Yonsei Med J.
2011 Nov;52(6):914-922. 10.3349/ymj.2011.52.6.914.
Association of Lipoprotein-Associated Phospholipase A2 with Characteristics of Vulnerable Coronary Atherosclerotic Plaques
- Affiliations
-
- 1Department of Cardiology, The Qilu Hospital of Shandong University, Jinan, China. daixh@vip.sina.com
- 2Department of Cardiology, The Second Hospital of Shandong University, Jinan, China. yushengliu2004@yahoo.com.cn
- 3Division of Internal Medicine, The NO. 4th Hospital of Jinan City, Taishan Medical College, Jinan, China.
- KMID: 1058810
- DOI: http://doi.org/10.3349/ymj.2011.52.6.914
Abstract
- PURPOSE
Lipoprotein-associated phospholipase A2 (Lp-PLA2) is an inflammatory enzyme expressed in atherosclerotic plaques. We investigated the association of circulating Lp-PLA2 with characteristics of vulnerable coronary atherosclerotic plaques.
MATERIALS AND METHODS
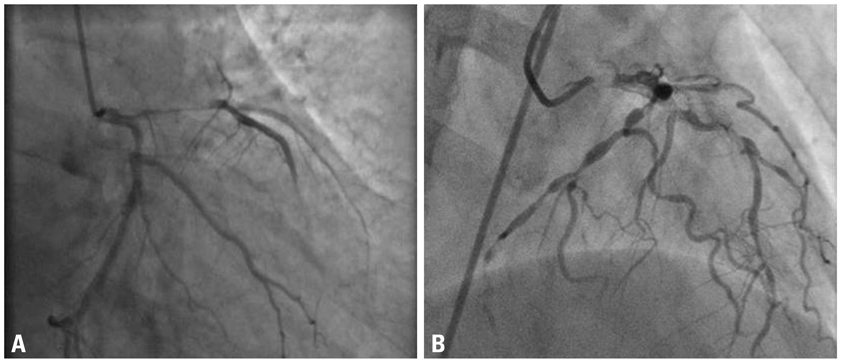
We recruited 113 patients with either unstable angina (UA, n=59) and stable angina (SA, n=54) by coronary angiography. Thirty-six healthy subjects served as controls. Intravascular ultrasound (IVUS) was used to evaluate the characteristics of coronary atherosclerotic plaque, and serum Lp-PLA2 concentration was measured as well.
RESULTS
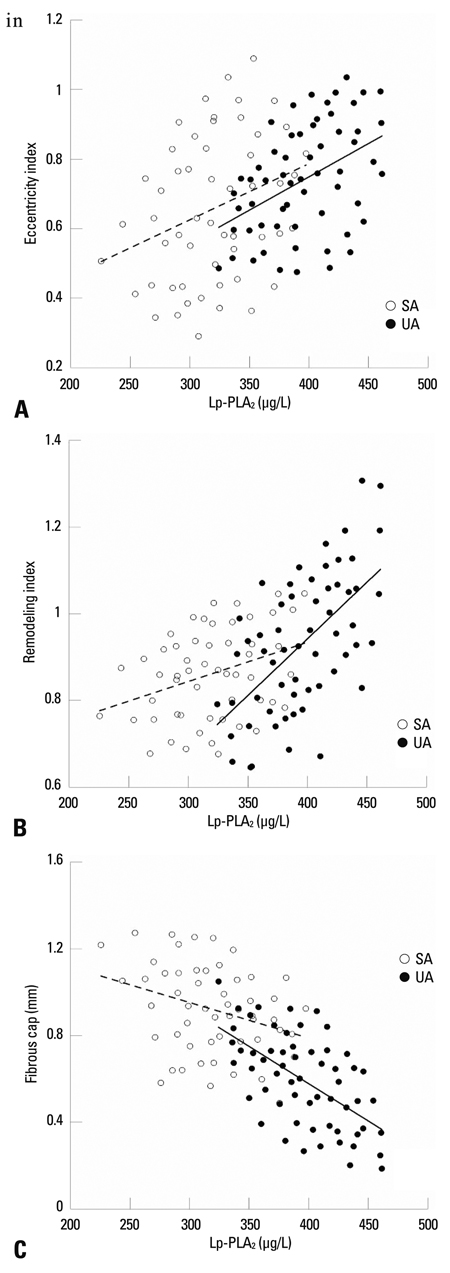
Lp-PLA2 concentration was significantly higher in both UA and SA patients [(396+/-36) microg/L and (321+/-39) microg/L, respectively] compared with the controls [(127+/-49) microg/L, p<0.01], and higher in UA than SA group. IVUS findings showed that remodeling index (RI) (0.91+/-0.15 vs. 0.85+/-0.11, p=0.005) and eccentricity index (EI) (0.73+/-0.16 vs. 0.65+/-0.22, p=0.039) were larger in UA than in SA group, and fibrous caps were thicker in SA than UA group [(0.91+/-0.23) mm vs. (0.63+/-0.21) mm, p=0.032]. Moreover, Lp-PLA2 correlated positively with EI (r=0.439, p<0.01) and RI (r=0.592, p<0.05) in UA group. There was an inverse relationship between Lp-PLA2 and fibrous cap thickness in both UA (r=-0.587, p<0.001) and SA (r=-0.318, p<0.05) groups. The independent risk factors in UA group were Lp-PLA2 (OR=1.055, 95% CI: 1.03-1.08, p=0.013), LDL-cholesterol (OR=0.032, 95% CI: 0.00-0.05, p=0.041) and fibrous cap thickness (OR=0.008, 95% CI: 0.00-0.45, p=0.019). Lp-PLA2 was strongly associated with both EI and fibrous cap thickness in both groups.
CONCLUSION
Serum level of Lp-PLA2 is associated with both eccentricity index and fibrous cap thickness in both UA and SA groups. Elevated levels of circulating Lp-PLA2 might to be a strong risk factor and more serious for unstable angina than stable angina.
MeSH Terms
Figure
Cited by 1 articles
-
Lipoprotein-Associated Phospholipase A2 Is Related to Plaque Stability and Is a Potential Biomarker for Acute Coronary Syndrome
Hyemoon Chung, Hyuck Moon Kwon, Jong-Youn Kim, Young Won Yoon, Jihyuk Rhee, Eui-Young Choi, Pil-Ki Min, Bum-Kee Hong, Se-Joong Rim, Ji Hyun Yoon, Sung-Joo Lee, Jong-Kwan Park, Myung-Hyun Kim, Minhee Jo, Jeong-Hee Yang, Byoung Kwon Lee
Yonsei Med J. 2014;55(6):1507-1515. doi: 10.3349/ymj.2014.55.6.1507.
Reference
-
1. Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med. 2004. 66:802–813.
Article2. Genest J. C-reactive protein: risk factor, biomarker and/or therapeutic target? Can J Cardiol. 2010. 26:Suppl A. 41A–44A.
Article3. Packard CJ, O'Reilly DS, Caslake MJ, McMahon AD, Ford I, Cooney J, et al. West of Scotland Coronary Prevention Study Group. Lipoprotein-associated phospholipase A2 as an independent predictor of coronary heart disease. N Engl J Med. 2000. 343:1148–1155.
Article4. Lp-PLA(2) Studies Collaboration. Thompson A, Gao P, Orfei L, Watson S, Di Angelantonio E, et al. Lipoprotein-associated phospholipase A(2) and risk of coronary disease, stroke, and mortality: collaborative analysis of 32 prospective studies. Lancet. 2010. 375:1536–1544.
Article5. Tellis CC, Tselepis AD. The role of lipoprotein-associated phospholipase A2 in atherosclerosis may depend on its lipoprotein carrier in plasma. Biochim Biophys Acta. 2009. 1791:327–338.
Article6. Asano K, Okamoto S, Fukunaga K, Shiomi T, Mori T, Iwata M, et al. Cellular source(s) of platelet-activating-factor acetylhydrolase activity in plasma. Biochem Biophys Res Commun. 1999. 261:511–514.
Article7. Stafforini DM, Elstad MR, McIntyre TM, Zimmerman GA, Prescott SM. Human macrophages secret platelet-activating factor acetylhydrolase. J Biol Chem. 1990. 265:9682–9687.
Article8. Zalewski A, Macphee C. Role of lipoprotein-associated phospholipase A2 in atherosclerosis: biology, epidemiology, and possible therapeutic target. Arterioscler Thromb Vasc Biol. 2005. 25:923–931.9. Häkkinen T, Luoma JS, Hiltunen MO, Macphee CH, Milliner KJ, Patel L, et al. Lipoprotein-associated phospholipase A(2), platelet-activating factor acetylhydrolase, is expressed by macrophages in human and rabbit atherosclerotic lesions. Arterioscler Thromb Vasc Biol. 1999. 19:2909–2917.10. Kolodgie FD, Burke AP, Skorija KS, Ladich E, Kutys R, Makuria AT, et al. Lipoprotein-associated phospholipase A2 protein expression in the natural progression of human coronary atherosclerosis. Arterioscler Thromb Vasc Biol. 2006. 26:2523–2529.
Article11. Naghavi M, Libby P, Falk E, Casscells SW, Litovsky S, Rumberger J, et al. From vulnerable plaque to vulnerable patient: a call for new definitions and risk assessment strategies: Part II. Circulation. 2003. 108:1772–1778.12. Mintz GS, Nissen SE, Anderson WD, Bailey SR, Erbel R, Fitzgerald PJ, et al. American College of Cardiology Clinical Expert Consensus Document on Standards for Acquisition, Measurement and Reporting of Intravascular Ultrasound Studies (IVUS). A report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2001. 37:1478–1492.
Article13. Tang D, Yang C, Zheng J, Woodard PK, Saffitz JE, Petruccelli JD, et al. Local maximal stress hypothesis and computational plaque vulnerability index for atherosclerotic plaque assessment. Ann Biomed Eng. 2005. 33:1789–1801.
Article14. Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005. 352:1685–1695.
Article15. Anderson JL. Lipoprotein-associated phospholipase A2: an independent predictor of coronary artery disease events in primary and secondary prevention. Am J Cardiol. 2008. 101:23F–33F.
Article16. Reddy KJ, Singh M, Bangit JR, Batsell RR. The role of lipoprotein-associated phospholipase A2 on cardiovascular disease risk assessment and plaque rupture: a clinical review. J Clin Lipidol. 2009. 3:85–93.
Article17. Rosenson RS. Lp-PLA(2) and risk of atherosclerotic vascular disease. Lancet. 2010. 375:1498–1500.
Article18. Brilakis ES, Khera A, McGuire DK, See R, Banerjee S, Murphy SA, et al. Influence of race and sex on lipoprotein-associated phospholipase A2 levels: observations from the Dallas Heart Study. Atherosclerosis. 2008. 199:110–115.
Article19. Virmani R, Burke AP, Kolodgie FD, Farb A. Pathology of the thin-cap fibroatheroma: a type of vulnerable plaque. J Interv Cardiol. 2003. 16:267–272.20. Kashiwagi M, Tanaka A, Kitabata H, Tsujioka H, Matsumoto H, Arita Y, et al. Relationship between coronary arterial remodeling, fibrous cap thickness and high-sensitivity C-reactive protein levels in patients with acute coronary syndrome. Circ J. 2009. 73:1291–1295.
Article21. Schoenhagen P, Ziada KM, Kapadia SR, Crowe TD, Nissen SE, Tuzcu EM. Extent and direction of arterial remodeling in stable versus unstable coronary syndromes: an intravascular ultrasound study. Circulation. 2000. 101:598–603.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Production of Phospholipase A2 in Different Types of Cultured Human Intervertebral Disc Cells
- Noninvasive Imaging of Atherosclerotic Plaques Using MRI and CT
- Recent Advances in the Development of PET/SPECT Probes for Atherosclerosis Imaging
- Statin Therapy with Coronary Plaque Imaging
- Multimodal intravascular photoacoustic and ultrasound imaging