Korean J Ophthalmol.
2010 Feb;24(1):23-28. 10.3341/kjo.2010.24.1.23.
Circadian Blood Pressure and Intraocular Pressure Patterns in Normal Tension Glaucoma Patients with Undisturbed Sleep
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University College of Medicine, Seoul, Korea. kihopark@snu.ac.kr
- 2Seoul Artificial Eye Center, Seoul National University Hospital Clinical Research Institute, Seoul, Korea.
- 3Jongro Kong Eye Clinic, Seoul, Korea.
- 4Kangbuk Samsung Hospital, Seoul, Korea.
- KMID: 1098789
- DOI: http://doi.org/10.3341/kjo.2010.24.1.23
Abstract
-
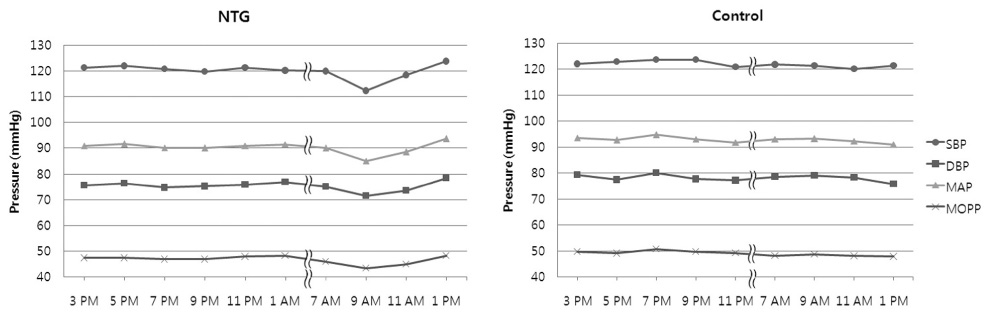
PURPOSE: To investigate and compare the circadian pattern of blood pressure (BP), intraocular pressure (IOP) and mean ocular perfusion pressure (MOPP) while experiencing undisturbed sleep in normal-tension glaucoma (NTG) and non-glaucoma control patient groups.
METHODS
Twenty-four eyes from 24 patients diagnosed with NTG and 22 eyes from 22 control group patients were enrolled. Systolic BP, diastolic BP and IOP were measured every two hours except for the period of time from 1 AM to 7 AM in the NTG group and from 11 PM to 7 AM in the control group over a one-day period. IOP and hemodynamic parameters were then compared between the two groups. NTG patients were subdivided according to the degree of morning BP dip and IOP, and hemodynamic parameters and visual field indices (mean deviation and pattern standard deviation) were also compared among these subgroups.
RESULTS
There were no significant differences in mean systolic BP, mean diastolic BP and mean arterial pressure (MAP) between the NTG and the control groups. The NTG group showed a significantly large morning BP dip compared to the control group (7.1+/-4.2% vs. 3.8+/-3.4%, p=0.022). However, there were no significant differences in mean or fluctuation of MOPP between the two groups. Morning over-dippers showed significantly large MAP and MOPP fluctuations compared to non-dippers and dippers, while there were no significant differences in visual field indices among the three subgroups.
CONCLUSIONS
NTG patients showed significant morning BP dips compared to the control group. The marked morning BP dip was associated with significantly large MAP or MOPP fluctuations but was not associated with visual field indices.
Keyword
MeSH Terms
Figure
Reference
-
1. Collaborative Normal-Rension Glaucoma Study Group. The effectiveness of intraocular pressure reduction in the treatment of normal-tension glaucoma. Am J Ophthalmol. 1998. 126:498–505.2. Heijl A, Leske MC, Bengtsson B, et al. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol. 2002. 120:1268–1279.3. Kass MA, Heuer DK, Higginbotham EJ, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002. 120:701–713.4. Higginbotham EJ, Gordon MO, Beiser JA, et al. The Ocular Hypertension Treatment Study: topical medication delays or prevents primary open-angle glaucoma in African American individuals. Arch Ophthalmol. 2004. 122:813–820.5. Hayreh SS, Zimmerman MB, Podhajsky P, Alward WL. Nocturnal arterial hypotension and its role in optic nerve head and ocular ischemic disorders. Am J Ophthalmol. 1994. 117:603–624.6. Flammer J, Orgul S. Optic nerve blood-flow abnormalities in glaucoma. Prog Retin Eye Res. 1998. 17:267–289.7. Bonomi L, Marchini G, Marraffa M, et al. Vascular risk factors for primary open angle glaucoma: the Egna-Neumarkt Study. Ophthalmology. 2000. 107:1287–1293.8. Flammer J, Orgul S, Costa VP, et al. The impact of ocular blood flow in glaucoma. Prog Retin Eye Res. 2002. 21:359–393.9. Fuchsjager-Mayrl G, Wally B, Georgopoulos M, et al. Ocular blood flow and systemic blood pressure in patients with primary open-angle glaucoma and ocular hypertension. Invest Ophthalmol Vis Sci. 2004. 45:834–839.10. Sehi M, Flanagan JG, Zeng L, et al. Relative change in diurnal mean ocular perfusion pressure: a risk factor for the diagnosis of primary open-angle glaucoma. Invest Ophthalmol Vis Sci. 2005. 46:561–567.11. Tielsch JM, Katz J, Sommer A, et al. Hypertension, perfusion pressure, and primary open-angle glaucoma: a population-based assessment. Arch Ophthalmol. 1995. 113:216–221.12. Leske MC, Wu SY, Nemesure B, Hennis A. Incident open-angle glaucoma and blood pressure. Arch Ophthalmol. 2002. 120:954–959.13. Verdecchia P, Schillaci G, Guerrieri M, et al. Circadian blood pressure changes and left ventricular hypertrophy in essential hypertension. Circulation. 1990. 81:528–536.14. Veerman DP, Imholz BP, Wieling W, et al. Circadian profile of systemic hemodynamics. Hypertension. 1995. 26:55–59.15. Liu JH. Circadian rhythm of intraocular pressure. J Glaucoma. 1998. 7:141–147.16. Liu JH, Kripke DF, Hoffman RE, et al. Nocturnal elevation of intraocular pressure in young adults. Invest Ophthalmol Vis Sci. 1998. 39:2707–2712.17. Liu JH, Zhang X, Kripke DF, Weinreb RN. Twenty-four-hour intraocular pressure pattern associated with early glaucomatous changes. Invest Ophthalmol Vis Sci. 2003. 44:1586–1590.18. Choi J, Jeong J, Cho HS, Kook MS. Effect of nocturnal blood pressure reduction on circadian fluctuation of mean ocular perfusion pressure: a risk factor for normal tension glaucoma. Invest Ophthalmol Vis Sci. 2006. 47:831–836.19. Choi J, Kim KH, Jeong J, et al. Circadian fluctuation of mean ocular perfusion pressure is a consistent risk factor for normal-tension glaucoma. Invest Ophthalmol Vis Sci. 2007. 48:104–111.20. Doughty MJ, Zaman ML. Human corneal thickness and its impact on intraocular pressure measures: a review and meta-analysis approach. Surv Ophthalmol. 2000. 44:367–408.21. Kario K, Matsuo T, Kobayashi H, et al. Nocturnal fall of blood pressure and silent cerebrovascular damage in elderly hypertensive patients. Advanced silent cerebrovascular damage in extreme dippers. Hypertension. 1996. 27:130–135.22. Plange N, Kaup M, Daneljan L, et al. 24-h blood pressure monitoring in normal tension glaucoma: night-time blood pressure variability. J Hum Hypertens. 2006. 20:137–142.23. Kaiser HJ, Flammer J, Graf T, Stumpfig D. Systemic blood pressure in glaucoma patients. Graefes Arch Clin Exp Ophthalmol. 1993. 231:677–680.24. Graham SL, Drance SM. Nocturnal hypotension: role in glaucoma progression. Surv Ophthalmol. 1999. 43:Suppl 1. S10–S16.25. Kashiwagi K, Hosaka O, Kashiwagi F, et al. Systemic circulatory parameters. comparison between patients with normal tension glaucoma and normal subjects using ambulatory monitoring. Jpn J Ophthalmol. 2001. 45:388–396.26. Harris A, Evans D, Martin B, et al. Nocturnal blood pressure reduction: effect on retrobulbar hemodynamics in glaucoma. Graefes Arch Clin Exp Ophthalmol. 2002. 240:372–378.27. O'Brien E, Murphy J, Tyndall A, et al. Twenty-four-hour ambulatory blood pressure in men and women aged 17 to 80 years: the Allied Irish Bank Study. J Hypertens. 1991. 9:355–360.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Circadian Biorhythmicity in Normal Pressure Hydrocephalus - A Case Series Report
- The Effect of Oral Calcium Channel Blockers on the Ocular Blood Flow
- The Acute Effect of Betaxolol and Difivefrin on Optic Nerve Head and Retinal Blood Flow in Normal Tension Glaucoma
- Intraocular Pressure and Axial Length in Children
- The Short-Term Effect of Prostaglandin Analog Monotherapy on Corneal Biomechanical Properties in Normal Tension Glaucoma Patients