Nutr Res Pract.
2024 Feb;18(1):98-109. 10.4162/nrp.2024.18.1.98.
The impact of probiotics and vitamin C on the prevention of upper respiratory tract symptoms in two preschool children cohorts
- Affiliations
-
- 1Institute of Medical Chemistry, Biochemistry and Clinical Biochemistry, Faculty of Medicine, Comenius University, 813 72 Bratislava, Slovakia
- 2JuvenaliaA Paediatric Centre, 929 01 Dunajská Streda, Slovakia
- 3Department of Clinical Sciences, Liverpool School of Tropical Medicine, Pembroke Place, Liverpool, L3 5QA, United Kingdom
- KMID: 2552286
- DOI: http://doi.org/10.4162/nrp.2024.18.1.98
Abstract
- BACKGROUND/OBJECTIVES
The efficacy of Lab4 probiotic and vitamin C combination on the prevention of upper respiratory tract infections (URTIs) was investigated in two studies with children. Our objective was to pool dataset of 57 preschool children from the PROCHILD study (ISRCTN28722693) and the dataset of 50 preschool matched cohort from the PROCHILD-2 study (ISRCTN26587549) to evaluate the impact of probiotic/vitamin C combination on the prevention of upper respiratory tract symptoms and provide a more robust assessment of effect using detailed individual level data.
SUBJECTS/METHODS
The children were supplemented daily for 6 months with either the multistrain probiotic (1.25×10 10 cfu/tablet consisting of two strains of Lactobacillus acidophilus CUL21 and CUL60, Bifidobacterium bifidum CUL20 and Bifidobacterium animalis subsp. lactis CUL34) plus 50 mg vitamin C or a placebo.
RESULTS
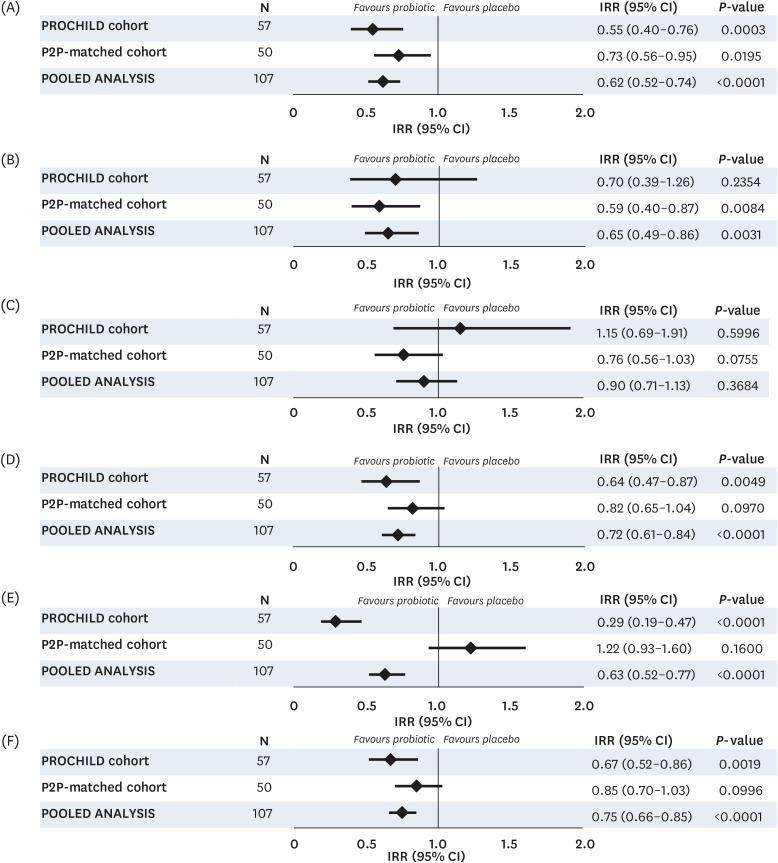
In the pooled analysis of the individual participant data (per protocol population), significant reductions were observed for the incidence (−25%; 95% confidence interval [CI], 0.66, 0.85; P < 0.0001) and duration (−14.9 days; 95% CI, −24.8, −5.1; P = 0.0030) of typical URTI symptoms in the active group compared with the placebo. The incidence rates of absenteeism from preschool (IR ratio, 0.75; 95% CI, 0.66, 0.86; P < 0.0001), paediatric visits (IR ratio, 0.56; 95% CI, 0.47; 0.68; P < 0.0001) and antibiotic usage (IR ratio, 0.53; 95% CI, 0.39, 0.71; P < 0.0001) were also significantly reduced.
CONCLUSION
The pooled analysis findings of comparable preschool cohorts from two studies indicate that the supplementation with probiotic and vitamin C combination is beneficial in the prevention and management of URTI symptoms.
Keyword
Figure
Reference
-
1. Sun Y, Sundell J. Early daycare attendance increase the risk for respiratory infections and asthma of children. J Asthma. 2011; 48:790–796. PMID: 21838620.2. Allan GM, Arroll B. Prevention and treatment of the common cold: making sense of the evidence. CMAJ. 2014; 186:190–199. PMID: 24468694.3. Gergova RT, Petrova G, Gergov S, Minchev P, Mitov I, Strateva T. Microbiological features of upper respiratory tract infections in Bulgarian children for the period 1998–2014. Balkan Med J. 2016; 33:675–680. PMID: 27994923.4. Jeseňák M, Mináriková D. Acute upper respiratory tract infections and its management. Prakt Lek. 2020; 10:63–70.5. Schot MJ, Dekker AR, van Werkhoven CH, van der Velden AW, Cals JW, Broekhuizen BD, Hopstaken RM, de Wit NJ, Verheij TJ. Burden of disease in children with respiratory tract infections in primary care: diary-based cohort study. Fam Pract. 2019; 36:723–729. PMID: 31166598.6. Fendrick AM, Monto AS, Nightengale B, Sarnes M. The economic burden of non-influenza-related viral respiratory tract infection in the United States. Arch Intern Med. 2003; 163:487–494. PMID: 12588210.7. Marengo RL, Ciceran A, Del Río Navarro BE. Upper respiratory tract infections in children and adults: Burden and management. A narrative summary of selected presentations that took place on 11th–12th May 2017, as part of the Encuentro Latinoamericano de Infecciones Respiratorias Recurrentes (ELAIR) educational event in Mexico City, Mexico. EMJ Respir. 2017; 5:22–28.8. Holstiege J, Schink T, Molokhia M, Mazzaglia G, Innocenti F, Oteri A, Bezemer I, Poluzzi E, Puccini A, Ulrichsen SP, et al. Systemic antibiotic prescribing to paediatric outpatients in 5 European countries: a population-based cohort study. BMC Pediatr. 2014; 14:174. PMID: 24997585.9. World Health Organization. Antibiotic resistance [Internet]. Geneva: World Health Organization;2020. cited 2023 September 25. Available from: https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance.10. Sencio V, Machado MG, Trottein F. The lung-gut axis during viral respiratory infections: the impact of gut dysbiosis on secondary disease outcomes. Mucosal Immunol. 2021; 14:296–304. PMID: 33500564.11. Cruz CS, Ricci MF, Vieira AT. Gut microbiota modulation as a potential target for the treatment of lung infections. Front Pharmacol. 2021; 12:724033. PMID: 34557097.12. Yang M, Yang Y, He Q, Zhu P, Liu M, Xu J, Zhao M. Intestinal microbiota-a promising target for antiviral therapy? Front Immunol. 2021; 12:676232. PMID: 34054866.13. Hill C, Guarner F, Reid G, Gibson GR, Merenstein DJ, Pot B, Morelli L, Canani RB, Flint HJ, Salminen S, et al. Expert consensus document. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol. 2014; 11:506–514. PMID: 24912386.14. Zhao Y, Dong BR, Hao Q. Probiotics for preventing acute upper respiratory tract infections. Cochrane Database Syst Rev. 2022; 8:CD006895. PMID: 36001877.15. King S, Tancredi D, Lenoir-Wijnkoop I, Gould K, Vann H, Connors G, Sanders ME, Linder JA, Shane AL, Merenstein D. Does probiotic consumption reduce antibiotic utilization for common acute infections? A systematic review and meta-analysis. Eur J Public Health. 2019; 29:494–499. PMID: 30219897.16. Hemilä H, Chalker E. Vitamin C for preventing and treating the common cold. Cochrane Database Syst Rev. 2013; 2013:CD000980. PMID: 23440782.17. Garaiova I, Muchová J, Nagyová Z, Wang D, Li JV, Országhová Z, Michael DR, Plummer SF, Ďuračková Z. Probiotics and vitamin C for the prevention of respiratory tract infections in children attending preschool: a randomised controlled pilot study. Eur J Clin Nutr. 2015; 69:373–379. PMID: 25205320.18. Garaiova I, Paduchová Z, Nagyová Z, Wang D, Michael DR, Plummer SF, Marchesi JR, Ďuračková Z, Muchová J. Probiotics with vitamin C for the prevention of upper respiratory tract symptoms in children aged 3–10 years: randomised controlled trial. Benef Microbes. 2021; 12:431–440. PMID: 34511049.19. Garaiova I, Paduchová Z, Nagyová Z, Wang D, Michael DR, Plummer SF, Marchesi JR, Ďuračková Z, Muchová J. Probiotics with low dose vitamin C reduce antibiotic prescriptions in children: a secondary analysis of a multicentre randomised double-blind placebo-controlled trial. J Funct Foods. 2023; 106:105625.20. Marteau P, Guyonnet D, Lafaye de Micheaux P, Gelu S. A randomized, double-blind, controlled study and pooled analysis of two identical trials of fermented milk containing probiotic Bifidobacterium lactis CNCM I-2494 in healthy women reporting minor digestive symptoms. Neurogastroenterol Motil. 2013; 25:331–e252. PMID: 23480238.21. Williams EA, Stimpson J, Wang D, Plummer S, Garaiova I, Barker ME, Corfe BM. Clinical trial: a multistrain probiotic preparation significantly reduces symptoms of irritable bowel syndrome in a double-blind placebo-controlled study. Aliment Pharmacol Ther. 2009; 29:97–103. PMID: 18785988.22. Plummer SF, Garaiova I, Sarvotham T, Cottrell SL, Le Scouiller S, Weaver MA, Tang J, Dee P, Hunter J. Effects of probiotics on the composition of the intestinal microbiota following antibiotic therapy. Int J Antimicrob Agents. 2005; 26:69–74. PMID: 15967639.23. Madden JA, Plummer SF, Tang J, Garaiova I, Plummer NT, Herbison M, Hunter JO, Shimada T, Cheng L, Shirakawa T. Effect of probiotics on preventing disruption of the intestinal microflora following antibiotic therapy: a double-blind, placebo-controlled pilot study. Int Immunopharmacol. 2005; 5:1091–1097. PMID: 15829425.24. Plummer S, Weaver MA, Harris JC, Dee P, Hunter J. Clostridium difficile pilot study: effects of probiotic supplementation on the incidence of C. difficile diarrhoea. Int Microbiol. 2004; 7:59–62. PMID: 15179608.25. Hepburn NJ, Garaiova I, Williams EA, Michael DR, Plummer S. Probiotic supplement consumption alters cytokine production from peripheral blood mononuclear cells: a preliminary study using healthy individuals. Benef Microbes. 2013; 4:313–317. PMID: 24311314.26. King S, Glanville J, Sanders ME, Fitzgerald A, Varley D. Effectiveness of probiotics on the duration of illness in healthy children and adults who develop common acute respiratory infectious conditions: a systematic review and meta-analysis. Br J Nutr. 2014; 112:41–54. PMID: 24780623.27. Laursen RP, Hojsak I. Probiotics for respiratory tract infections in children attending day care centers-a systematic review. Eur J Pediatr. 2018; 177:979–994. PMID: 29752587.28. Hatakka K, Savilahti E, Pönkä A, Meurman JH, Poussa T, Näse L, Saxelin M, Korpela R. Effect of long term consumption of probiotic milk on infections in children attending day care centres: double blind, randomised trial. BMJ. 2001; 322:1327. PMID: 11387176.29. Hojsak I, Snovak N, Abdović S, Szajewska H, Misak Z, Kolacek S. Lactobacillus GG in the prevention of gastrointestinal and respiratory tract infections in children who attend day care centers: a randomized, double-blind, placebo-controlled trial. Clin Nutr. 2010; 29:312–316. PMID: 19896252.30. Kumpu M, Lehtoranta L, Roivainen M, Rönkkö E, Ziegler T, Söderlund-Venermo M, Kautiainen H, Järvenpää S, Kekkonen R, Hatakka K, et al. The use of the probiotic Lactobacillus rhamnosus GG and viral findings in the nasopharynx of children attending day care. J Med Virol. 2013; 85:1632–1638. PMID: 23794458.31. Merenstein D, Murphy M, Fokar A, Hernandez RK, Park H, Nsouli H, Sanders ME, Davis BA, Niborski V, Tondu F, et al. Use of a fermented dairy probiotic drink containing Lactobacillus casei (DN-114 001) to decrease the rate of illness in kids: the DRINK study. A patient-oriented, double-blind, cluster-randomized, placebo-controlled, clinical trial. Eur J Clin Nutr. 2010; 64:669–677. PMID: 20485304.32. Prodeus A, Niborski V, Schrezenmeir J, Gorelov A, Shcherbina A, Rumyantsev A. Fermented milk consumption and common infections in children attending day-care centers: a randomized trial. J Pediatr Gastroenterol Nutr. 2016; 63:534–543. PMID: 27168455.33. Leyer GJ, Li S, Mubasher ME, Reifer C, Ouwehand AC. Probiotic effects on cold and influenza-like symptom incidence and duration in children. Pediatrics. 2009; 124:e172–e179. PMID: 19651563.34. Lau AS, Yanagisawa N, Hor YY, Lew LC, Ong JS, Chuah LO, Lee YY, Choi SB, Rashid F, Wahid N, et al. Bifidobacterium longum BB536 alleviated upper respiratory illnesses and modulated gut microbiota profiles in Malaysian pre-school children. Benef Microbes. 2018; 9:61–70. PMID: 29065707.35. Caceres P, Montes S, Vega N, Cruchet S, Brunser O, Gotteland M. Effects of Lactobacillus rhamnosus HN001on acute respiratory infections and intestinal secretory IgA in children. J Pediatr Infect Dis. 2010; 5:353–362.36. Hojsak I, Močić Pavić A, Kos T, Dumančić J, Kolaček S. Bifidobacterium animalis subsp. lactis in prevention of common infections in healthy children attending day care centers - randomized, double blind, placebo-controlled study. Clin Nutr. 2016; 35:587–591. PMID: 26031908.37. Lazou Ahrén I, Berggren A, Teixeira C, Martinsson Niskanen T, Larsson N. Evaluation of the efficacy of Lactobacillus plantarum HEAL9 and Lactobacillus paracasei 8700:2 on aspects of common cold infections in children attending day care: a randomised, double-blind, placebo-controlled clinical study. Eur J Nutr. 2020; 59:409–417. PMID: 31734734.38. Damholt A, Keller MK, Baranowski K, Brown B, Wichmann A, Melsaether C, Eskesen D, Westphal V, Arltoft D, Habicht A, et al. Lacticaseibacillus rhamnosus GG DSM 33156 effects on pathogen defence in the upper respiratory tract: a randomised, double-blind, placebo-controlled paediatric trial. Benef Microbes. 2022; 13:13–23. PMID: 34895109.39. Hay AD, Anderson E, Ingle S, Beck C, Hollingworth W. Respiratory tract infections in children in the community: prospective online inception cohort study. Ann Fam Med. 2019; 17:14–22. PMID: 30670390.40. Burvenich R, Dillen H, Trinh NT, Freer J, Wynants L, Heytens S, De Sutter A, Verbakel JY. Antibiotic use in ambulatory care for acutely ill children in high-income countries: a systematic review and meta-analysis. Arch Dis Child. 2022; 107:1088–1094. PMID: 35948405.41. Shi HY, Zhu X, Li WL, Mak JW, Wong SH, Zhu ST, Guo SL, Chan FK, Zhang ST, Ng SC. Modulation of gut microbiota protects against viral respiratory tract infections: a systematic review of animal and clinical studies. Eur J Nutr. 2021; 60:4151–4174. PMID: 33852069.42. Lehtoranta L, Latvala S, Lehtinen MJ. Role of probiotics in stimulating the immune system in viral respiratory tract infections: a narrative review. Nutrients. 2020; 12:3163. PMID: 33081138.43. Davies T, Plummer S, Jack A, Allen M, Michael D. Lactobacillus and Bifidobacterium promote antibacterial and antiviral immune response in human macrophages. J Prob Health. 2018; 6:195.44. Webberley TS, Masetti G, Baker LM, Dally J, Hughes TR, Marchesi JR, Jack AA, Plummer SF, Ramanathan G, Facey PD, et al. The impact of Lab4 probiotic supplementation in a 90-day study in wistar rats. Front Nutr. 2021; 8:778289. PMID: 34901123.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Drug therapy for the common cold
- Erratum: A Retrospective Analysis of Use in Hospitalized Children with Upper Respiratory Tract Infection
- Vitamin D and acute lower respiratory tract infection
- Probiotics in Children: What Is the Evidence?
- The Role of Probiotics in the Prevention and Management of Allergic Diseases