Healthc Inform Res.
2024 Jan;30(1):42-48. 10.4258/hir.2024.30.1.42.
Deep Learning Model and its Application for the Diagnosis of Exudative Pharyngitis
- Affiliations
-
- 1Department of Paediatrics, National University of Singapore, Singapore
- 2Department of Cardiology, National Heart Centre, Singapore
- 3NUS High School of Math and Science, Singapore
- 4Department of Diagnostic Radiology, Singapore General Hospital, Singapore
- KMID: 2551859
- DOI: http://doi.org/10.4258/hir.2024.30.1.42
Abstract
Objectives
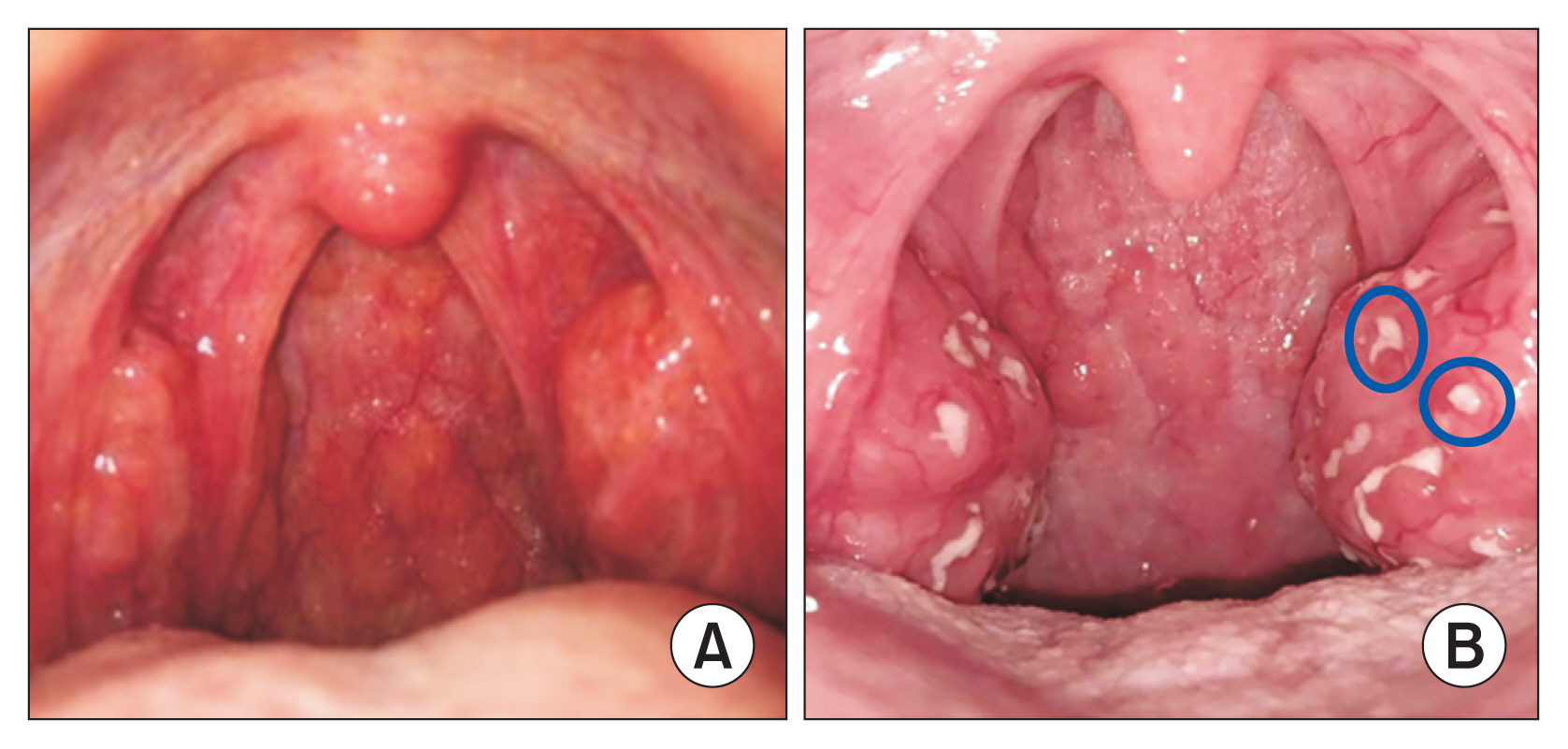
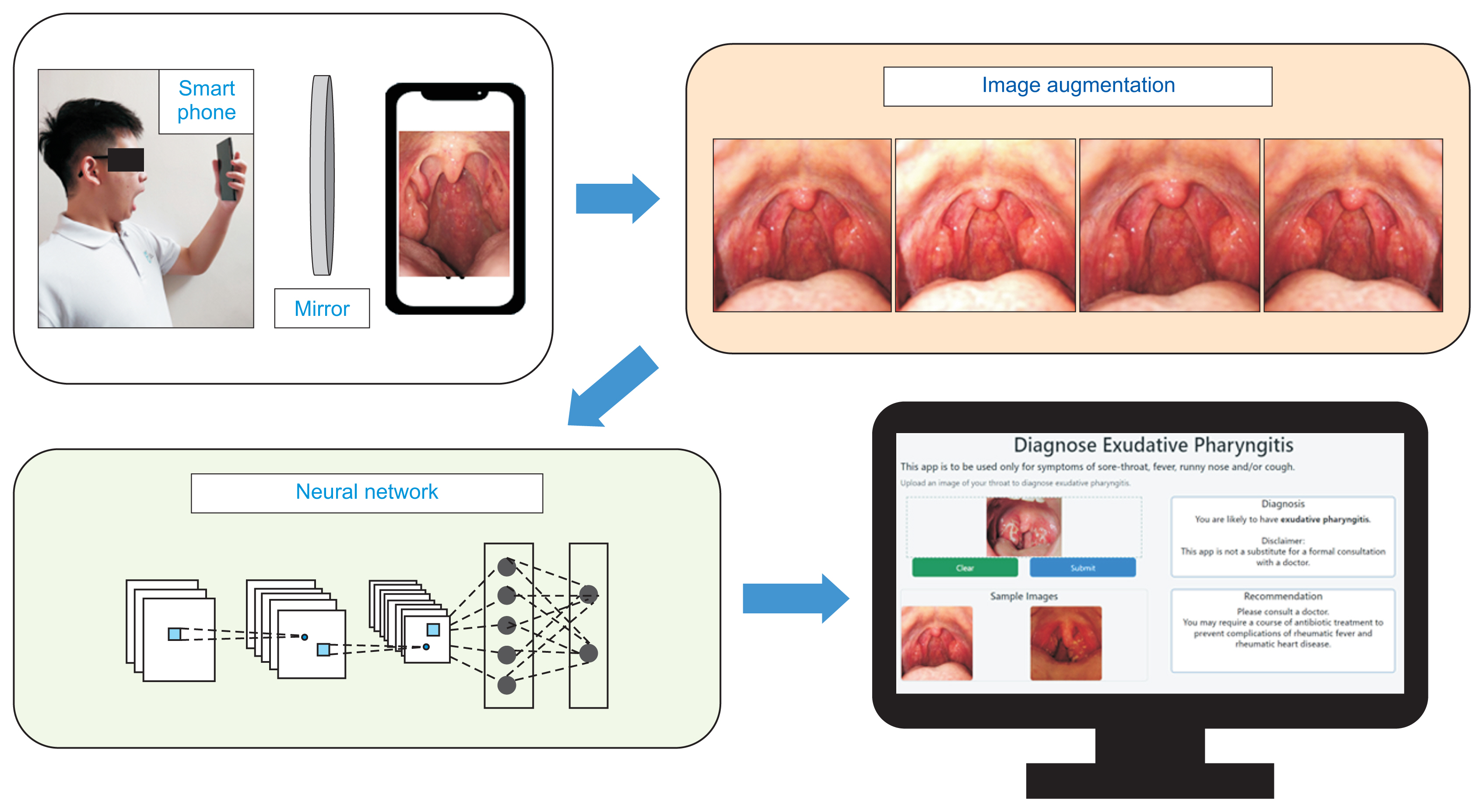
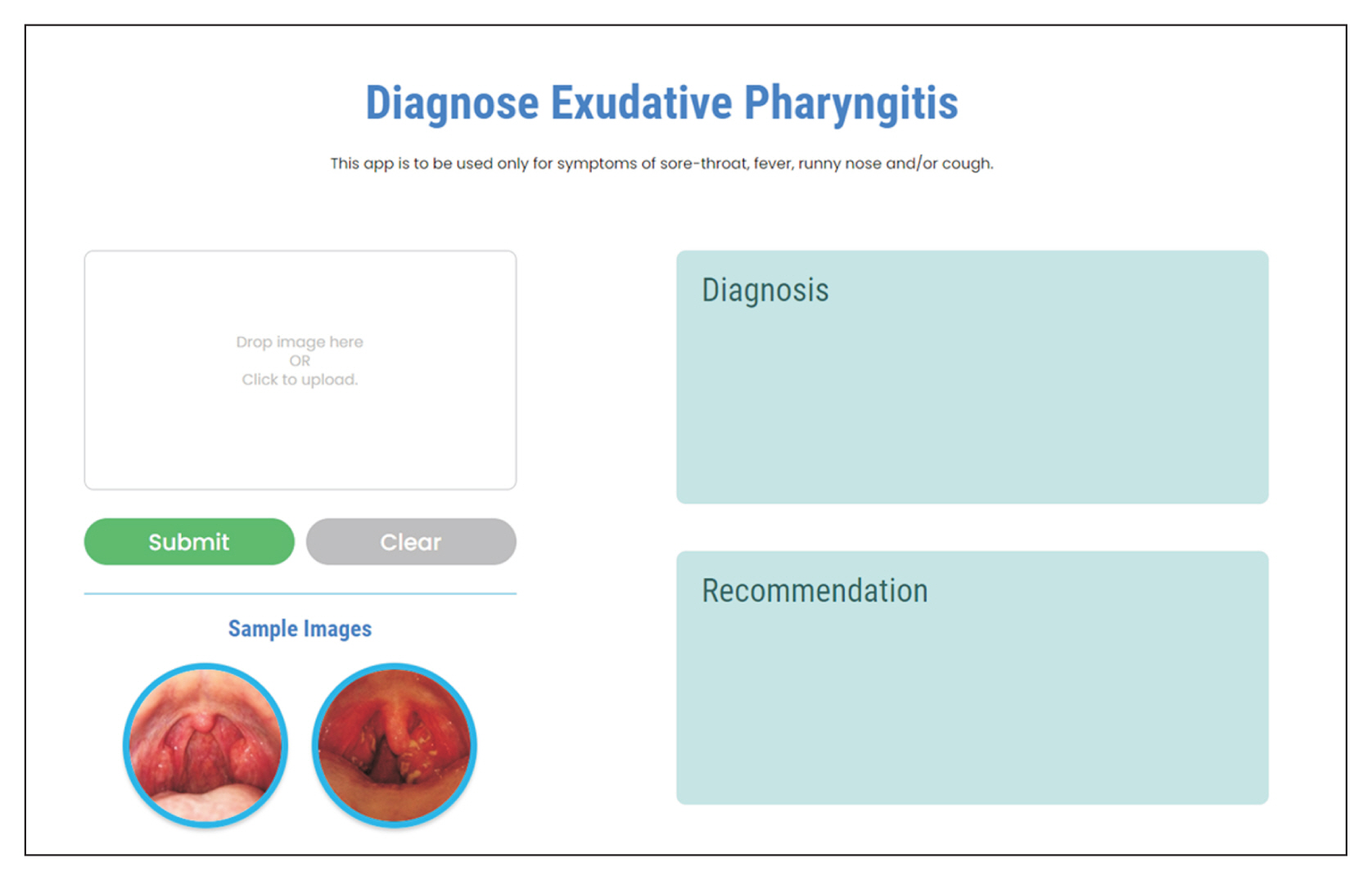
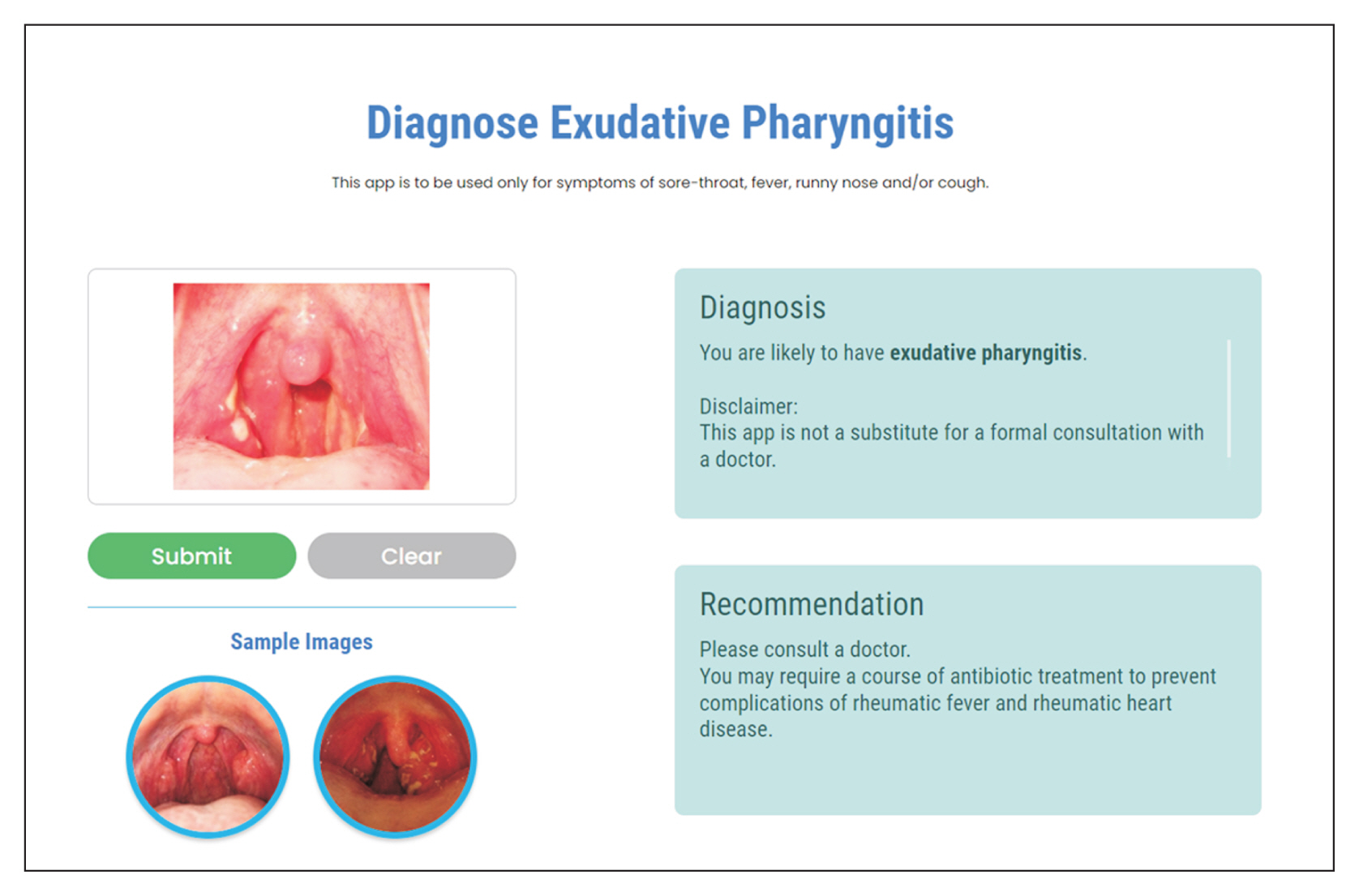
Telemedicine is firmly established in the healthcare landscape of many countries. Acute respiratory infections are the most common reason for telemedicine consultations. A throat examination is important for diagnosing bacterial pharyngitis, but this is challenging for doctors during a telemedicine consultation. A solution could be for patients to upload images of their throat to a web application. This study aimed to develop a deep learning model for the automated diagnosis of exudative pharyngitis. Thereafter, the model will be deployed online.
Methods
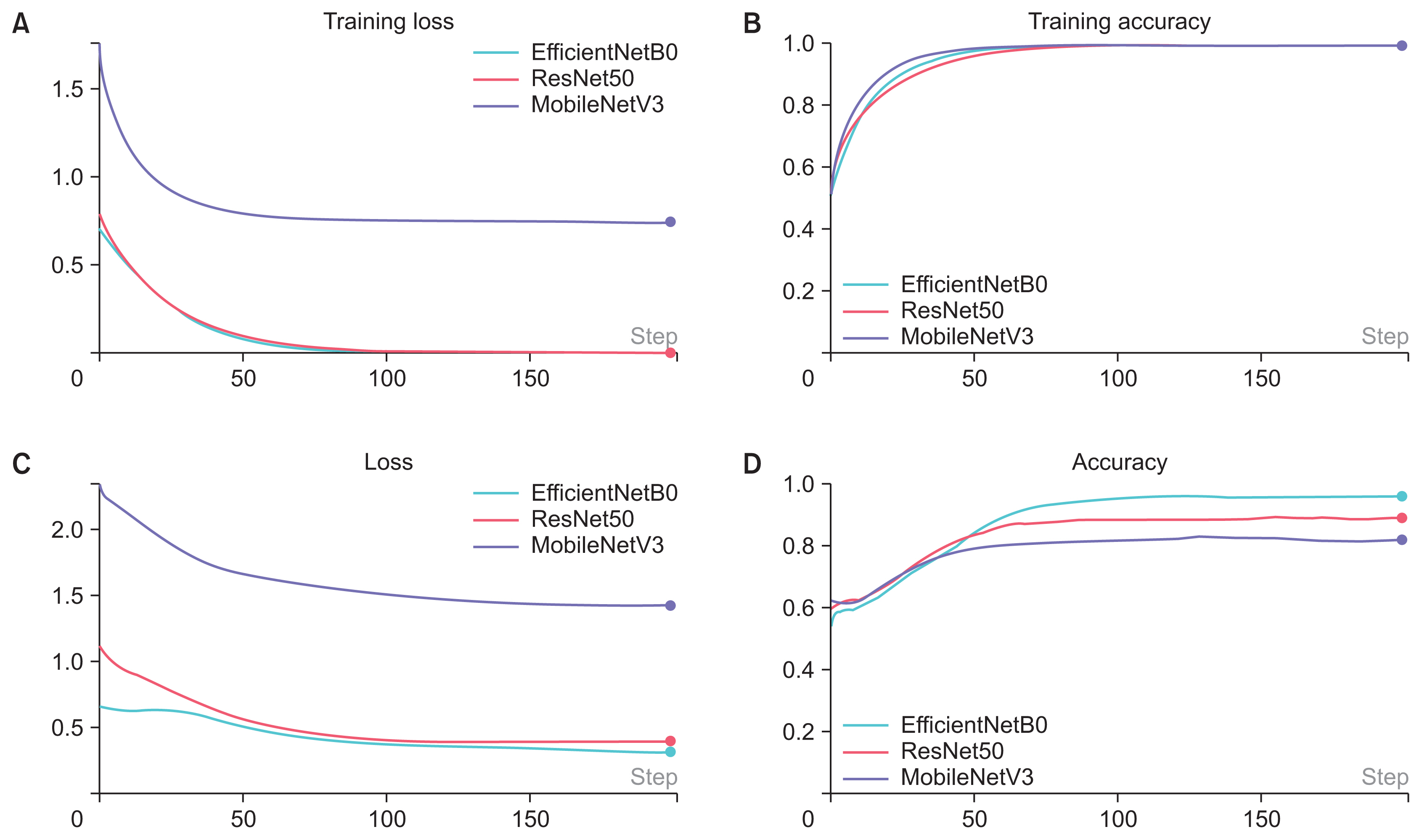
We used 343 throat images (139 with exudative pharyngitis and 204 without pharyngitis) in the study. ImageDataGenerator was used to augment the training data. The convolutional neural network models of MobileNetV3, ResNet50, and EfficientNetB0 were implemented to train the dataset, with hyperparameter tuning.
Results
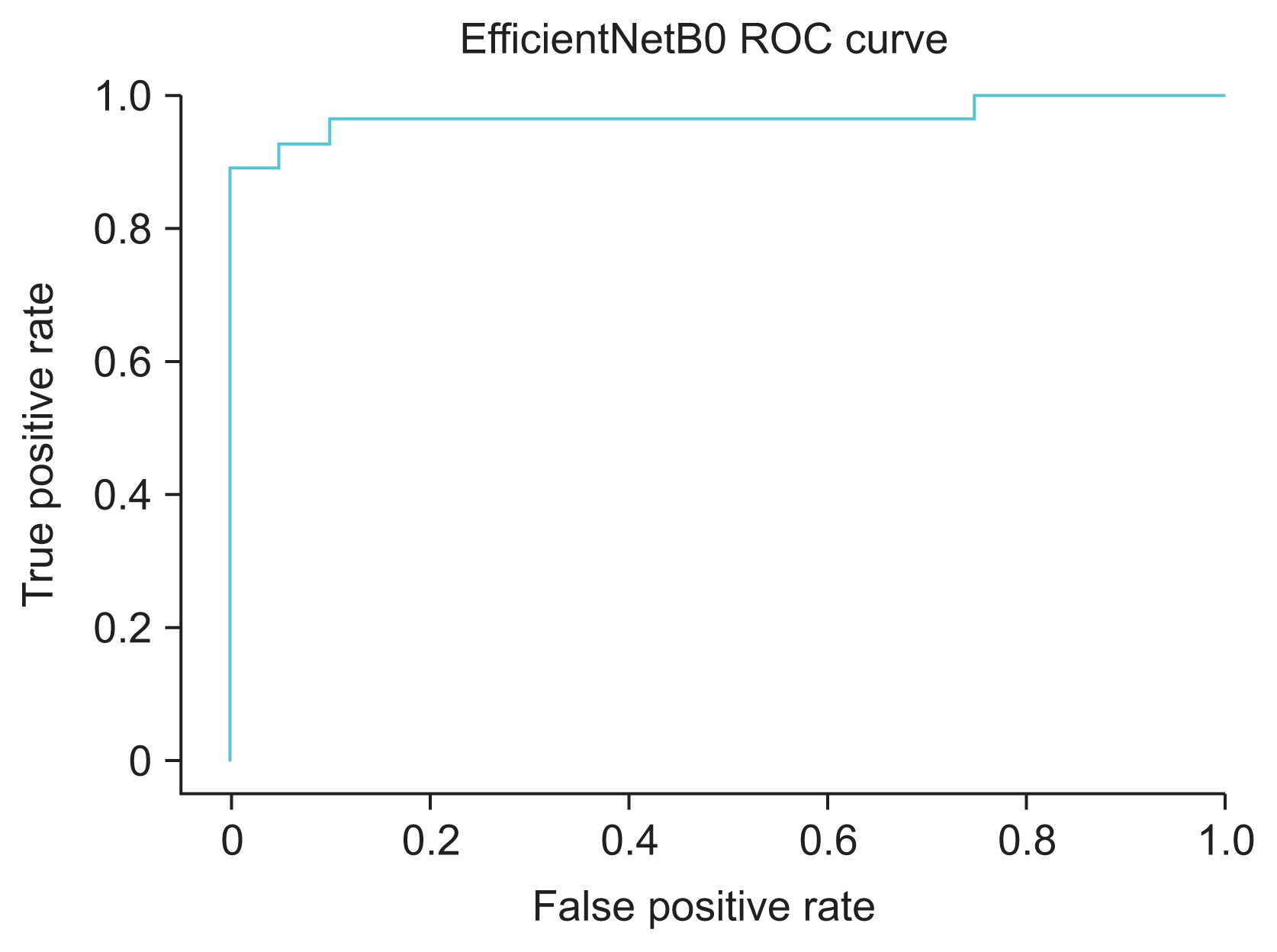
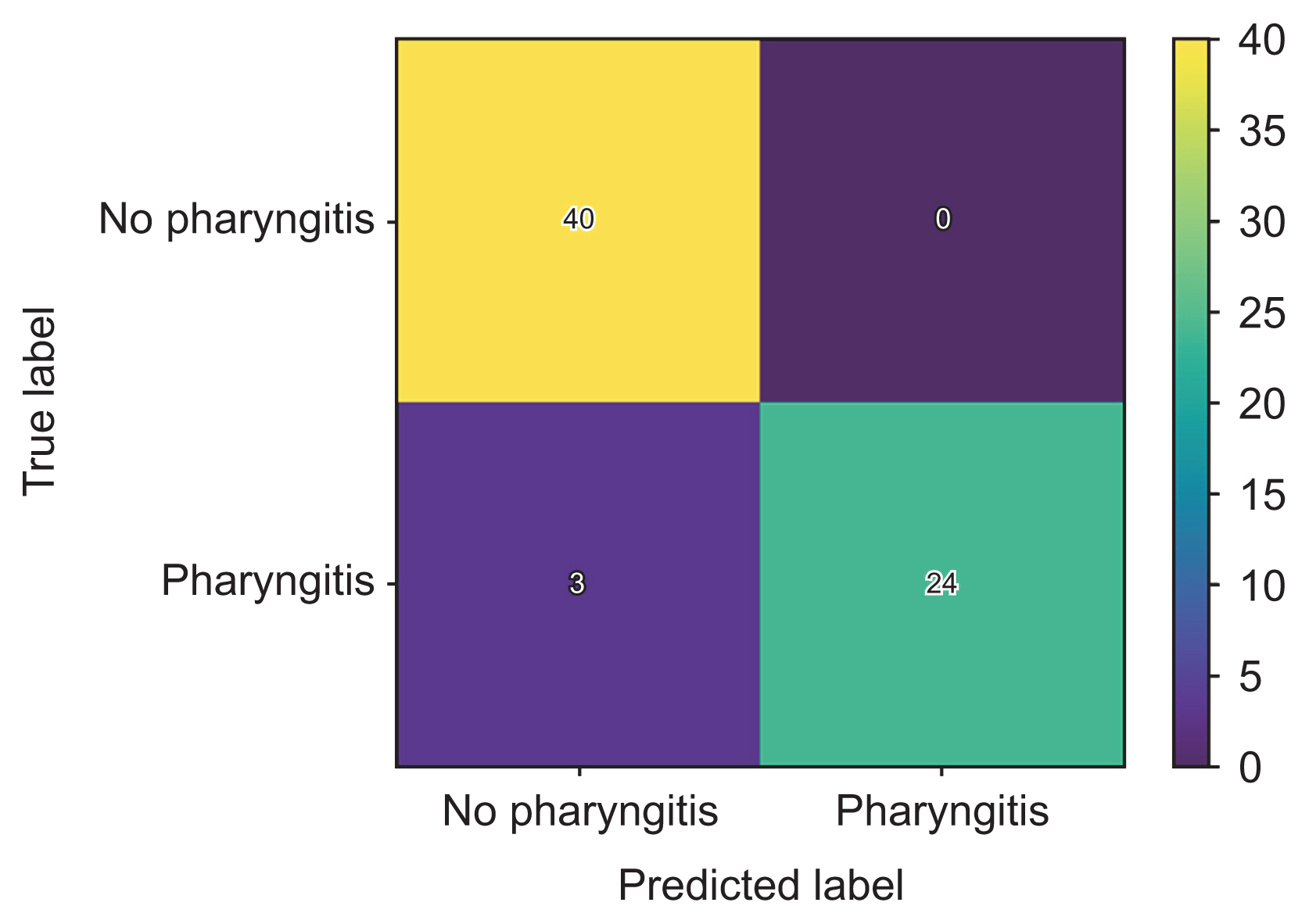
All three models were trained successfully; with successive epochs, the loss and training loss decreased, and accuracy and training accuracy increased. The EfficientNetB0 model achieved the highest accuracy (95.5%), compared to MobileNetV3 (82.1%) and ResNet50 (88.1%). The EfficientNetB0 model also achieved high precision (1.00), recall (0.89) and F1-score (0.94).
Conclusions
We trained a deep learning model based on EfficientNetB0 that can diagnose exudative pharyngitis. Our model was able to achieve the highest accuracy, at 95.5%, out of all previous studies that used machine learning for the diagnosis of exudative pharyngitis. We have deployed the model on a web application that can be used to augment the doctor’s diagnosis of exudative pharyngitis.
Figure
Reference
-
References
1. Cortez C, Mansour O, Qato DM, Stafford RS, Alexander GC. Changes in short-term, long-term, and preventive care delivery in US office-based and telemedicine visits during the COVID-19 pandemic. JAMA Health Forum. 2021; 2(7):e211529. https://doi.org/10.1001/jamahealth-forum.2021.1529.
Article2. Mandal S, Wiesenfeld BM, Mann D, Lawrence K, Chunara R, Testa P, et al. Evidence for telemedicine’s ongoing transformation of health care delivery since the onset of COVID-19: retrospective observational study. JMIR Form Res. 2022; 6(10):e38661. https://doi.org/10.2196/38661.
Article3. Saigi-Rubio F, Borges do Nascimento IJ, Robles N, Ivanovska K, Katz C, Azzopardi-Muscat N, et al. The current status of telemedicine technology use across the World Health Organization European Region: an overview of systematic reviews. J Med Internet Res. 2022; 24(10):e40877. https://doi.org/10.2196/40877.
Article4. Ministry of Health. Licensing of Telemedicine Services under the Healthcare Services Act (HCSA) [Internet]. Singapore: Ministry of Health;2023. [cited at 2024 Jan 24]. Available from: https://www.moh.gov.sg/licensing-and-regulation/telemedicine.5. Mustafa Z, Ghaffari M. Diagnostic methods, clinical guidelines, and antibiotic treatment for Group A Streptococcal Pharyngitis: a narrative review. Front Cell Infect Microbiol. 2020; 10:563627. https://doi.org/10.3389/fcimb.2020.563627.
Article6. Akhtar M, Van Heukelom PG, Ahmed A, Tranter RD, White E, Shekem N, et al. Telemedicine physical examination utilizing a consumer device demonstrates poor concordance with in-person physical examination in emergency department patients with sore throat: a prospective blinded study. Telemed J E Health. 2018; 24(10):790–6. https://doi.org/10.1089/tmj.2017.0240.
Article7. Yoo TK. Toward automated severe pharyngitis detection with smartphone camera using deep learning networks [Internet]. Amsterdam, Netherlands: Mendeley Data, Elsevier;2020. [cited at 2024 Jan 24]. Available from: https://doi.org/10.17632/8ynyhnj2kz.2.
Article8. Howard AG, Zhu M, Chen B, Kalenichenko D, Wang W, Weyand T, et al. Mobilenets: efficient convolutional neural networks for mobile vision applications [Internet]. Ithaca (NY): arXiv.org;2017. [cited at 2024 Jan 24]. Available from: https://doi.org/10.48550/arXiv.1704.04861.
Article9. Sandler M, Howard A, Zhu M, Zhmoginov A, Chen LC. MobileNetV2: inverted residuals and linear bottlenecks [Internet]. Ithaca (NY): arXiv.org;2019. [cited at 2024 Jan 24]. Available from: https://doi.org/10.48550/arXiv.1801.04381.
Article10. Howard A, Sandler M, Chen B, Wang W, Chen LC, Tan M, et al. Searching for MobileNetV3. In : Proceedings of IEEE/CVF International Conference on Computer Vision (ICCV); 2019 Oct 27–Nov 2; Seoul, South Korea. p. 1314–24. https://doi.org/10.1109/ICCV.2019.00140.
Article11. He KM, Zhang XY, Ren SQ, Sun J. Deep residual learning for image recognition. In : Proceedings of IEEE Conference on Computer Vision and Pattern Recognition (CVPR); 2016 Jun 27–30; Las Vegas, NV, USA. p. 770–8. https://doi.org/10.1109/CVPR.2016.90.
Article12. Tan M, Le QV. EfficientNet: rethinking model scaling for convolutional neural networks [Internet]. Ithaca (NY): arXiv.org;2020. [cited at 2024 Jan 24]. Available from: https://doi.org/10.48550/arXiv.1905.11946.
Article13. Yoo TK, Choi JY, Jang Y, Oh E, Ryu IH. Toward automated severe pharyngitis detection with smartphone camera using deep learning networks. Comput Biol Med. 2020; 125:103980. https://doi.org/10.1016/j.compbiomed.2020.103980.
Article14. Askarian B, Yoo SC, Chong JW. Novel image processing method for detecting strep throat (streptococcal pharyngitis) using smartphone. Sensors (Basel). 2019; 19(15):3307. https://doi.org/10.3390/s19153307.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Development of an Optimized Deep Learning Model for Medical Imaging
- Deep Learning in Nuclear Medicine and Molecular Imaging: Current Perspectives and Future Directions
- Deep Learning in Dental Radiographic Imaging
- Deep Learning in MR Motion Correction:a Brief Review and a New Motion Simulation Tool (view2Dmotion)
- Developing and Evaluating Deep Learning Algorithms for Object Detection: Key Points for Achieving Superior Model Performance