Korean J Lab Med.
2011 Apr;31(2):98-100. 10.3343/kjlm.2011.31.2.98.
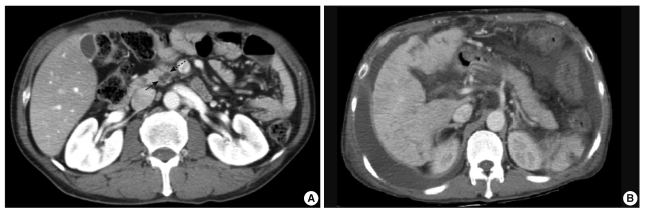
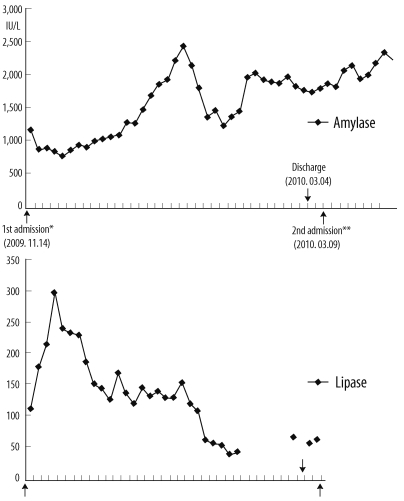
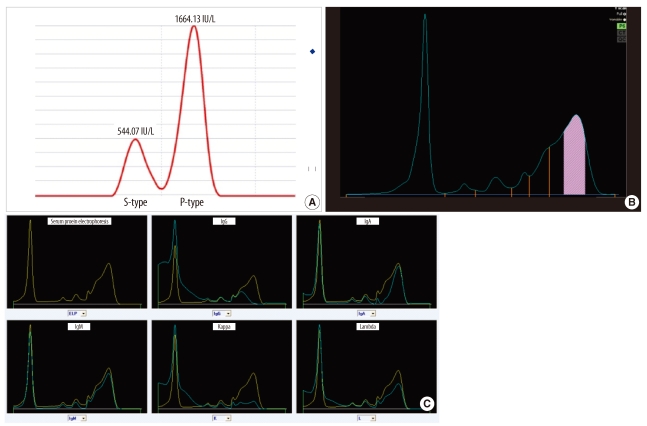
Overlapping Presence of Macroamylasemia and Hyperamylasemia in Acute Pancreatitis
- Affiliations
-
- 1Department of Laboratory Medicine, Kyung Hee University School of Medicine, Seoul, Korea. Suhjt@hitel.net
- 2Department of Surgery, Ewha Womans University School of Medicine, Seoul, Korea.
- KMID: 1094348
- DOI: http://doi.org/10.3343/kjlm.2011.31.2.98
Abstract
- No abstract available.
MeSH Terms
Figure
Reference
-
1. Choi S, Ihm C, Jang S. Evaluation of the clinical usefulness for pancreatic amylase in acute pancreatitis. Korean J Lab Med. 2003; 23:98–103.2. Klonoff DC. Macroamylasemia and other immunoglobulin-complexed enzyme disorders. West J Med. 1980; 133:392–407. PMID: 6162278.3. Sagristani M, Guariglia R, Pocali B, De Rienzo M, Guastafierro S, Romano G, et al. Macroamylasemia in a patient with multiple myeloma. Leuk Lymphoma. 2002; 43:1705–1707. PMID: 12400618.
Article4. Lankisch PG, Doobe C, Finger T, Lübbers H, Mahlke R, Brinkmann G, et al. Hyperamylasaemia and/or hyperlipasaemia: incidence and underlying causes in hospitalized patients with non-pancreatic diseases. Scand J Gastroenterol. 2009; 44:237–241. PMID: 18819039.
Article5. Barera G, Bazzigaluppi E, Viscardi M, Renzetti F, Bianchi C, Chiumello G, et al. Macroamylasemia attributable to gluten-related amylase autoantibodies: a case report. Pediatrics. 2001; 107:E93. PMID: 11389291.
Article6. Van Gossum A. Macroamylasemia: a biochemical or clinical problem? Dig Dis. 1989; 7:19–27. PMID: 2466587.
Article7. Yoshida K, Minegishi Y, Okawa H, Yata J, Tokoi S, Kitagawa T, et al. Epstein-Barr virus-associated malignant lymphoma with macroamylasemia and monoclonal gammopathy in a patient with Wiskott-Aldrich syndrome. Pediatr Hematol Oncol. 1997; 14:85–89. PMID: 9021818.
Article8. Galasso PJ, Litin SC, O'Brien JF. The macroenzymes: a clinical review. Mayo Clin Proc. 1993; 68:349–354. PMID: 7681133.
Article9. Kobayashi T, Nakayama T, Kitamura M. Electrophoretic identification of serum immunoglobulins linked to amylase:macroamylase. Clin Chim Acta. 1978; 86:261–265. PMID: 668118.10. McPherson RA, Pincus MR, editors. Henry's clinical diagnosis and management by laboratory methods. 2007. 21st ed. St. Louis: Elsevier Saunders;p. 231–244.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Macroamylasemia in a 4-year-old girl with abdominal pain
- Macroamylasemia as a Rare Cause of Hyperamylasemia: A Case Report
- ERCP in Acute Pancreatitis
- Role of Oxygen - Derived Free Radical in the ERCF - Induced Hyperamylasemia
- Acute Pancreatitis Following Organophosphate Intoxication: Analysis of 6 Cases