hemodialysis access sites with thrombolysis and angioplasty. Kidney Int. 1994. 46:1375–1380.15. Slonim SM, Dake MD, Razavi MK, Kee ST, Samuels SL, Rhee JS, et al. Management of misplaced or migrated endovascular stents. J Vasc Interv Radiol. 1999. 10:851–859.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endovascular Therapy to Salvage Hemodialysis Access
- Proximal Vein Obstruction or Stenosis Failed to Angioplasty in Hemodialysis Patients: Treatment with Endovascular Stent
- Endovascular Management for Malfunctioning Hemodialysis Access
- Clinical Experience with a Hybrid Procedure Using the Adherent Clot Catheter for Salvage of Thrombosed Hemodialysis Access: A Comparison with the Standard Fogarty Balloon Catheter
- Endovascular interventions for central vein stenosis