Korean J Gastroenterol.
2011 Sep;58(3):153-156. 10.4166/kjg.2011.58.3.153.
A Case of Perforated Xanthogranulomatous Cholecystitis Presenting as Biloma
- Affiliations
-
- 1Department of Internal Medicine, Gyeongsang National University School of Medicine, Jinju, Korea. kimthy@medimail.co.kr
- 2Department of Pathology and Institute of Health Science, Gyeongsang National University School of Medicine, Jinju, Korea.
- KMID: 1018404
- DOI: http://doi.org/10.4166/kjg.2011.58.3.153
Abstract
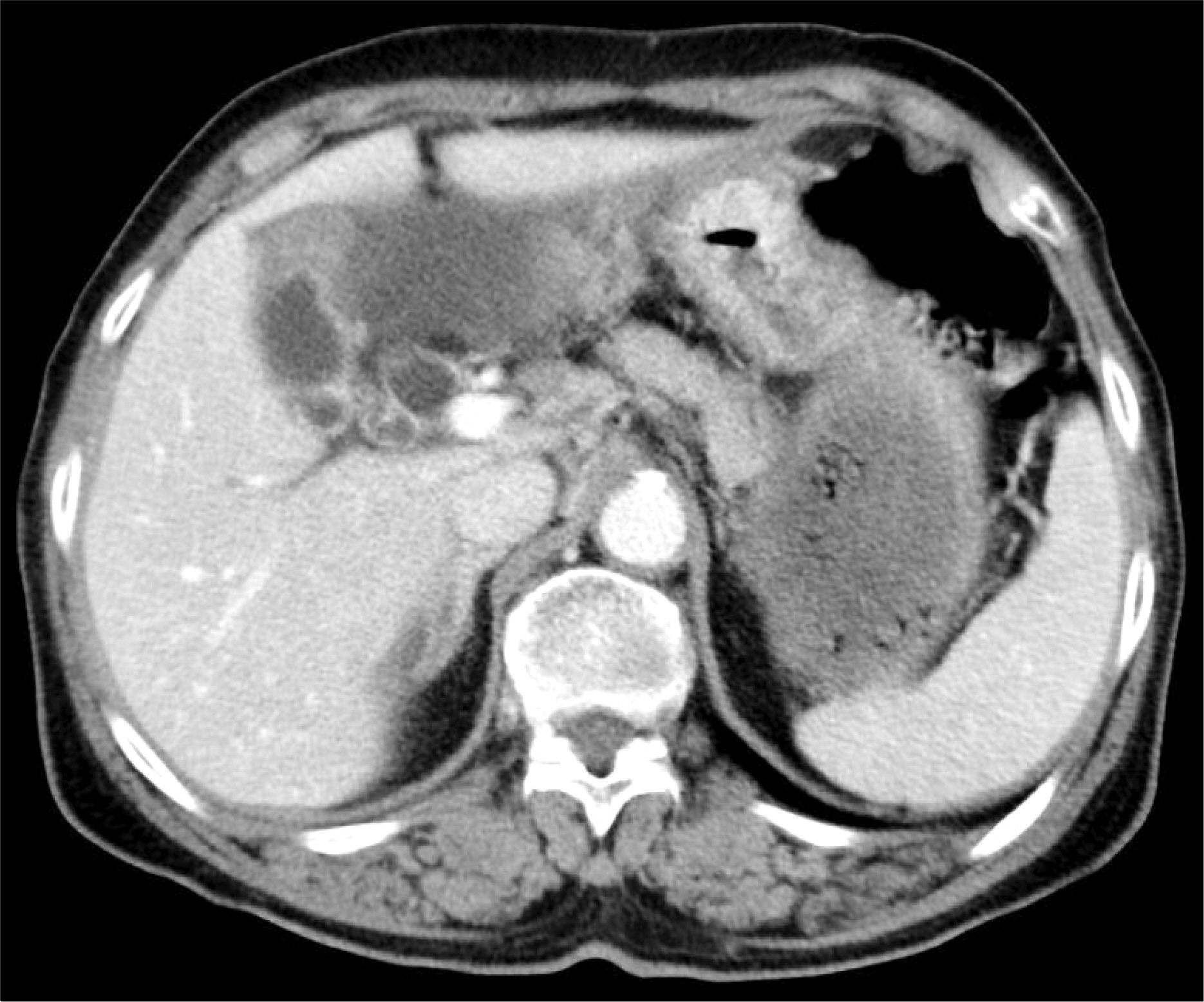
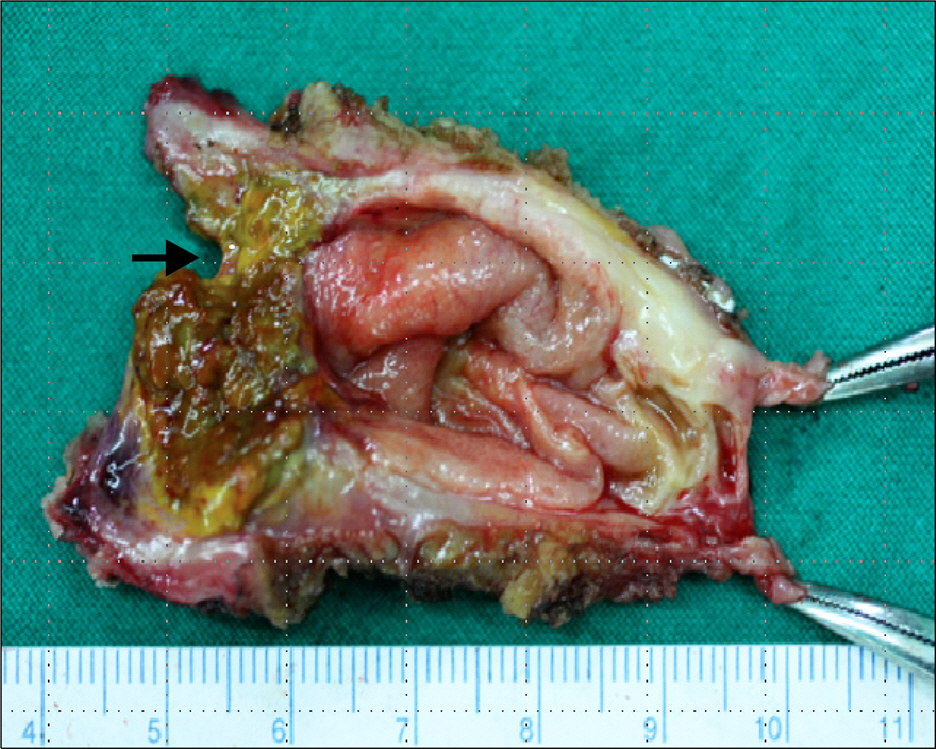
- Xanthogranulomatous cholecystitis is an unusual inflammatory disease of the gallbladder characterized by severe proliferative fibrosis and the accumulation of lipid-laden macrophages in areas of destructive inflammation. Its macroscopic appearance may occasionally be confused with gallbladder carcinoma. We present a case of perforated xanthogranulomatous cholecystitis presenting as biloma. An 80-year-old woman was referred to our hospital with a 1-week history of abdominal pain and febrile sensation. Abdominal CT showed a biloma in the subhepatic area. The follow-up CT showed that the biloma increased in size. Therefore, ultrasonography-guided aspiration was performed. The aspirated fluid/serum bilirubin ratio was greater than 5, which was strongly suggestive of bile leakage complicated by perforated cholecystitis. She underwent a laparoscopic cholecystectomy with cyst aspiration and adhesiolysis. A histological diagnosis of perforated xanthogranulomatous cholecystitis was made.
MeSH Terms
Figure
Reference
-
References
1. Hanada K, Nakata H, Nakayama T, et al. Radiologic findings in xanthogranulomatous cholecystitis. AJR Am J Roentgenol. 1987; 148:727–730.
Article2. Parra JA, Acinas O, Bueno J, Güezmes A, Fernández MA, Fariñas MC. Xanthogranulomatous cholecystitis: clinical, sonographic, and CT findings in 26 patients. AJR Am J Roentgenol. 2000; 174:979–983.3. Roberts KM, Parsons MA. Xanthogranulomatous cholecystitis: clinicopathological study of 13 cases. J Clin Pathol. 1987; 40:412–417.
Article4. Seo SH, Park JI, Kim JS, Kim KH, Choi CS, Choi YK. Xanthogranulomatous cholecystitis: a retrospective analysis of 36 cases. J Korean Surg Soc. 2009; 76:371–377.
Article5. Kim HY, Cho YH, Park JH. Xanthogranulomatous cholecystitis not associated with gallstone in a 9-year-old girl. J Korean Surg Soc. 2009; 77:72–74.
Article6. Joo YE, Lee JJ, Chung IJ, et al. A case of xanthogranulomatous cholecystitis. Korean J Intern Med. 1999; 14:90–93.
Article7. Kim DS, Choi DY, Kim YS, et al. A case of xanthogranulomatous cholecystitis associated with Mirizzi syndrome. Korean J Gastroenterol. 1999; 34:136–141.8. Kim PN, Ha HK, Kim YH, Lee MG, Kim MH, Auh YH. US findings of xanthogranulomatous cholecystitis. Clin Radiol. 1998; 53:290–292.
Article9. Kim KH, Ahn CH, Kim JS, et al. Xanthogranulomatous cholecystitis mimicking gallbladder cancer. J Korean Surg Soc. 2002; 63:441–444.10. Lee HS, Joo KR, Kim DH, et al. A case of simultaneous xanthogranulomatous cholecystitis and carcinoma of the gallbladder. Korean J Intern Med. 2003; 18:53–56.
Article11. Houston JP, Sampson MA, Collins MC. Ultrasound diagnosis of gallbladder perforation in a case of xanthogranulomatous cholecystitis. Br J Radiol. 1989; 62:273–274.
Article12. Hsu C, Hurwitz JL, Schuss A, Katz DS. Radiology-pathology conference: xanthogranulomatous cholecystitis. Clin Imaging. 2003; 27:421–425.13. Khan SA, Gulfam , Anwer AW, Arshad Z, Hameed K, Shoaib M. Gallbladder perforation: a rare complication of acute cholecystitis. J Pak Med Assoc. 2010; 60:228–229.14. Darwin P, Goldberg E, Uradomo L. Jackson Pratt drain fluid-to-serum bilirubin concentration ratio for the diagnosis of bile leaks. Gastrointest Endosc. 2010; 71:99–104.
Article15. Runyon BA. Ascitic fluid bilirubin concentration as a key to choleperitoneum. J Clin Gastroenterol. 1987; 9:543–545.
Article16. Welsch T, von Frankenberg M, Schmidt J, Büchler MW. Diagnosis and definition of anastomotic leakage from the surgeon's perspective. Chirurg. 2011; 82:48–55.17. Antolovic D, Koch M, Galindo L, et al. Hepaticojejunostomy–an-alysis of risk factors for postoperative bile leaks and surgical complications. J Gastrointest Surg. 2007; 11:555–561.
Article