J Cerebrovasc Endovasc Neurosurg.
2024 Mar;26(1):79-84. 10.7461/jcen.2023.E2022.12.001.
Spontaneous occlusion of a pial arteriovenous fistula after angiography: The role of iodinated contrast media
- Affiliations
-
- 1Department of Neurology and Neurointerventional Surgery, Neurological Institute, Cleveland Clinic, Abu Dhabi, United Arab Emirates
- 2School of Medicine, Queen’s University, Belfast, Ireland
- KMID: 2554050
- DOI: http://doi.org/10.7461/jcen.2023.E2022.12.001
Abstract
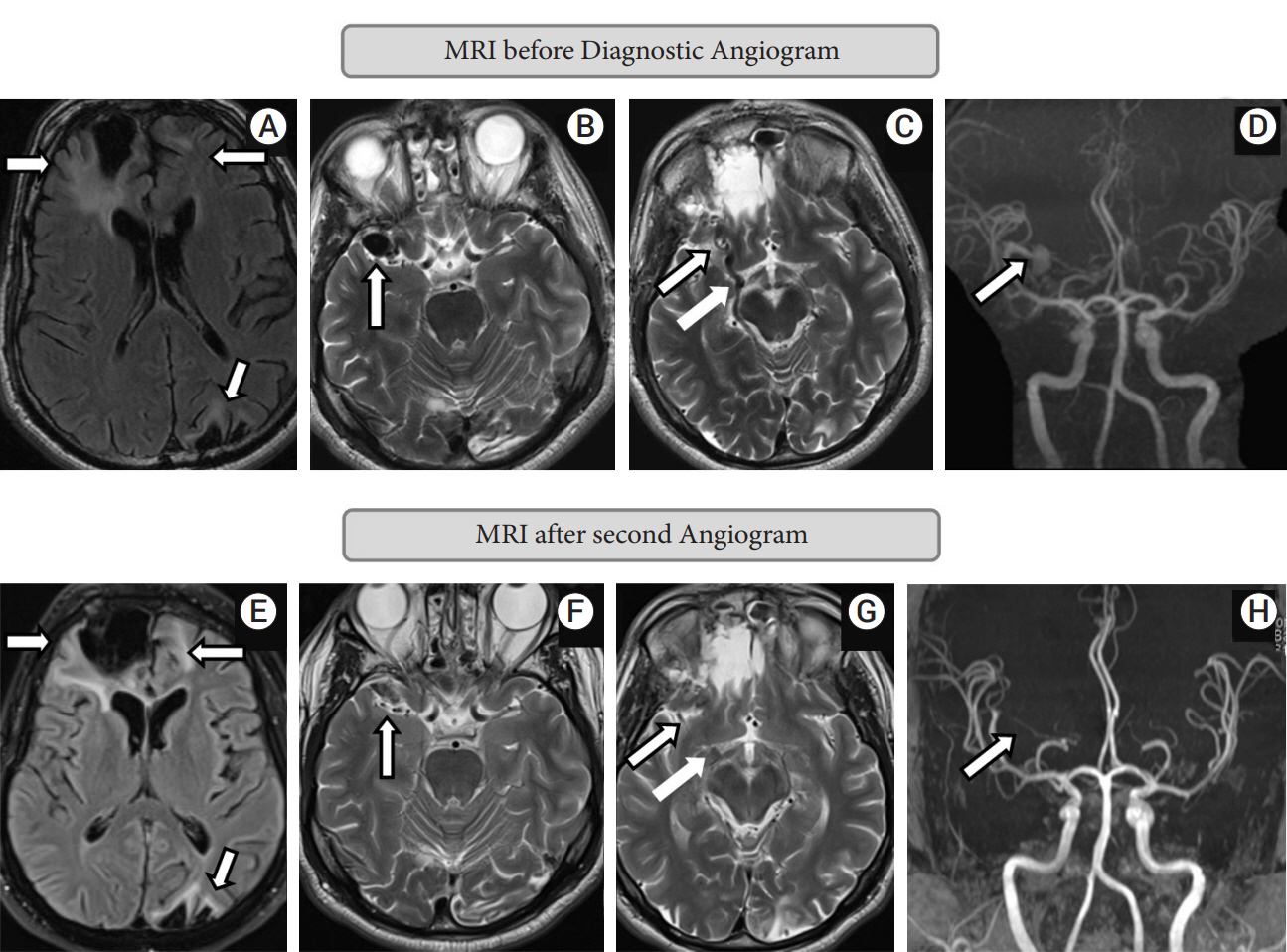
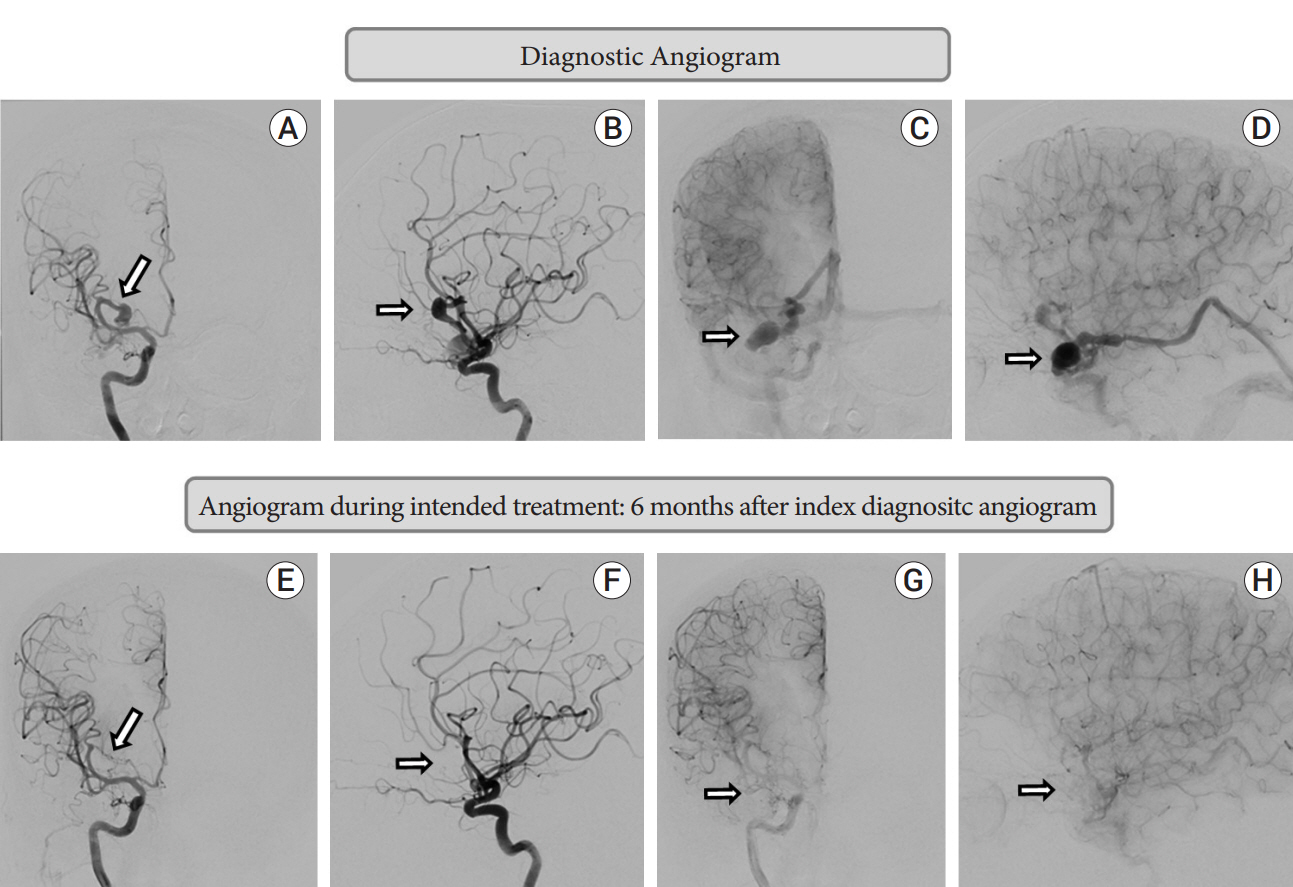
- Intracranial non-galenic pial arteriovenous fistula (PAVF) is an extremely rare vascular malformation, where one or more pial arteries feeds directly into a cortical vein without any intervening nidus. Though occasionally they can be asymptomatic, neurological symptoms such as headache, seizure, or focal neurological deficit are more common presenting features. Life threatening or fatal hemorrhage is not uncommon, hence needed to be treated more often than not. Spontaneous occlusion of PAVF is reported only four times before. We report a 49-year-old gentleman, who was diagnosed to have a PAVF, possibly secondary to trauma. He presented 5 months and 22 days from initial digital subtraction angiography (DSA) for treatment, and follow-up angiogram showed complete obliteration. He denied any significant event, medication or alternate treatment during this period. His clinical symptoms were stable as well. We postulate iodinated contrast medium induced vasculopathy as a possible cause, which has been described for other vascular pathologies, but never for PAVF.
Keyword
Figure
Reference
-
1. Chang CF, Liu XM, Peyton KJ, Durante W. Heme oxygenase-1 counteracts contrast media-induced endothelial cell dysfunction. Biochem Pharmacol. 2014; Jan. 87(2):303–11.
Article2. Franke RP, Fuhrmann R, Hiebl B, Jung F. Influence of radiographic contrast media (Iodixanol and Iomeprol) on the endothelin-1 release from human arterial and venous endothelial cells cultured on an extracellular matrix. Clin Hemorheol Microcirc. 2012; 52(2-4):229–34.
Article3. Halbach VV, Higashida RT, Hieshima GB, Hardin CW, Dowd CF, Barnwell SL. Transarterial occlusion of solitary intracerebral arteriovenous fistulas. AJNR Am J Neuroradiol. 1989; Jul-Aug. 10(4):747–52.4. Hoh BL, Putman CM, Budzik RF, Ogilvy CS. Surgical and endovascular flow disconnection of intracranial pial single-channel arteriovenous fistulae. Neurosurgery. 2001; Dec. 49(6):1351–63.
Article5. John S, Hussain SI, Elhammady MS, Navarro R, Zahra K. Multiple cranial dural and pial arteriovenous fistulas with occlusion of all after embolization of primary superior sagittal sinus dural fistula. World Neurosurg. 2020; Aug. 140:224–8.
Article6. Lyons MK, Hoxworth JM, McClendon J, Krishna CX, Patel NP. Spontaneous resolution of ruptured intracranial pial arteriovenous fistula following spinal surgery. Neuroradiol J. 2017; Apr. 30(2):175–9.
Article7. Medhi G, Gupta AK, Saini J, Ramalingaiah AH, Pendharkar H, Parida S. Pial arteriovenous fistula: A clinical and neuro-interventional experience of outcomes in a rare entity. Indian Journal of Radiology and Imaging. 2020; JulSep. 30(3):286–93.
Article8. Peeters SM, Colby GP, Guivatchian E, Sun MZ, Tateshima S, Wang AC. Spontaneous resolution of dural and pial arteriovenous fistulae arising after superficial temporal artery to middle cerebral artery bypass for moyamoya disease. World Neurosurg. 2020; Oct. 142:404–7.
Article9. Ren L, Wang P, Wang Z, Liu Y, Lv S. Hypotonic contrast media is more toxic than isotonic contrast media on endothelial cells in vivo and in vitro. Mol Med Rep. 2017; Oct. 16(4):4334–40.10. Ronda N, Potì F, Palmisano A, Gatti R, Orlandini G, Maggiore U, et al. Effects of the radiocontrast agent iodixanol on endothelial cell morphology and function. Vascul Pharmacol. 2013; Jan. 58(1-2):39–47.
Article11. Santosh C, Teasdale E, Molyneux A. Spontaneous closure of an intracranial middle cerebral arteriovenous fistula. Neuroradiology. 1991; 33(1):65–6.
Article12. Satow T, Suzuki M, Komuro T, Ogawa M, Kobayashi A, Nishida S. Spontaneous resolution of cerebral pial arteriovenous fistula after angiography: Report of two cases. World Neurosurg. 2017; Jul. 103:954.
Article13. Scoditti E, Massaro M, Montinari MR. Endothelial safety of radiological contrast media: Why being concerned. Vascul Pharmacol. 2013 ; Jan. 58(1-2):48–53.
Article14. Zhang B, Zhang Y, Liu B, Fang L, Li Y, Meng S. Iso-osmolar iodixanol induces less increase in circulating endothelial microparticles in vivo and less endothelial apoptosis in vitro compared with low-osmolar iohexol. Contrast Media Mol Imaging. 2018; Apr. 2018:8303609.15. Zhao Y, Tao Z, Xu Z, Tao Z, Chen B, Wang L, et al. Toxic effects of a high dose of non-ionic iodinated contrast media on renal glomerular and aortic endothelial cells in aged rats in vivo. Toxicol Lett. 2011; May. 202(3):253–60.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spontaneous Occlusion of Traumatic Carotid Cavernous Fistula with Pseudoaneurysm Formation-management with Neuroform Stent and Coiling: A Case Report
- Successful Treatment of Intracranial Small Pial Single-Channel Arteriovenous Fistula Using N-butyl Cyanoacrylate: Report of 2 Cases
- Embolization of Cerebral Pial Arteriovenous Fistula Under Balloon-assisted Flow Control Using NBCA: a Case Report
- Intracranial Pial Arteriovenous Fistula Presenting with Hemorrhage: A Case Report
- Cortical versus Pial Venous Drainage in Dural Arteriovenous Fistula