Yonsei Med J.
2010 Sep;51(5):648-652. 10.3349/ymj.2010.51.5.648.
Optimal Use of the Halo-Vest Orthosis for Upper Cervical Spine Injuries
- Affiliations
-
- 1Department of Neurosurgery, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea. zunzae@hanmail.net
- 2Department of Neurosurgery, Mokdong Hospital, Ewha Womans University School of Medicine, Seoul, Korea.
- KMID: 1071414
- DOI: http://doi.org/10.3349/ymj.2010.51.5.648
Abstract
- PURPOSE
Upper cervical fractures can heal with conservative treatments such as halo-vest immobilization (HVI) and Minerva jackets without surgery. The most rigid of these, HVI, remains the most frequently used treatment in many centers despite its relatively high frequency of orthosis-related complications. We conducted this study to investigate the clinical outcome, effectiveness, patient satisfaction, and associated complications of HVI.
MATERIALS AND METHODS
From April 1997 to December 2008, we treated 23 patients for upper cervical spinal injuries with HVI. For analysis, we divided high cervical fractures into four groups, including C1 fracture, C2 dens fracture, C2 hangman's fracture, and C1-2 associated fracture. We evaluated the clinical outcome, complications, and patient satisfaction through chart reviews and a telephone questionnaire.
RESULTS
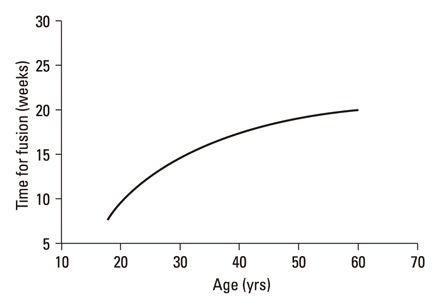
The healing rate for upper cervical fracture using HVI was 60.9%. In most cases, bony healing occurred within 16 weeks. Older patients required longer fusion time. We observed a 39.1% failure rate, and 60.9% of patients experienced complications. The most common complications were frequent pin loosening (34.8%; 8/23) and pin site infection (17.4%; 4/23). The HVI treatment failed in 66.7% of patients with pin site problems. The patient approval rate was 31.6%.
CONCLUSION
The HVI produced frequent complications and low patient satisfaction. Bony fusion succeeded in 60.9% of patients. Pin site complications showed a tendency to influence the outcome of HVI, and would be promptly addressed to prevent treatment failure if they develop. The decision to use HVI requires an explanation to the patient of potential complications and constant vigilance to prevent such complications and unsatisfactory outcomes.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Analysis of Risk Factors Associated with Fusion Failure of Traumatic Odontoid Fracture Type III after Halo-Vest Immobilization
Dong Kwang Seo, Jin Hoon Park, Dong Ho Lee, Sang Ryong Jeon
Korean J Neurotrauma. 2012;8(2):87-93. doi: 10.13004/kjnt.2012.08.0.87.
Reference
-
1. Clark CR, White AA 3rd. Fractures of the dens. A multicenter study. J Bone Joint Surg Am. 1985. 67:1340–1348.
Article2. Nickel VL, Perry J, Garrett A, Heppenstall M. The halo. A spinal skeletal traction fixation device. J Bone Joint Surg Am. 1968. 50:1400–1409.3. Garfin SR, Botte MJ, Waters RL, Nickel VL. Complications in the use of the halo fixation device. J Bone Joint Surg Am. 1986. 68:320–325.
Article4. Lind B, Sihlbom H, Nordwall A. Halo-vest treatment of unstable traumatic cervical spine injuries. Spine (Phila Pa 1976). 1988. 13:425–432.
Article5. Glaser JA, Whitehill R, Stamp WG, Jane JA. Complications associated with the halo-vest. A review of 245 cases. J Neurosurg. 1986. 65:762–769.6. Guiot B, Fessler RG. Complex atlantoaxial fractures. J Neurosurg. 1999. 91:139–143.
Article7. Kim DH, Vaccaro AR, Affonso J, Jenis L, Hilibrand AS, Albert TJ. Early predictive value of supine and upright X-ray films of odontoid fractures treated with halo-vest immobilization. Spine J. 2008. 8:612–618.
Article8. Ochoa G. Surgical management of odontoid fractures. Injury. 2005. 36:Suppl 2. B54–B64.
Article9. Rockswold GL, Bergman TA, Ford SE. Halo immobilization and surgical fusion: relative indications and effectiveness in the treatment of 140 cervical spine injuries. J Trauma. 1990. 30:893–898.10. Majercik S, Tashjian RZ, Biffl WL, Harrington DT, Cioffi WG. Halo vest immobilization in the elderly: a death sentence? J Trauma. 2005. 59:350–356.
Article11. Houtkin S, Levine DB. The halo yoke: a simplified device for attachment of the halo to a body cast. J Bone Joint Surg Am. 1972. 54:881–883.12. Daentzer D, Flörkemeier T. Conservative treatment of upper cervical spine injuries with the halo vest: an appropriate option for all patients independent of their age? J Neurosurg Spine. 2009. 10:543–550.
Article13. Bransford RJ, Stevens DW, Uyeji S, Bellabarba C, Chapman JR. Halo vest treatment of cervical spine injuries: a success and survivorship analysis. Spine (Phila Pa 1976). 2009. 34:1561–1566.14. Vieweg U, Schultheiss R. A review of halo vest treatment of upper cervical spine injuries. Arch Orthop Trauma Surg. 2001. 121:50–55.
Article15. Fabris Monterumici DA, Sinigaglia R. Long term results of halo-vest fixation for upper cervical spine fractures. Chir Narzadow Ruchu Ortop Pol. 2007. 72:71–79.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unstable C1, 2 Cervical Spine Injuries Treated with Halo vest
- Clinical Application of Halo-Vest Apparatus in Cervical Spine Lesions
- Surgical Experience of Cervical Spine Injury
- Clinical Analysis of the Result of Halo Immobilization Versus Surgical Fusion in the Management of Traumatic Cerical Spine Injury
- Traumatic Atlantoaxial Unifacetal Joint Dislocation Associated with Fractures of Ipsilateral C2 Body and Contralateral Pars