Ann Surg Treat Res.
2024 Apr;106(4):211-217. 10.4174/astr.2024.106.4.211.
Fate of small remnant pancreatic tail in splenic hilum after laparoscopic spleen preserving distal pancreatectomy: a retrospective study
- Affiliations
-
- 1Division of Hepatobiliary-pancreatic Surgery, Department of Surgery, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea
- 2Division of Hepatobiliary-Pancreatic Surgery, Department of Surgery, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Korea
- 3Division of Hepatobiliary-Pancreatic Surgery, Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2554480
- DOI: http://doi.org/10.4174/astr.2024.106.4.211
Abstract
- Purpose
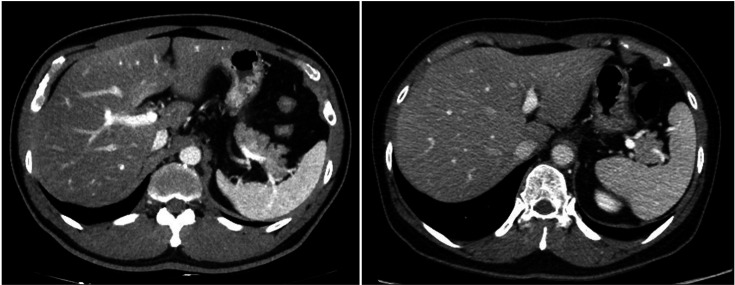
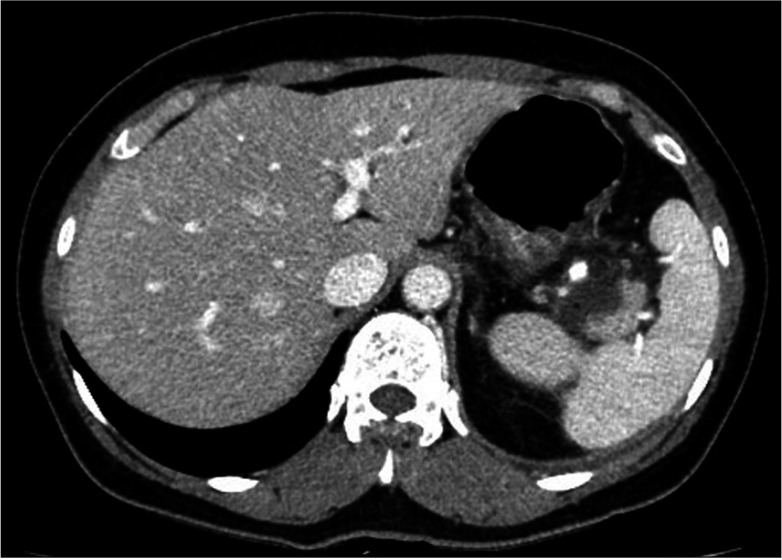
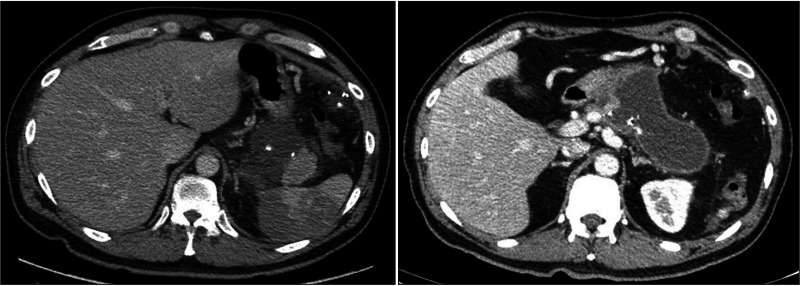
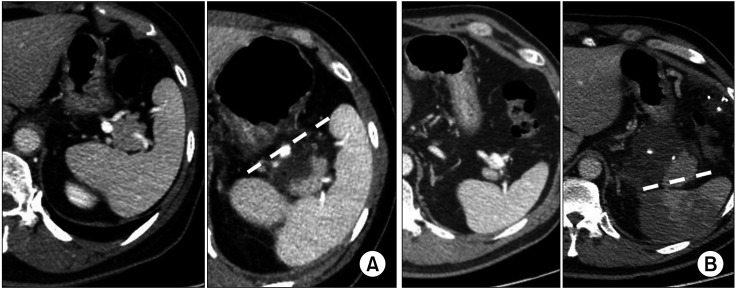
When performing laparoscopic spleen-preserving distal pancreatectomy (LSPDP), sometimes, anatomically challenging patients are encountered, where the pancreatic tail is deep in the splenic hilum. The purpose of this study was to discuss the experience with the surgical technique of leaving the deep pancreatic tail of the splenic hilum in these patients.
Methods
Eleven patients who underwent LSPDP with remnant pancreatic tails between November 2019 and August 2021 at Samsung Medical Center in Seoul, Korea were included in the study. Their short-term postoperative outcomes were analyzed retrospectively.
Results
The mean operative time was 168.6 ± 26.0 minutes, the estimated blood loss was 172.7 ± 95.8 mL, and the postoperative length of stay was 6.1 ± 1.0 days. All 11 lesions were in the body or tail of the pancreas and included 2 intraductal papillary mucinous neoplasms, 6 neuroendocrine tumors, 2 cystic neoplasms, and 1 patient with chronic pancreatitis. In 10 of the 11 patients, only the pancreatic tail was left inside the distal portion of the splenic hilum of the branching splenic vessel, and there was a collection of intraabdominal fluid, which was naturally resolved. One patient with a remnant pancreatic tail above the hilar vessels was readmitted due to a postoperative pancreatic fistula with fever and underwent internal drainage.
Conclusion
In spleen preservation, leaving a small pancreatic tail inside the splenic hilum is feasible and more beneficial to the patient than performing splenectomy in anatomically challenging patients.
Figure
Reference
-
1. Clark GJ, Onders RP, Knudson JD. Laparoscopic distal pancreatectomy procedures in a rural hospital. AORN J. 1997; 65:334–343. PMID: 9034442.2. Santoro E, Carlini M, Carboni F. Laparoscopic pancreatic surgery: indications, techniques and preliminary results. Hepatogastroenterology. 1999; 46:1174–1180. PMID: 10370687.3. Di Sabatino A, Carsetti R, Corazza GR. Post-splenectomy and hyposplenic states. Lancet. 2011; 378:86–97. PMID: 21474172.4. Meriglier E, Puyade M, Carretier M, Roblot F, Roblot P. Long-term infectious risks after splenectomy: a retrospective cohort study with up to 10 years follow-up. Rev Med Interne. 2017; 38:436–443. PMID: 28190612.5. Harji DP, Jaunoo SS, Mistry P, Nesargikar PN. Immunoprophylaxis in asplenic patients. Int J Surg. 2009; 7:421–423. PMID: 19607947.6. Rubin LG, Schaffner W. Clinical practice: care of the asplenic patient. N Engl J Med. 2014; 371:349–356. PMID: 25054718.7. Milito P, Aiolfi A, Asti E, Rausa E, Bonitta G, Bonavina L. Impact of spleen preserving laparoscopic distal pancreatectomy on postoperative infectious complications: systematic review and meta-analysis. J Laparoendosc Adv Surg Tech A. 2019; 29:167–177. PMID: 30592691.8. Tihanyi TF, Morvay K, Nehéz L, Winternitz T, Rusz Z, Flautner LE. Laparoscopic distal resection of the pancreas with the preservation of the spleen. Acta Chir Hung. 1997; 36:359–361. PMID: 9408401.9. Tang CW, Feng WM, Bao Y, Fei MY, Tao YL. Spleen-preserving distal pancreatectomy or distal pancreatectomy with splenectomy?: perioperative and patient-reported outcome analysis. J Clin Gastroenterol. 2014; 48:e62–e66. PMID: 24231937.10. Zhao YP, Du X, Dai MH, Zhang TP, Liao Q, Guo JC, et al. Laparoscopic distal pancreatectomy with or without splenectomy: spleen-preservation does not increase morbidity. Hepatobiliary Pancreat Dis Int. 2012; 11:536–541. PMID: 23060401.11. Kim EY, Choi HJ, You YK, Kim DG, Hong TH. Spleen-preserving distal pancreatectomy with vein scarifying and artery saving as an alternative for Warshaw method. J Gastrointest Surg. 2021; 25:1556–1558. PMID: 33037556.12. Kimura W, Yano M, Sugawara S, Okazaki S, Sato T, Moriya T, et al. Spleen-preserving distal pancreatectomy with conservation of the splenic artery and vein: techniques and its significance. J Hepatobiliary Pancreat Sci. 2010; 17:813–823. PMID: 20024588.13. Kim EY, You YK, Kim DG, Hong TH. Dual-incision laparoscopic spleen-preserving distal pancreatectomy: merits compared to the conventional method. J Gastrointest Surg. 2019; 23:1384–1391. PMID: 30367399.14. Di Mauro D, Gelsomino M, Fasano A, Wajed S, Manzelli A. Elective splenectomy in patients with non-Hodgkin lymphoma: does the size of the spleen affect surgical outcomes? Ann Hepatobiliary Pancreat Surg. 2022; 26:144–148. PMID: 35168206.15. Wayne M, Neragi-Miandoab S, Kasmin F, Brown W, Pahuja A, Cooperman AM. Central pancreatectomy without anastomosis. World J Surg Oncol. 2009; 7:67. PMID: 19719851.16. Warshaw AL. Distal pancreatectomy with preservation of the spleen. J Hepatobiliary Pancreat Sci. 2010; 17:808–812. PMID: 19882099.17. Melloul E, Lassen K, Roulin D, Grass F, Perinel J, Adham M, et al. Guidelines for perioperative care for pancreatoduodenectomy: Enhanced Recovery After Surgery (ERAS) Recommendations 2019. World J Surg. 2020; 44:2056–2084. PMID: 32161987.18. Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005; 138:8–13. PMID: 16003309.19. Govil S, Imrie CW. Value of splenic preservation during distal pancreatectomy for chronic pancreatitis. Br J Surg. 1999; 86:895–898. PMID: 10417561.20. Edgren G, Almqvist R, Hartman M, Utter GH. Splenectomy and the risk of sepsis: a population-based cohort study. Ann Surg. 2014; 260:1081–1087. PMID: 24374533.21. Bayrhuber M, Anka N, Camp J, Glattacker M, Farin E, Rieg S. Prevention of post-splenectomy sepsis in patients with asplenia: a study protocol of a controlled trial. BMC Infect Dis. 2020; 20:41. PMID: 31937251.22. Kashuk JL, Moore EE, Johnson JL, Biffl WL, Burlew CC, Barnett C, et al. Progressive postinjury thrombocytosis is associated with thromboembolic complications. Surgery. 2010; 148:667–675. PMID: 20719351.23. Kimura W, Inoue T, Futakawa N, Shinkai H, Han I, Muto T. Spleen-preserving distal pancreatectomy with conservation of the splenic artery and vein. Surgery. 1996; 120:885–890. PMID: 8909526.24. Elabbasy F, Gadde R, Hanna MM, Sleeman D, Livingstone A, Yakoub D. Minimally invasive spleen-preserving distal pancreatectomy: does splenic vessel preservation have better postoperative outcomes?: a systematic review and meta-analysis. Hepatobiliary Pancreat Dis Int. 2015; 14:346–353. PMID: 26256077.25. Korrel M, Lof S, Al Sarireh B, Björnsson B, Boggi U, Butturini G, et al. Short-term outcomes after spleen-preserving minimally invasive distal pancreatectomy with or without preservation of splenic vessels: a pan-European retrospective study in high-volume centers. Ann Surg. 2023; 277:e119–e125. PMID: 34091515.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic Spleen Preserving Distal Pancreatectomy with the Conservation of the Splenic Artery and the Vein
- Splenic vessel patency: is it real menace to perform laparoscopic splenic vessel-preserving distal pancreatectomy
- Dual-incision laparoscopic spleen-preserving distal pancreatectomy
- The First Experience of Robot Assisted Spleen-Preserving Laparoscopic Distal Pancreatectomy in Korea
- Safety and Efficacy of Laparoscopic Distal Pancreatectomy with Preservation of the Spleen and Splenic Vessels