Ann Surg Treat Res.
2024 Feb;106(2):93-105. 10.4174/astr.2024.106.2.93.
Short-term and long-term oncologic outcomes of self-expandable metallic stent compared with tube decompression for obstructive colorectal cancer: a systematic review and meta-analysis
- Affiliations
-
- 1Research Institute of Clinical Medicine of Jeonbuk National University-Biomedical Research Institute of Jeonbuk National University Hospital, Jeonju, Korea
- KMID: 2552390
- DOI: http://doi.org/10.4174/astr.2024.106.2.93
Abstract
- Purpose
Patients with obstructive colorectal cancer managed by emergency surgery show high morbidity, mortality, and stoma formation rates. Decompression modalities, including the self-expandable metallic stent (SEMS) and tube drainage (TD), have been used to improve surgical outcomes. However, there have been limited studies comparing the 2 modalities. We performed a meta-analysis on short- and long-term outcomes between SEMS and TD.
Methods
PubMed, EMBASE, Cochrane Library, and Google Scholar were searched. Data were pooled, and the overall effect size was calculated using random effect models. Outcome measures were perioperative short-term and 3-year survival outcomes.
Results
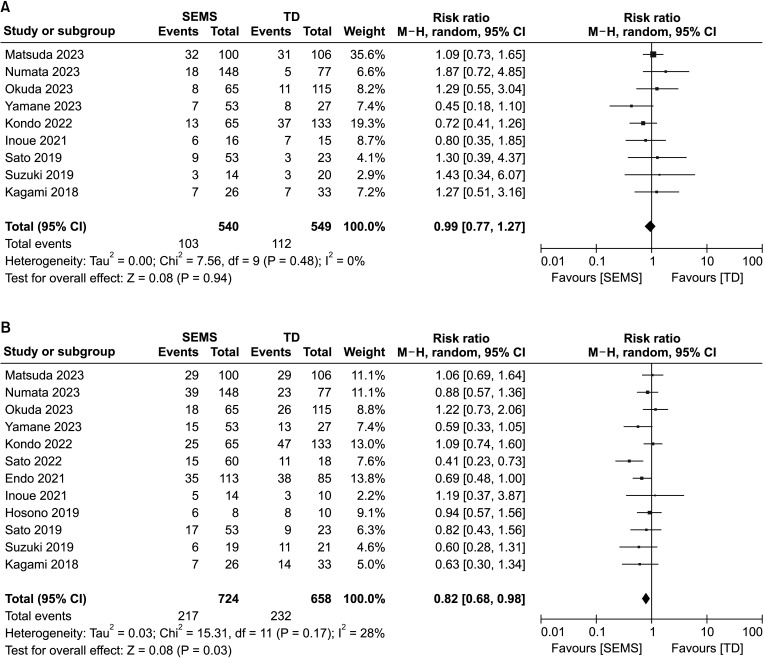
We included 20 nonrandomized studies that examined 2,047 patients in the meta-analysis. The meta-analysis showed SEMS had better short-term outcomes in clinical success rate, decompression-related complications, laparoscopic surgery rate, stoma formation rate, and postoperative complication rate with a relative risk (RR) of 0.36 (95% confidence interval [CI], 0.24–0.54; I2 = 20%), 0.32 (95% CI, 0.20–0.50; I 2 = 0%), 0.47 (95% CI, 0.34–0.66; I2 = 87%), 0.34 (95% CI, 0.24–0.49; I2 = 52%), and 0.70 (95% CI, 0.54–0.89, I2 = 28%), respectively. However, there was no significant difference between the 2 groups in 3-year overall survival (RR, 0.99; 95% CI, 0.77–1.27; I2 = 0%).
Conclusion
Although the long-term oncologic impact of SEMS is still unclear compared with TD, the results of this metaanalysis may suggest that SEMS insertion can be performed more successfully and safely and may have benefits for shortterm perioperative outcomes compared with TD. Further studies are warranted to provide more definitive survival results.
Figure
Reference
-
1. McArdle CS, McMillan DC, Hole DJ. The impact of blood loss, obstruction and perforation on survival in patients undergoing curative resection for colon cancer. Br J Surg. 2006; 93:483–488. PMID: 16555262.2. Yeo HL, Lee SW. Colorectal emergencies: review and controversies in the management of large bowel obstruction. J Gastrointest Surg. 2013; 17:2007–2012. PMID: 24048614.3. Zorcolo L, Covotta L, Carlomagno N, Bartolo DC. Safety of primary anastomosis in emergency colo-rectal surgery. Colorectal Dis. 2003; 5:262–269. PMID: 12780890.4. Tekkis PP, Kinsman R, Thompson MR, Stamatakis JD. Association of Coloproctology of Great Britain, Ireland. The Association of Coloproctology of Great Britain and Ireland study of large bowel obstruction caused by colorectal cancer. Ann Surg. 2004; 240:76–81. PMID: 15213621.5. Arezzo A, Forcignanò E, Bonino MA, Balagué C, Targarona E, Borghi F, et al. Long-term oncologic results after stenting as a bridge to surgery versus emergency surgery for malignant left-sided colonic obstruction: a multicenter randomized controlled trial (ESCO Trial). Ann Surg. 2020; 272:703–708. PMID: 32833762.6. CReST Collaborative Group. Colorectal Endoscopic Stenting Trial (CReST) for obstructing left-sided colorectal cancer: randomized clinical trial. Br J Surg. 2022; 109:1073–1080. PMID: 35986684.7. Shingu Y, Hasegawa H, Sakamoto E, Komatsu S, Kurumiya Y, Norimizu S, et al. Clinical and oncologic safety of laparoscopic surgery for obstructive left colorectal cancer following transanal endoscopic tube decompression. Surg Endosc. 2013; 27:3359–3363. PMID: 23549762.8. Shigeta K, Baba H, Yamafuji K, Kaneda H, Katsura H, Kubochi K. Outcomes for patients with obstructing colorectal cancers treated with one-stage surgery using transanal drainage tubes. J Gastrointest Surg. 2014; 18:1507–1513. PMID: 24871080.9. Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009; 151:264–269. W64PMID: 19622511.10. Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. Version 5.1.0, vol. 5. Wiley;2011.11. Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses [Internet]. Ottawa Hospital Research Institute;c2021. cited 2023 Nov 1. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp .12. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327:557–560. PMID: 12958120.13. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986; 7:177–188. PMID: 3802833.14. Thabane L, Akhtar-Danesh N. Guidelines for reporting descriptive statistics in health research. Nurse Res. 2008; 15:72–81.15. Patsopoulos NA, Evangelou E, Ioannidis JP. Sensitivity of between-study heterogeneity in meta-analysis: proposed metrics and empirical evaluation. Int J Epidemiol. 2008; 37:1148–1157. PMID: 18424475.16. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997; 315:629–634. PMID: 9310563.17. Sutton AJ, Duval SJ, Tweedie RL, Abrams KR, Jones DR. Empirical assessment of effect of publication bias on meta-analyses. BMJ. 2000; 320:1574–1577. PMID: 10845965.18. Matsuda A, Yamada T, Yokoyama Y, Takahashi G, Yoshida H. Long-term outcomes between self-expandable metallic stent and transanal decompression tube for malignant large bowel obstruction: a multicenter retrospective study and meta-analysis. Ann Gastroenterol Surg. 2023; 7:583–593. PMID: 37416739.19. Numata K, Numata M, Shirai J, Sawazaki S, Okamoto H, Godai T, et al. Short- and long-term outcomes of transanal decompression tube and self-expandable metallic stent for obstructive colorectal cancer based on a multicenter database (KYCC2110). J Surg Oncol. 2023; 128:1372–1379. PMID: 37753717.20. Okuda Y, Shimura T, Uno K, Yamada T, Nukui T, Mizushima T, et al. A multicenter case-control study of self-expanding metallic stent versus transanal colorectal tube for stage II/III non-right-sided obstructive colon cancer. J Gastroenterol. 2023; 58:217–228. PMID: 36629947.21. Yamane K, Umino Y, Nagami T, Tarumoto K, Hattori K, Maemoto R, et al. Comparison of oncological and perioperative outcomes between self-expanding metal stents and decompression tubes for stages II and III obstructive colorectal cancer: a retrospective observational study. World J Surg. 2023; 47:2279–2286. PMID: 37184666.22. Kondo A, Kumamoto K, Kobara H, Nagahara T, Wato M, Shibatoge M, et al. Outcomes of patients with left-sided obstructive colorectal cancer: comparison between self-expandable metallic stent and other treatment methods. Dig Surg. 2022; 39:117–124. PMID: 35462370.23. Sato K, Imaizumi K, K asajima H, Kurushima M, Umehara M, Tsuruga Y, et al. Short- and long-term outcomes of a self-expandable metallic stent versus a transanal decompression tube for pathological stage II and III left-sided obstructive colorectal cancer: a retrospective observational study. Surg Today. 2022; 52:268–277. PMID: 34272601.24. Zhang S, Liu G, Wu GH, Zhang SW, Zhao YJ, Xu J. Transanal decompression tube is superior to self-expandable metallic colonic stent for malignant colorectal obstruction: a retrospective study. ANZ J Surg. 2022; 92:140–145. PMID: 34636468.25. Endo S, Kumamoto K, Enomoto T, Koizumi K, Kato H, Saida Y. Comparison of survival and perioperative outcome of the colonic stent and the transanal decompression tube placement and emergency surgery for left-sided obstructive colorectal cancer: a retrospective multi-center observational study “The CODOMO study”. Int J Colorectal Dis. 2021; 36:987–998. PMID: 33247313.26. Inoue H, Arita T, Kuriu Y, Shimizu H, Kiuchi J, Yamamoto Y, et al. Emergency management of obstructive colorectal cancer: a retrospective study of efficacy and safety in self-expanding metallic stents and trans-anal tubes. In Vivo. 2021; 35:2289–2296. PMID: 34182508.27. An Y, Wang N, Yang Z, Li Y, Xu B, Guo G, et al. Efficacy of transanal drainage tube and self-expanding metallic stent in acute left malignant colorectal obstruction. Ann Palliat Med. 2020; 9:1614–1621. PMID: 32692191.28. Xu YS, Fu YF, Li DC, Song T. Preoperative colonic decompression with decompression tube insertion versus stent insertion in patients with malignant left colonic obstruction. Surg Laparosc Endosc Percutan Tech. 2020; 30:183–186. PMID: 31318847.29. Hosono M, Matsuda T, Yamashita K, Hasegawa H, Yamamoto M, Kanaji S, et al. Successful single-stage laparoscopic surgery using a preoperative self-expanding metallic stent in patients with obstructive colorectal cancer. Asian J Endosc Surg. 2019; 12:401–407. PMID: 30411530.30. Sato R, Oikawa M, Kakita T, Okada T, Oyama A, Abe T, Yazawa T, Tsuchiya H, Akazawa N, Ohira T, Harada Y, Tanaka M, Okano H, Ito K, Tsuchiya T. Comparison of the long-term outcomes of the self-expandable metallic stent and transanal decompression tube for obstructive colorectal cancer. Ann Gastroenterol Surg. 2019; 3:209–216. PMID: 30923791.31. Suzuki Y, Moritani K, Seo Y, Takahashi T. Comparison of decompression tubes with metallic stents for the management of right-sided malignant colonic obstruction. World J Gastroenterol. 2019; 25:1975–1985. PMID: 31086465.32. Kagami S, Funahashi K, Ushigome M, Koike J, Kaneko T, Koda T, et al. Comparative study between colonic metallic stent and anal tube decompression for Japanese patients with left-sided malignant large bowel obstruction. World J Surg Oncol. 2018; 16:210. PMID: 30333034.33. Kawachi J, Kashiwagi H, Shimoyama R, Isogai N, Fukai R, Miyake K, et al. Comparison of efficacies of the self-expandable metallic stent versus transanal drainage tube and emergency surgery for malignant left-sided colon obstruction. Asian J Surg. 2018; 41:498–505. PMID: 28844781.34. Matsuda A, Miyashita M, Matsumoto S, Sakurazawa N, Takahashi G, Matsutani T, et al. Comparison between metallic stent and transanal decompression tube for malignant large-bowel obstruction. J Surg Res. 2016; 205:474–481. PMID: 27664898.35. Takeyama H, Kitani K, Wakasa T, Tsujie M, Fujiwara Y, Mizuno S, et al. Self-expanding metallic stent improves histopathologic edema compared with transanal drainage tube for malignant colorectal obstruction. Dig Endosc. 2016; 28:456–464. PMID: 26632261.36. Li CY, Guo SB, Wang NF. Decompression of acute left-sided malignant colorectal obstruction: comparing transanal drainage tube with metallic stent. J Clin Gastroenterol. 2014; 48:e37–e42. PMID: 24162168.37. Moroi R, Endo K, Ichikawa R, Nagai H, Shinkai H, Kimura T, et al. The effectiveness of self-expandable metallic stent insertion in treating right-sided colonic obstruction: a comparison between SEMS and decompression tube placement and an investigation of the safety and difficulties of SEMS insertion in right colons. Gastroenterol Res Pract. 2014; 2014:372918. PMID: 25580111.38. Ma W, Zhang JC, Luo K, Wang L, Zhang C, Cai B, et al. Self-expanding metal stents versus decompression tubes as a bridge to surgery for patients with obstruction caused by colorectal cancer: a systematic review and meta-analysis. World J Emerg Surg. 2023; 18:46. PMID: 37759264.39. Chen F, Dong Q, Zhang F. Is self-expandable metallic stents superior to transanal decompression tubes for the treatment of malignant large-bowel obstruction: a meta-analysis. Ann Palliat Med. 2021; 10:7378–7387. PMID: 34263636.40. Wang FG, Bai RX, Yan M, Song MM, Yan WM. Short-term outcomes of self-expandable metallic stent versus decompression tube for malignant colorectal obstruction: a meta-analysis of clinical data. J Invest Surg. 2020; 33:762–770. PMID: 30885015.41. Sloothaak DA, van den Berg MW, Dijkgraaf MG, Fockens P, Tanis PJ, van Hooft JE, et al. Oncological outcome of malignant colonic obstruction in the Dutch Stent-In 2 trial. Br J Surg. 2014; 101:1751–1757. PMID: 25298250.42. Takahashi G, Yamada T, Iwai T, Takeda K, Koizumi M, Shinji S, et al. Oncological assessment of stent placement for obstructive colorectal cancer from circulating cell-free DNA and circulating tumor DNA dynamics. Ann Surg Oncol. 2018; 25:737–744.43. Matsuda A, Miyashita M, Matsumoto S, Sakurazawa N, Kawano Y, Yamahatsu K, et al. Colonic stent-induced mechanical compression may suppress cancer cell proliferation in malignant large bowel obstruction. Surg Endosc. 2019; 33:1290–1297. PMID: 30171397.44. Matsuda Miyashita M, Matsumoto S, Sakurazawa N, Kawano Y, Yamada T, et al. Optimal interval from placement of a self-expandable metallic stent to surgery in patients with malignant large bowel obstruction: a preliminary study. Surg Laparosc Endosc Percutan Tech. 2018; 28:239–244. PMID: 29889691.45. Lawler J, Choynowski M, Bailey K, Bucholc M, Johnston A, Sugrue M. Meta-analysis of the impact of postoperative infective complications on oncological outcomes in colorectal cancer surgery. BJS Open. 2020; 4:737–747. PMID: 32525280.46. Ha GW, Kim JH, Lee MR. Oncologic impact of anastomotic leakage following colorectal cancer surgery: a systematic review and meta-analysis. Ann Surg Oncol. 2017; 24:3289–3299. PMID: 28608118.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Short-term Oncologic Outcome of Curative Resection for Obstructive Colorectal Cancer Followed by Stent Insertion: Comparative Study with Non-abstructive Colorectal Cancer
- Short-Term Outcome of Curative One-Stage Laparoscopic Resection for Obstructive Left-Sided Colon Cancers Followed by Stent Insertion: Comparative Study with Non-Obstructive Left-Sided Colon Cancers
- Percutaneous placement of self-expandable metallic stents in patients with obstructive jaundice due to hepatocellular carcinoma
- Oncological Safety of a Metallic Stent for a Left-sided Obstructive Colorectal Carcinoma
- Is stent insertion for obstructing colon cancer a good prognostic factor in long-term oncologic outcomes in symptomatic obstructive colon cancer?