Intest Res.
2024 Apr;22(2):162-171. 10.5217/ir.2023.00090.
Sarcopenia is common in ulcerative colitis and correlates with disease activity
- Affiliations
-
- 1Department of Gastroenterology, Postgraduate Institute of Medical Education and Research, Chandigarh, India
- 2Department of Endocrinology, Postgraduate Institute of Medical Education and Research, Chandigarh, India
- 3Department of Radiodiagnosis, Postgraduate Institute of Medical Education and Research, Chandigarh, India
- 4Department of GI Surgery, HPB and Liver Transplantation, Postgraduate Institute of Medical Education and Research, Chandigarh, India
- 5Department of Histopathology, Postgraduate Institute of Medical Education and Research, Chandigarh, India
- KMID: 2554660
- DOI: http://doi.org/10.5217/ir.2023.00090
Abstract
- Background/Aims
Association of sarcopenia with disease severity in ulcerative colitis (UC) is not clearly defined. We planned to estimate the prevalence of sarcopenia in patients with UC as per the revised definition and its relation with the disease severity.
Methods
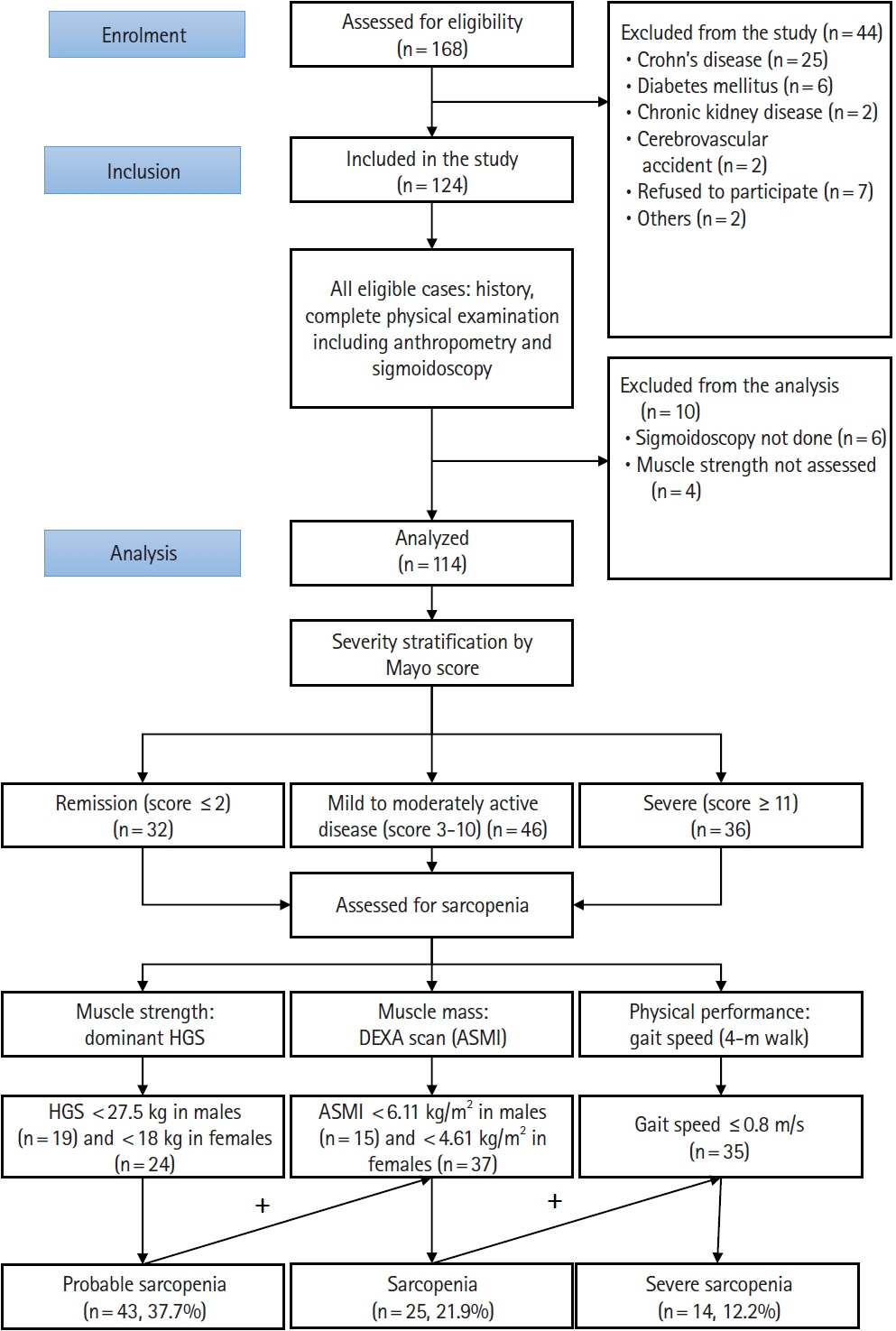
A cross-sectional assessment of sarcopenia in patients with UC was performed. Disease activity was graded according to complete Mayo score. Hand grip strength was assessed with Jamar hand dynamometer, muscle mass using a dual energy X-ray absorptiometry scan, and physical performance with 4-m walk test. Sarcopenia was defined as a reduction of both muscle mass and strength. Severe sarcopenia was defined as reduced gait speed in presence of sarcopenia.
Results
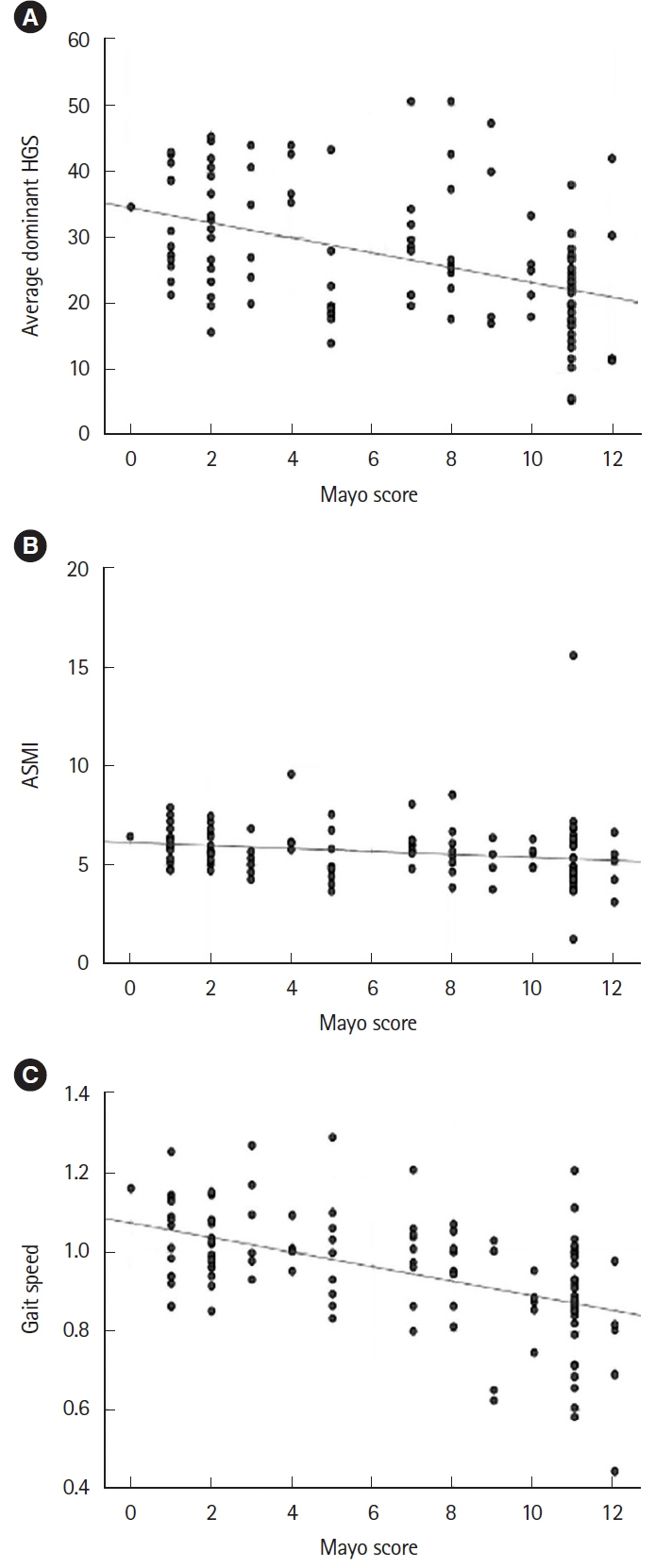
Of 114 patients (62 males, mean age: 36.49±12.41 years), 32 (28%) were in remission, 46 (40.4%) had mild-moderate activity, and 36 (31.6%) had severe UC. Forty-three patients (37.7%) had probable sarcopenia, 25 (21.9%) had sarcopenia, and 14 (12.2%) had severe sarcopenia. Prevalence of sarcopenia was higher in active disease (2 in remission, 6 in active, and 17 in severe, P<0.001). Of 14 with severe sarcopenia, 13 had severe UC while 1 had moderate UC. On multivariate analysis, lower body mass index and higher Mayo score were associated with sarcopenia. Of 37 patients with acute severe colitis, 16 had sarcopenia. Requirement of second-line therapy was similar between patients with and without sarcopenia. On follow-up (median: 18 months), there was a non-significant higher rate of major adverse events in those with sarcopenia (47.4% vs. 33.8%, P=0.273).
Conclusions
Sarcopenia and severe sarcopenia in UC correlate with the disease activity.
Keyword
Figure
Reference
-
1. Rosenberg IH. Sarcopenia: origins and clinical relevance. J Nutr. 1997; 127(5 Suppl):990S–991S.
Article2. Muscaritoli M, Anker SD, Argilés J, et al. Consensus definition of sarcopenia, cachexia and pre-cachexia: joint document elaborated by Special Interest Groups (SIG) “cachexia-anorexia in chronic wasting diseases” and “nutrition in geriatrics”. Clin Nutr. 2010; 29:154–159.
Article3. Fielding RA, Vellas B, Evans WJ, et al. Sarcopenia: an undiagnosed condition in older adults: current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc. 2011; 12:249–256.
Article4. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010; 39:412–423.5. Brämer GR. International statistical classification of diseases and related health problems: tenth revision. World Health Stat Q. 1988; 41:32–36.6. Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet. 2019; 393:2636–2646.
Article7. Nishikawa H, Nakamura S, Miyazaki T, et al. Inflammatory bowel disease and sarcopenia: its mechanism and clinical importance. J Clin Med. 2021; 10:4214.
Article8. Nardone OM, de Sire R, Petito V, et al. Inflammatory bowel diseases and sarcopenia: the role of inflammation and gut microbiota in the development of muscle failure. Front Immunol. 2021; 12:694217.
Article9. Singh A, Midha V, Mahajan R, et al. Evaluation of nutritional characteristics reveals similar prevalence of malnutrition in patients with ulcerative colitis and Crohn’s disease. Dig Dis Sci. 2023; 68:580–595.
Article10. Ryan E, McNicholas D, Creavin B, Kelly ME, Walsh T, Beddy D. Sarcopenia and inflammatory bowel disease: a systematic review. Inflamm Bowel Dis. 2019; 25:67–73.
Article11. Li S, Ney M, Eslamparast T, et al. Systematic review of nutrition screening and assessment in inflammatory bowel disease. World J Gastroenterol. 2019; 25:3823–3837.
Article12. Erős A, Soós A, Hegyi P, et al. Sarcopenia as an independent predictor of the surgical outcomes of patients with inflammatory bowel disease: a meta-analysis. Surg Today. 2020; 50:1138–1150.
Article13. Liu S, Ding X, Maggiore G, et al. Sarcopenia is associated with poor clinical outcomes in patients with inflammatory bowel disease: a prospective cohort study. Ann Transl Med. 2022; 10:367.
Article14. Harbord M, Eliakim R, Bettenworth D, et al. Third European evidence-based consensus on diagnosis and management of ulcerative colitis. Part 2: current management. J Crohns Colitis. 2017; 11:769–784.
Article15. Wani RT. Socioeconomic status scales-modified Kuppuswamy and Udai Pareekh’s scale updated for 2019. J Family Med Prim Care. 2019; 8:1846–1849.
Article16. Satsangi J, Silverberg MS, Vermeire S, Colombel JF. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut. 2006; 55:749–753.
Article17. Pal R, Aggarwal A, Singh T, et al. Diagnostic cut-offs, prevalence, and biochemical predictors of sarcopenia in healthy Indian adults: the Sarcopenia-Chandigarh Urban Bone Epidemiological Study (Sarco-CUBES). Eur Geriatr Med. 2020; 11:725–736.
Article18. Cruz-Jentoft AJ, Bahat G, Bauer J, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019; 48:601.
Article19. Schroeder KW, Tremaine WJ, Ilstrup DM. Coated oral 5-aminosalicylic acid therapy for mildly to moderately active ulcerative colitis: a randomized study. N Engl J Med. 1987; 317:1625–1629.
Article20. Truelove SC, Witts LJ. Cortisone in ulcerative colitis; final report on a therapeutic trial. Br Med J. 1955; 2:1041–1048.21. Bryant RV, Ooi S, Schultz CG, et al. Low muscle mass and sarcopenia: common and predictive of osteopenia in inflammatory bowel disease. Aliment Pharmacol Ther. 2015; 41:895–906.
Article22. Ünal NG, Oruç N, Tomey O, Ömer Özütemiz A. Malnutrition and sarcopenia are prevalent among inflammatory bowel disease patients with clinical remission. Eur J Gastroenterol Hepatol. 2021; 33:1367–1375.
Article23. Adams DW, Gurwara S, Silver HJ, et al. Sarcopenia is common in overweight patients with inflammatory bowel disease and may predict need for surgery. Inflamm Bowel Dis. 2017; 23:1182–1186.
Article24. Ge X, Xia J, Wu Y, et al. Sarcopenia assessed by computed tomography is associated with colectomy in patients with acute severe ulcerative colitis. Eur J Clin Nutr. 2022; 76:410–418.
Article25. Ge X, Jiang L, Yu W, et al. The importance of sarcopenia as a prognostic predictor of the clinical course in acute severe ulcerative colitis patients. Dig Liver Dis. 2021; 53:965–971.
Article26. Bamba S, Sasaki M, Takaoka A, et al. Sarcopenia is a predictive factor for intestinal resection in admitted patients with Crohn’s disease. PLoS One. 2017; 12:e0180036.
Article27. Cushing KC, Kordbacheh H, Gee MS, Kambadakone A, Ananthakrishnan AN. Sarcopenia is a novel predictor of the need for rescue therapy in hospitalized ulcerative colitis patients. J Crohns Colitis. 2018; 12:1036–1041.
Article28. Mishra S, Mandavdhare HS, Singh H, et al. Adjuvant use of combination of antibiotics in acute severe ulcerative colitis: a placebo controlled randomized trial. Expert Rev Anti Infect Ther. 2021; 19:949–955.
Article29. Ribeiro HS, Neri SG, Oliveira JS, Bennett PN, Viana JL, Lima RM. Association between sarcopenia and clinical outcomes in chronic kidney disease patients: a systematic review and meta-analysis. Clin Nutr. 2022; 41:1131–1140.
Article30. Tantai X, Liu Y, Yeo YH, et al. Effect of sarcopenia on survival in patients with cirrhosis: a meta-analysis. J Hepatol. 2022; 76:588–599.
Article31. Subramaniam K, Fallon K, Ruut T, et al. Infliximab reverses inflammatory muscle wasting (sarcopenia) in Crohn’s disease. Aliment Pharmacol Ther. 2015; 41:419–428.
Article32. Aswani-Omprakash T, Sharma V, Bishu S, et al. Addressing unmet needs from a new frontier of IBD: the South Asian IBD Alliance. Lancet Gastroenterol Hepatol. 2021; 6:884–885.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Nonischemic Central Retinal Vein Occlusion Developed in the course of Ulcerative Colits
- A Case of Cytomegalvirus Colitis Developed during the Treatment of Ulcerative Colitis
- A Case of Malignant Lymphoma in Patient with Ulcerative Colitis
- Trends in the incidence of ulcerative colitis in Korea
- A case of ulcerative colitis