Korean J Radiol.
2012 Feb;13(1):53-60. 10.3348/kjr.2012.13.1.53.
Right Gastric Venous Drainage: Angiographic Analysis in 100 Patients
- Affiliations
-
- 1Division of Intervention, Department of Radiology, Seoul National University Bundang Hospital, Gyeonggi-do 436-707, Korea.
- 2Department of Radiology, Seoul National University College of Medicine, Institute of Radiation Medicine, Seoul National University Medical Research Center, and Clinical Research Institute, Seoul National University Hospital, Seoul 110-744, Korea. chungjw@
- 3Interventional Radiology, Center for Liver Cancer, National Cancer Center, Gyeonggi-do 410-769, Korea.
- 4Department of Surgery and Research Institute of Clinical Medicine, Chonbuk National University Hospital, Jeollabuk-do 567-712, Korea.
- KMID: 1058793
- DOI: http://doi.org/10.3348/kjr.2012.13.1.53
Abstract
OBJECTIVE
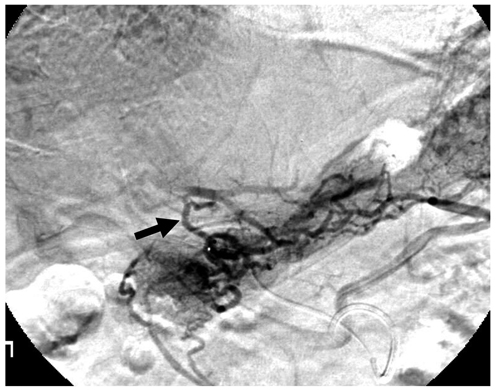
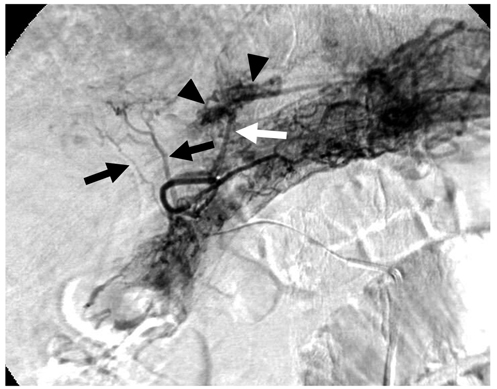
To evaluate the pattern of right gastric venous drainage by use of digital subtraction angiography.
MATERIALS AND METHODS
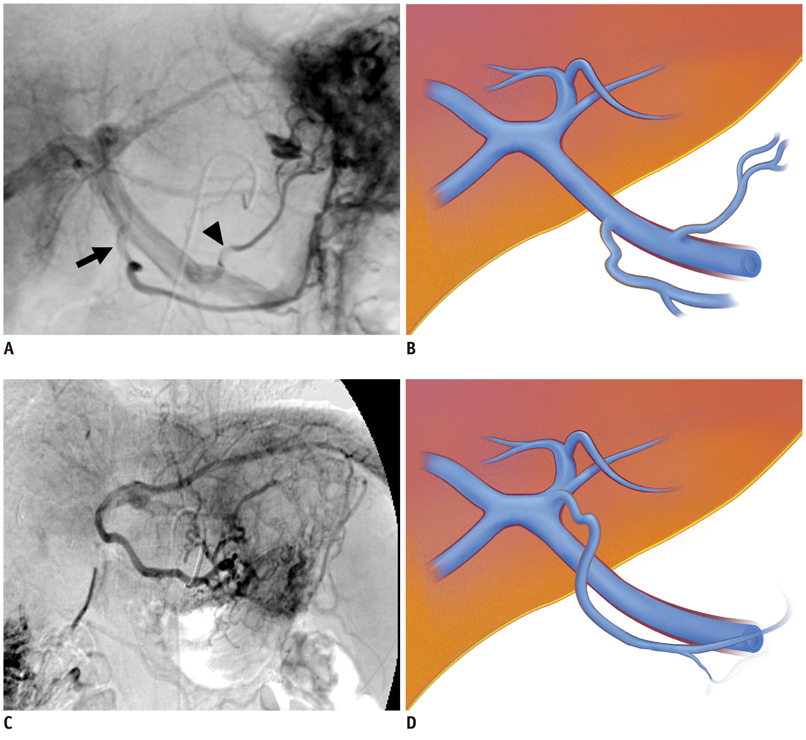
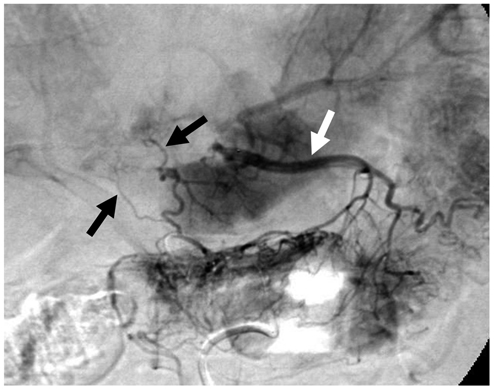
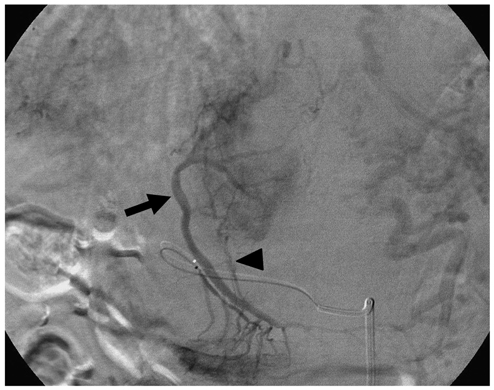
A series of 100 consecutive patients who underwent right gastric arteriography during transcatheter arterial chemoembolization for hepatocellular carcinoma were included in this study. Angiographic findings were retrospectively analyzed with respect to the presence or absence of the right and aberrant gastric veins, multiplicity of draining veins, aberrant right gastric venous drainage sites, and the termination pattern of aberrant right gastric veins (ARGVs). We also compared the relative size of the right and left gastric veins.
RESULTS
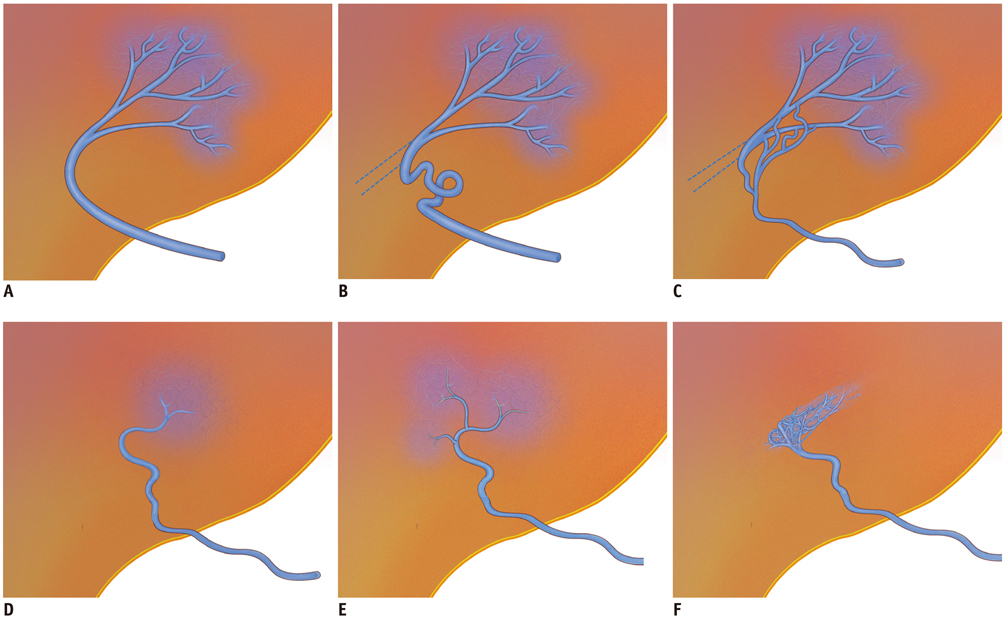
A total of 49 patients collectively had 66 ARGVs. The common drainage sites for the ARGVs included the hepatic segment IV (n = 35) and segment I (n = 15). The termination pattern of ARGV could be classified into 4 different types. The most common type was termination as a superficial parenchymal blush formation in small areas without demonstrable portal branches. A statistically significant difference was found for the dominancy of the right gastric vein in gastric venous drainage between the two groups with or without ARGV (p < 0.05, Fisher's exact test). In the group of patients without ARGV (n = 51), the right gastric vein was equal to (n = 9) or larger than (n = 17) the left gastric vein in 26 patients (26 of 51, 51%).
CONCLUSION
The incidence of ARGV is higher than expected with four distinct types in its termination pattern. The right gastric vein may play a dominant role in gastric venous drainage.
Keyword
MeSH Terms
Figure
Reference
-
1. Gilfillan RS, Hills HL. Anatomic study of the portal vein and its main branches. Arch Surg. 1950. 61:449–461.2. Deneve E, Caty L, Fontaine C, Guillem P. Simultaneous aberrant left and right gastric veins draining directly into the liver. Ann Anat. 2003. 185:263–266.3. Takayasu K, Aoki K, Ichikawa T, Ohmura T, Sekiguchi R, Terauchi T, et al. Aberrant right gastric vein directly communicating with left portal vein system. Incidence and implications. Acta Radiol. 1990. 31:575–577.4. Yoon KH, Matsui O, Kadoya M, Yoshigawa J, Gabata T, Arai K. Pseudolesion in segments II and III of the liver on CT during arterial portography caused by aberrant right gastric venous drainage. J Comput Assist Tomogr. 1999. 23:306–309.5. Caty L, Deneve E, Fontaine C, Guillem P. Concurrent aberrant right gastric vein directly draining into the liver and variations of the hepatic artery. Surg Radiol Anat. 2004. 26:70–73.6. Gabata T, Matsui O, Kadoya M, Ueda K, Kawamori Y, Yoshikawa J, et al. Aberrant gastric venous drainage in a focal spared area of segment IV in fatty liver: demonstration with color Doppler sonography. Radiology. 1997. 203:461–463.7. Kurosaki Y, Tanaka YO, Itai Y. Aberrant gastric venous drainage in focal fatty liver of segment IV: demonstration with sonography. AJR Am J Roentgenol. 1998. 171:897–898.8. Maeda H, Sato M, Kimura M, Kawai N, Sonomura T, Kishi K, et al. Focal fatty infiltration in the quadrate lobe of the liver accompanied by aberrant right gastric vein. Radiat Med. 1998. 16:61–64.9. Matsui O, Takahashi S, Kadoya M, Yoshikawa J, Gabata T, Takashima T, et al. Pseudolesion in segment IV of the liver at CT during arterial portography: correlation with aberrant gastric venous drainage. Radiology. 1994. 193:31–35.10. Tajima H, Murakami R, Tajima N, Kumazaki T. Aberrant right gastric vein draining directly into the quadrate lobe of the liver. A case report. Acta Radiol. 1995. 36:270–272.11. Kawamori Y, Matsui O, Takahashi S, Kadoya M, Takashima T, Miyayama S. Focal hepatic fatty infiltration in the posterior edge of the medial segment associated with aberrant gastric venous drainage: CT, US, and MR findings. J Comput Assist Tomogr. 1996. 20:356–359.12. Yamagami T, Nakamura T, Maeda T. Aberrant gastric venous inflow to the left lobe of the liver parenchyma adjacent to the falciform ligament. Br J Radiol. 1999. 72:903–905.13. Zhang J, Rath AM, Chevrel JP. Anatomic basis of venous drainage in gastric tubular esophagoplasty. Surg Radiol Anat. 1994. 16:221–228.14. del Pilar Fernandez M, Bernardino ME. Hepatic pseudolesion: appearance of focal low attenuation in the medial segment of the left lobe at CT arterial portography. Radiology. 1991. 181:809–812.15. Miyaki T, Yamada M, Kumaki K. Aberrant course of the left gastric vein in the human. Possibility of a persistent left portal vein. Acta Anat (Basel). 1987. 130:275–279.16. Couinaud C. The parabiliary venous system. Surg Radiol Anat. 1988. 10:311–316.17. Nelson RC, Thompson GH, Chezmar JL, Harned RK 2nd, Fernandez MP. CT during arterial portography: diagnostic pitfalls. Radiographics. 1992. 12:705–718. discussion 719-720.18. Ohashi I, Ina H, Gomi N, Himeno Y, Okada Y, Hanafusa K, et al. Hepatic pseudolesion in the left lobe around the falciform ligament at helical CT. Radiology. 1995. 196:245–249.19. Ohnishi K, Okuda K, Ohtsuki T, Nakayama T, Hiyama Y, Iwama S, et al. Formation of hilar collaterals or cavernous transformation after portal vein obstruction by hepatocellular carcinoma. Observations in ten patients. Gastroenterology. 1984. 87:1150–1153.20. Bezzi M, Broglia L, Lemos AA, Rossi P. Transjugular intrahepatic portosystemic shunt in portal vein thrombosis: role of the right gastric vein with anomalous insertion. Cardiovasc Intervent Radiol. 1995. 18:102–105.21. Parker RA, Seal RM. Cavernous transformation of the portal vein. J Pathol Bacteriol. 1955. 70:97–103.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Angiographic Analysis of Hemorrhagic Cerebral Arteriovenous Malformations
- Analysis of angiographic findings in cerebral arteriovenous malformations: Correlation with hemorrhage
- Gastric salvage after venous congestion during major pancreatic resections: A series of three cases
- Cortical versus Pial Venous Drainage in Dural Arteriovenous Fistula
- The Variants of Macular Choroidal Veins in ICG Angiography