Ann Surg Treat Res.
2024 Mar;106(3):133-139. 10.4174/astr.2024.106.3.133.
Impact of COVID-19 infection during the postoperative period in patients who underwent gastrointestinal surgery: a retrospective study
- Affiliations
-
- 1Division of Colon and Rectal Surgery, Department of Surgery, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea
- KMID: 2553380
- DOI: http://doi.org/10.4174/astr.2024.106.3.133
Abstract
- Purpose
The coronavirus disease 2019 (COVID-19) pandemic has led to significant global casualties. This study examines the postoperative impact of COVID-19 on patients who underwent gastrointestinal surgery, considering their heightened vulnerability to infections and increased morbidity and mortality risk.
Methods
This retrospective observational study was conducted at a tertiary center and patients who underwent gastrointestinal surgery between January 2022 and February 2023 were included. Postoperative COVID-19 infection was defined as the detection of severe acute respiratory syndrome coronavirus 2 RNA by RT-PCR within 14 days after surgery. Propensity score matching was performed including age, sex, American Society of Anesthesiology physical status classification, and emergency operation between the COVID-19-negative (–) and -positive (+) groups.
Results
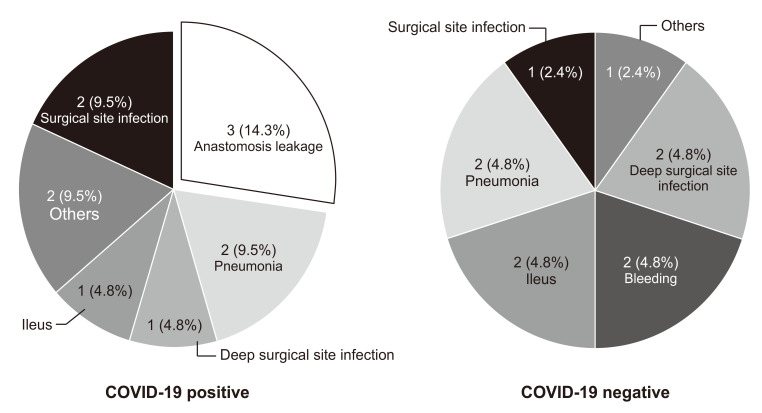
Following 1:2 propensity score matching, 21 COVID-19(+) and 42 COVID-19(–) patients were included in the study. In the COVID-19(+) group, the postoperative complication rate was significantly higher (52.4% vs. 23.8%, P = 0.023). Mechanical ventilator requirement, intensive care unit (ICU) admission, and readmission rate did not significantly differ between the 2 groups. The median length of ICU (19 days vs. 4 days, P < 0.001) and hospital stay (18 vs. 8 days, P = 0.015) were significantly longer in the COVID-19(+) group. Patients with COVID-19 had a 2.4 times higher relative risk (RR) of major complications than patients without COVID-19 (RR, 2.37; 95% confidence interval, 1.254–4.467; P = 0.015).
Conclusion
COVID-19 infection during the postoperative period in gastrointestinal surgery may have adverse outcomes which may increase the risk of major complications. Preoperative COVID-19 screening and protocols for COVID-19 prevention in surgical patients should be maintained.
Keyword
Figure
Reference
-
1. World Health Organization (WHO). WHO COVID-19 dashboard [Internet]. WHO;2020. cited 2023 Jul 8. Available from: https://covid19.who.int/ .2. Matta S, Chopra KK, Arora VK. Morbidity and mortality trends of Covid 19 in top 10 countries. Indian J Tuberc. 2020; 67:S167–S172. PMID: 33308665.3. Zhou W, Tang B, Bai Y, Shao Y, Xiao Y, Tang S. The resurgence risk of COVID-19 in China in the presence of immunity waning and ADE: a mathemat ical modelling study. Vaccine. 2022; 40:7141–7150. PMID: 36328883.4. Alazawi W, Pirmadjid N, Lahiri R, Bhattacharya S. Inf lammatory and immune responses to surgery and their clinical impact. Ann Surg. 2016; 264:73–80. PMID: 27275778.5. Dąbrowska AM, Słotwiński R. The immune response to surgery and infection. Cent Eur J Immunol. 2014; 39:532–537. PMID: 26155175.6. Inzunza M, Romero C, Irarrázaval MJ, Ruiz-Esquide M, Achurra P, Quezada N, et al. Morbidity and mortality in patients with perioperative COVID-19 infection: prospective cohort in general, gastroesophagic, hepatobiliary, and colorectal surgery. World J Surg. 2021; 45:1652–1662. PMID: 33748925.7. Knisely A, Zhou ZN, Wu J, Huang Y, Holcomb K, Melamed A, et al. Perioperative morbidity and mortality of patients with COVID-19 who undergo urgent and emergent surgical procedures. Ann Surg. 2021; 273:34–40. PMID: 33074900.8. Aziz H, Filkins A, Kwon YK. Review of COVID-19 outcomes in surgical patients. Am Surg. 2020; 86:741–745. PMID: 32683945.9. COVIDSurg Collaborative. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020; 396:27–38. PMID: 32479829.10. Doglietto F, Vezzoli M, Gheza F, Lussardi GL, Domenicucci M, Vecchiarelli L, et al. Factors associated with surgical mortality and complications among patients with and without coronavirus disease 2019 (COVID-19) in Italy. JAMA Surg. 2020; 155:691–702. PMID: 32530453.11. Rojas-Machado SA, Romero-Simó M, Arroyo A, Rojas-Machado A, López J, Calpena R. Prediction of anastomotic leak in colorectal cancer surgery based on a new prognostic index PROCOLE (prognostic colorectal leakage) developed from the meta-analysis of observational studies of risk factors. Int J Colorectal Dis. 2016; 31:197–210. PMID: 26507962.12. Patel S, Parikh C, Verma D, Sundararajan R, Agrawal U, Bheemisetty N, et al. Bowel ischemia in COVID-19: a systematic review. Int J Clin Pract. 2021; 75:e14930. PMID: 34605117.13. National Institutes of Health (NIH). COVID-19 treatment guidelines [Internet]. NIH;2023. cited 2023 Jul 8. Available from: https://www.covid19treatmentguidelines.nih.gov/ .14. COVIDSurg Collaborative. Outcomes from elective colorectal cancer surgery during the SARS-CoV-2 pandemic. Colorectal Dis. 2020; 11. 15. 23:732–749. PMID: 33191669.15. Eklöv K, Nygren J, Bringman S, Löfgren J, Sjövall A, Nordenvall C, et al. Trends in treatment of colorectal cancer and short-term outcomes during the first wave of the COVID-19 pandemic in Sweden. JAMA Netw Open. 2022; 5:e2211065. PMID: 35532933.16. Morris EJ, Goldacre R, Spata E, Mafham M, Finan PJ, Shelton J, et al. Impact of the COVID-19 pandemic on the detection and management of colorectal cancer in England: a population-based study. Lancet Gastroenterol Hepatol. 2021; 6:199–208. PMID: 33453763.17. Okuyan GÇ, Yıldırım M. The effect of the COVID-19 pandemic on the outcomes of surgically treated colorectal diseases: a retrospective cohort study. Ann Surg Treat Res. 2022; 103:104–111. PMID: 36017140.18. Ma C, Cong Y, Zhang H. COVID-19 and the digestive system. Am J Gastroenterol. 2020; 115:1003–1006. PMID: 32618648.19. Galanopoulos M, Gkeros F, Doukatas A, Karianakis G, Pontas C, Tsoukalas N, et al. COVID-19 pandemic: pathophysiology and manifestations from the gastrointestinal tract. World J Gastroenterol. 2020; 26:4579–4588. PMID: 32884218.20. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020; 323:1061–1069. PMID: 32031570.21. Liu Q, Wang RS, Qu GQ, Wang YY, Liu P, Zhu YZ, et al. Gross examination report of a COVID-19 death autopsy. Fa Yi Xue Za Zhi. 2020; 36:21–23. PMID: 32198987.22. Xiao F, Tang M, Zheng X, Liu Y, Li XH. Evidence for gastrointestinal infection of SARS-CoV-2. gastroenterology. 2020; 158:1831–1833. PMID: 32142773.23. Carvalho A, Alqusairi R, Adams A, Paul M, Kothari N, Peters S, et al. SARS-CoV-2 gastrointestinal infection causing hemorrhagic colitis: implications for detection and transmission of COVID-19 disease. Am J Gastroenterol. 2020; 115:942–946. PMID: 32496741.24. Hwabejire JO, Kaafarani HM, Mashbari H, Misdraji J, Fagenholz PJ, Gartland RM, et al. Bowel ischemia in COVID-19 infection: one-year surgical experience. Am Surg. 2021; 87:1893–1900. PMID: 34772281.25. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020; 395:497–506. PMID: 31986264.26. Zhang H, Kang Z, Gong H, Xu D, Wang J, Li Z, et al. The digestive system is a potential route of 2019-nCov infection: a bioinformatics analysis based on single-cell transcriptomes [Preprint]. BioRxiv. 2020; 01. 31. Available from: . DOI: 10.1101/2020.01.30.927806.27. Hamming I, Timens W, Bulthuis ML, Lely AT, Navis G, van Goor H. Tissue distribut ion of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004; 203:631–637. PMID: 15141377.28. COVIDSurg Collaborative. Delaying surgery for patients with a previous SARS-CoV-2 infection. Br J Surg. 2020; 107:e601–e602. PMID: 32974904.29. Tian D, Sun Y, Xu H, Ye Q. The emergence and epidemic characteristics of the highly mutated SARS-CoV-2 Omicron variant. J Med Virol. 2022; 94:2376–2383. PMID: 35118687.30. Sutton D, Fuchs K, D'Alton M, Goffman D. Universal screening for SARS-CoV-2 in women admitted for delivery. N Engl J Med. 2020; 382:2163–2164. PMID: 32283004.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The impact of preoperative coronavirus disease 19 infection on early postoperative mortality during the vaccination era: a nationwide retrospective cohort study
- The impact of the COVID-19 pandemic on in-hospital mortality in patients admitted through the emergency department
- COVID-19 Rapid Antigen Test: Role in Screening Prior to Gastrointestinal Endoscopy
- Mortality Rate and Outcomes of Omicron Variant Positive Patients with Osteoporotic Fractures: A Retrospective Study
- Intracranial Hypertension after COVID-19 Infection