Korean J Orthod.
2024 Jan;54(1):26-47. 10.4041/kjod23.064.
Role of vitamin D for orthodontic tooth movement, external apical root resorption, and bone biomarker expression and remodeling: A systematic review
- Affiliations
-
- 1Dentistry Unit, Department of Health Sciences, Magna Graecia University of Catanzaro, Catanzaro, Italy
- 2Physical Medicine and Rehabilitation Unit, Department of Neurosciences, ASST Carlo Poma, Mantova, Italy
- 3Physical and Rehabilitative Medicine, Department of Health Sciences, University of Eastern Piedmont “A. Avogadro”, Novara, Italy
- 4Translational Medicine, Dipartimento Attività Integrate Ricerca e Innovazione (DAIRI), Azienda Ospedaliera SS. Antonio e Biagio e Cesare Arrigo, Alessandria, Italy
- 5Department of Anatomy, Histology, Forensic Medicine and Orthopedics, Sapienza University, Rome, Italy
- 6Department of Neurological and Rehabilitation Science, IRCCS San Raffaele, Rome, Italy
- 7Dentistry Unit, Department of Translational Medicine, University of Eastern Piedmont “A. Avogadro”, Novara, Italy
- 8Physical Medicine and Rehabilitation Unit, Department of Medical and Surgical Sciences, Magna Graecia University of Catanzaro, Catanzaro, Italy
- KMID: 2551473
- DOI: http://doi.org/10.4041/kjod23.064
Abstract
Objective
This systematic review aimed to evaluate the correlation between vitamin D levels and the rate of tooth movement, external apical root resorption, bone biomarker expression, and bone remodeling.
Methods
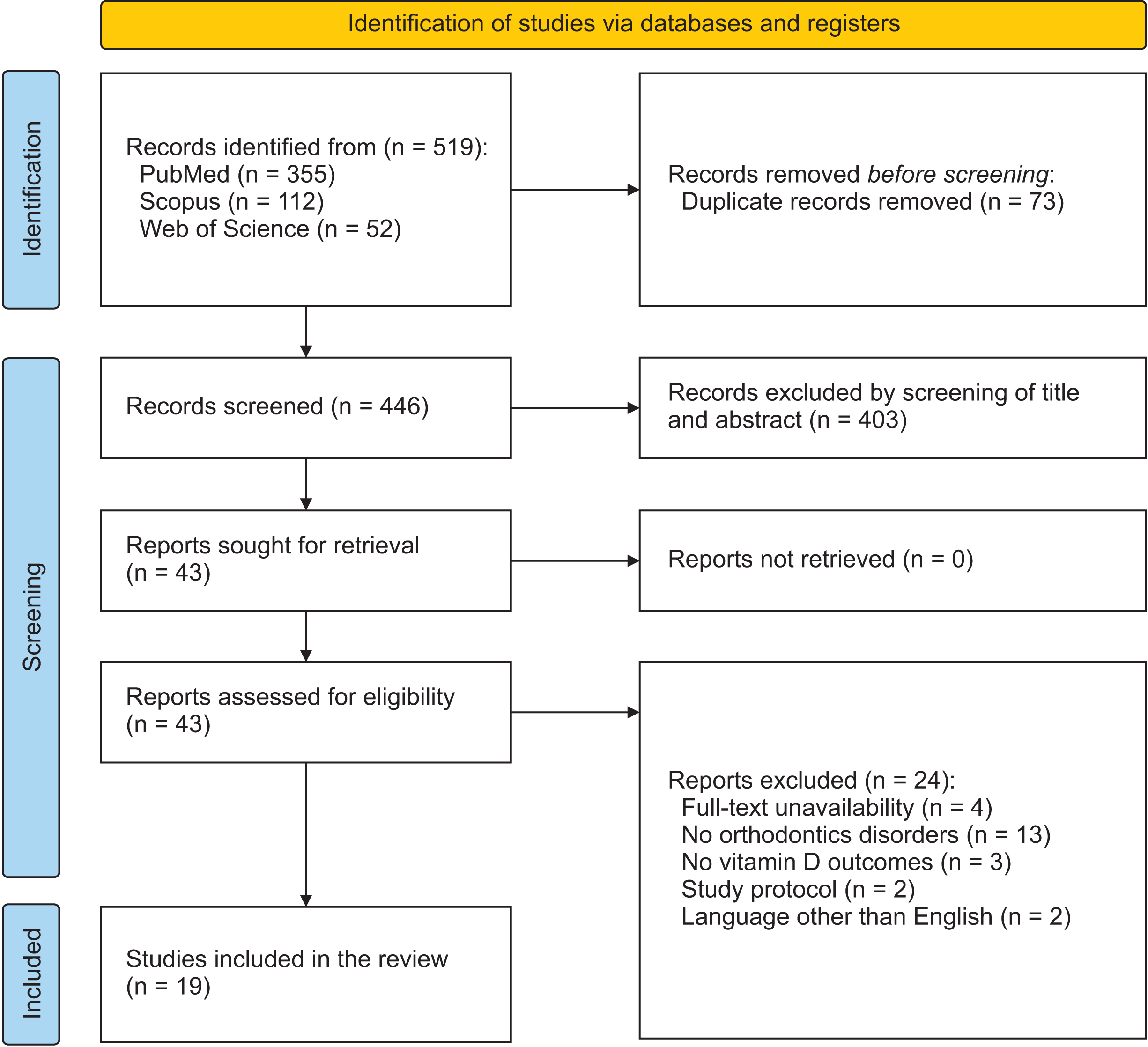
Three databases (PubMed, Scopus, and Web of Science) were systematically searched from inception until 14th March 2023 to identify studies investigating the correlation between orthodontic tooth movement and vitamin D in animals and humans. The quality assessment was made in accordance with the Joanna Briggs Institute Critical Appraisal Checklist.
Results
Overall, 519 records were identified, and 19 were selected for the qualitative synthesis. Eleven studies investigated the effect of local administration (injections in the periodontal ligament, to the gingiva distal to the teeth, or submucosae palatal area) and systemic administration (oral supplementation) of vitamin D on tooth movement, external apical root movement, pro-inflammatory cytokines, and bone remodeling factors. The remaining eight studies investigated the correlation between serum vitamin D levels and salivary vitamin D levels on bone turnover markers and tooth movement. Conclusions: The findings of this systematic review support that vitamin D3 local injections might increase the rate of tooth movement via the receptor activator of the nuclear factor-kB/osteoprotegerin axis. However, the non-uniform study designs and the different protocols and outcome methods make it challenging to draw reliable conclusions.
Figure
Reference
-
1. Kapoor P, Kharbanda OP, Monga N, Miglani R, Kapila S. 2014; Effect of orthodontic forces on cytokine and receptor levels in gingival crevicular fluid: a systematic review. Prog Orthod. 15:65. https://doi.org/10.1186/s40510-014-0065-6. DOI: 10.1186/s40510-014-0065-6. PMID: 25487828. PMCID: PMC4259981.2. Meikle MC. 2006; The tissue, cellular, and molecular regulation of orthodontic tooth movement: 100 years after Carl Sandstedt. Eur J Orthod. 28:221–40. https://doi.org/10.1093/ejo/cjl001. DOI: 10.1093/ejo/cjl001. PMID: 16687469.3. Masella RS, Meister M. 2006; Current concepts in the biology of orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 129:458–68. https://doi.org/10.1016/j.ajodo.2005.12.013. DOI: 10.1016/j.ajodo.2005.12.013. PMID: 16627170.4. Yamaguchi M. 2009; RANK/RANKL/OPG during orthodontic tooth movement. Orthod Craniofac Res. 12:113–9. https://doi.org/10.1111/j.1601-6343.2009.01444.x. DOI: 10.1111/j.1601-6343.2009.01444.x. PMID: 19419454.5. Kobayashi Y, Hashimoto F, Miyamoto H, Kanaoka K, Miyazaki-Kawashita Y, Nakashima T, et al. 2000; Force-induced osteoclast apoptosis in vivo is accompanied by elevation in transforming growth factor beta and osteoprotegerin expression. J Bone Miner Res. 15:1924–34. https://doi.org/10.1359/jbmr.2000.15.10.1924. DOI: 10.1359/jbmr.2000.15.10.1924. PMID: 11028444.6. Epsley S, Tadros S, Farid A, Kargilis D, Mehta S, Rajapakse CS. 2021; The effect of inflammation on bone. Front Physiol. 11:511799. https://doi.org/10.3389/fphys.2020.511799. DOI: 10.3389/fphys.2020.511799. PMID: 33584321. PMCID: PMC7874051. PMID: cbd5650c277845409a2d127c1a615cfa.7. Uematsu S, Mogi M, Deguchi T. 1996; Interleukin (IL)-1 beta, IL-6, tumor necrosis factor-alpha, epidermal growth factor, and beta 2-microglobulin levels are elevated in gingival crevicular fluid during human orthodontic tooth movement. J Dent Res. 75:562–7. https://doi.org/10.1177/00220345960750010801. DOI: 10.1177/00220345960750010801. PMID: 8655760.8. Yamaguchi M, Aihara N, Kojima T, Kasai K. 2006; RANKL increase in compressed periodontal ligament cells from root resorption. J Dent Res. 85:751–6. https://doi.org/10.1177/154405910608500812. DOI: 10.1177/154405910608500812. PMID: 16861294.9. Xiong J, Piemontese M, Onal M, Campbell J, Goellner JJ, Dusevich V, et al. 2015; Osteocytes, not osteoblasts or lining cells, are the main source of the RANKL required for osteoclast formation in remodeling bone. PLoS One. 10:e0138189. https://doi.org/10.1371/journal.pone.0138189. DOI: 10.1371/journal.pone.0138189. PMID: 26393791. PMCID: PMC4578942. PMID: 35f70f5672144557a69c5e41b87ba366.10. Küchler EC, Schröder A, Teodoro VB, Nazet U, Scariot R, Spanier G, et al. 2021; The role of 25-hydroxyvitamin-D3 and vitamin D receptor gene in human periodontal ligament fibroblasts as response to orthodontic compressive strain: an in vitro study. BMC Oral Health. 21:386. https://doi.org/10.1186/s12903-021-01740-8. DOI: 10.1186/s12903-021-01740-8. PMID: 34362362. PMCID: PMC8344219. PMID: 8ff58cff7ff94713a46335784767b956.11. Bischoff-Ferrari HA, Borchers M, Gudat F, Dürmüller U, Stähelin HB, Dick W. 2004; Vitamin D receptor expression in human muscle tissue decreases with age. J Bone Miner Res. 19:265–9. https://doi.org/10.1359/jbmr.2004.19.2.265. DOI: 10.1359/jbmr.2004.19.2.265. PMID: 14969396.12. Iolascon G, Moretti A, de Sire A, Calafiore D, Gimigliano F. 2017; Effectiveness of calcifediol in improving muscle function in post-menopausal women: a prospective cohort study. Adv Ther. 34:744–52. https://doi.org/10.1007/s12325-017-0492-0. DOI: 10.1007/s12325-017-0492-0. PMID: 28205055.13. Li B, Zhang YH, Wang LX, Li X, Zhang XD. 2015; Expression of OPG, RANKL, and RUNX2 in rabbit periodontium under orthodontic force. Genet Mol Res. 14:19382–8. https://doi.org/10.4238/2015.December.29.48. DOI: 10.4238/2015.December.29.48. PMID: 26782591.14. Yu X, Zong X, Pan Y. 2019; Associations between vitamin D receptor genetic variants and periodontitis: a meta-analysis. Acta Odontol Scand. 77:484–94. https://doi.org/10.1080/00016357.2019.1597160. DOI: 10.1080/00016357.2019.1597160. PMID: 30957605.15. Ferrillo M, Lippi L, Giudice A, Calafiore D, Paolucci T, Renò F, et al. 2022; Temporomandibular disorders and vitamin D deficiency: what is the linkage between these conditions? A systematic review. J Clin Med. 11:6231. https://doi.org/10.3390/jcm11216231. DOI: 10.3390/jcm11216231. PMID: 36362456. PMCID: PMC9655046. PMID: 8ac1697e351f4ab98531d0410fa4ffcd.16. Ferrillo M, Migliario M, Roccuzzo A, Molinero-Mourelle P, Falcicchio G, Umano GR, et al. 2021; Periodontal disease and vitamin D deficiency in pregnant women: which correlation with preterm and low-weight birth? J Clin Med. 10:4578. https://doi.org/10.3390/jcm10194578. DOI: 10.3390/jcm10194578. PMID: 34640596. PMCID: PMC8509337. PMID: 068c189b189f4ec9b9f1ec0047e9c116.17. Ferrillo M, Migliario M, Marotta N, Lippi L, Antonelli A, Calafiore D, et al. 2022; Oral health in breast cancer women with vitamin D deficiency: a machine learning study. J Clin Med. 11:4662. https://doi.org/10.3390/jcm11164662. DOI: 10.3390/jcm11164662. PMID: 36012901. PMCID: PMC9410090. PMID: 17a91984e29c4055bf6c07ab764157b5.18. Arqub SA, Gandhi V, Iverson MG, Ahmed M, Kuo CL, Mu J, et al. 2021; The effect of the local administration of biological substances on the rate of orthodontic tooth movement: a systematic review of human studies. Prog Orthod. 22:5. https://doi.org/10.1186/s40510-021-00349-5. DOI: 10.1186/s40510-021-00349-5. PMID: 33523325. PMCID: PMC7851211. PMID: 743414f993c849b5a3cb520db89d1f93.19. Al-Attar A, Abid M, Dziedzic A, Al-Khatieeb MM, Seppala M, Cobourne MT, et al. 2021; The impact of calcitriol on orthodontic tooth movement: a cumulative systematic review and meta-analysis. Appl Sci. 11:8882. https://doi.org/10.3390/app11198882. DOI: 10.3390/app11198882. PMID: 131f57e1fedd4db79bdef1a69806d710.20. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. 2021; The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 372:n71. https://doi.org/10.1136/bmj.n71. DOI: 10.1136/bmj.n71. PMID: 33782057. PMCID: PMC8005924.21. Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. 2015; Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc. 13:147–53. https://doi.org/10.1097/XEB.0000000000000054. DOI: 10.1097/XEB.0000000000000054. PMID: 26317388.22. Al-hasani NR, Al-bustani AI, Ghareeb MM, Hussain SA. 2011; Clinical efficacy of locally injected calcitriol in orthodontic tooth movement. Int J Pharm Pharm Sci. 5:139–43. https://d1wqtxts1xzle7.cloudfront.net/66870183/CLINICAL_EFFICACY_OF_LOCALLY_INJECTED_CA20210504-24281-ddxdes.pdf?1620114250=&response-content-disposition=inline%3B+filename%3DClinical_Efficacy_of_Locally_Injected_Ca.pdf&Expires=1701758593&Signature=dZJgk~ThTLt7nJY7CFIoSpXtJkBtc1S-3ozaAspvEJxRiQXcLNp5oYQ6~NSp-qg8cwWY1co6uWFAi1U7NI-dBg1oiv-CDsi9RxNwGi6w4zw~VQJZyD-Fv-h8z9B3JmxDGbS2FSjetrym~B5J9JxNGQWfcMvSEIdVNEKjUuTmH7FxA2gCl-7VQ2D8b7my61rp8YNfSFCF~X4Q-ypmuDpRFOhg40WHHNy-lFJSiWticvx5JKBZwAYKaot7j3EH3B9lAc~FO9-rOntGwWRTGwXJr54CZDnacoBcOrFMz7VStRUW3wOD-8rEX-dJJjo49TT1NRPJhfIvl2BRLuGJ2bvdPw__&Key-Pair-Id=APKAJLOHF5GGSLRBV4ZA">https://d1wqtxts1xzle7.cloudfront.net/66870183/CLINICAL_EFFICACY_OF_LOCALLY_INJECTED_CA20210504-24281-ddxdes.pdf?1620114250=&response-content-disposition=inline%3B+filename%3DClinical_Efficacy_of_Locally_Injected_Ca.pdf&Expires=1701758593&Signature=dZJgk~ThTLt7nJY7CFIoSpXtJkBtc1S-3ozaAspvEJxRiQXcLNp5oYQ6~NSp-qg8cwWY1co6uWFAi1U7NI-dBg1oiv-CDsi9RxNwGi6w4zw~VQJZyD-Fv-h8z9B3JmxDGbS2FSjetrym~B5J9JxNGQWfcMvSEIdVNEKjUuTmH7FxA2gCl-7VQ2D8b7my61rp8YNfSFCF~X4Q-ypmuDpRFOhg40WHHNy-lFJSiWticvx5JKBZwAYKaot7j3EH3B9lAc~FO9-rOntGwWRTGwXJr54CZDnacoBcOrFMz7VStRUW3wOD-8rEX-dJJjo49TT1NRPJhfIvl2BRLuGJ2bvdPw__&Key-Pair-Id=APKAJLOHF5GGSLRBV4ZA.23. Iosub Ciur MD, Zetu IN, Haba D, Viennot S, Bourgeois D, Andrian S. 2016; Evaluation of the influence of local administration of vitamin D on the rate of orthodontic tooth movement. Rev Med Chir Soc Med Nat Iasi. 120:694–99. https://pubmed.ncbi.nlm.nih.gov/30148332/.24. Collins MK, Sinclair PM. 1988; The local use of vitamin D to increase the rate of orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 94:278–84. https://doi.org/10.1016/0889-5406(88)90052-2. DOI: 10.1016/0889-5406(88)90052-2. PMID: 3177281.25. Cui J, Li J, Wang W, Han X, Du J, Sun J, et al. 2016; The effect of calcitriol on high mobility group box 1 expression in periodontal ligament cells during orthodontic tooth movement in rats. J Mol Histol. 47:221–8. https://doi.org/10.1007/s10735-016-9669-0. DOI: 10.1007/s10735-016-9669-0. PMID: 26956363.26. Fontana ML, de Souza CM, Bernardino JF, Hoette F, Hoette ML, Thum L, et al. 2012; Association analysis of clinical aspects and vitamin D receptor gene polymorphism with external apical root resorption in orthodontic patients. Am J Orthod Dentofacial Orthop. 142:339–47. https://doi.org/10.1016/j.ajodo.2012.04.013. DOI: 10.1016/j.ajodo.2012.04.013. PMID: 22920700.27. Kale S, Kocadereli I, Atilla P, Aşan E. 2004; Comparison of the effects of 1,25 dihydroxycholecalciferol and prostaglandin E2 on orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 125:607–14. https://doi.org/10.1016/j.ajodo.2003.06.002. DOI: 10.1016/j.ajodo.2003.06.002. PMID: 15127030.28. Kawakami M, Takano-Yamamoto T. 2004; Local injection of 1,25-dihydroxyvitamin D3 enhanced bone formation for tooth stabilization after experimental tooth movement in rats. J Bone Miner Metab. 22:541–6. https://doi.org/10.1007/s00774-004-0521-3. DOI: 10.1007/s00774-004-0521-3. PMID: 15490263.29. Khalaf RM, Almudhi AA. 2022; Effects of vitamin D deficiency on the rate of orthodontic tooth movement: an animal study. Saudi Dent J. 34:129–35. https://doi.org/10.1016/j.sdentj.2021.12.008. DOI: 10.1016/j.sdentj.2021.12.008. PMID: 35241902. PMCID: PMC8864377.30. Khalaf RM, Almudhi AA. 2022; The effect of vitamin D deficiency on the RANKL/OPG ratio in rats. J Oral Biol Craniofac Res. 12:228–32. https://doi.org/10.1016/j.jobcr.2022.02.004. DOI: 10.1016/j.jobcr.2022.02.004. PMID: 35242513. PMCID: PMC8886034.31. Leszczyszyn A, Hnitecka S, Dominiak M. 2021; Could vitamin D3 deficiency influence malocclusion development? Nutrients. 13:2122. https://doi.org/10.3390/nu13062122. DOI: 10.3390/nu13062122. PMID: 34205632. PMCID: PMC8234332. PMID: 442bd1fa749546d38b8089f8a24703a4.32. Takano-Yamamoto T, Kawakami M, Kobayashi Y, Yamashiro T, Sakuda M. 1992; The effect of local application of 1,25-dihydroxycholecalciferol on osteoclast numbers in orthodontically treated rats. J Dent Res. 71:53–9. https://doi.org/10.1177/00220345920710010901. DOI: 10.1177/00220345920710010901. PMID: 1311005.33. Tashkandi N, Zhao Y, Mitchell-Lee G, Stephens D, Patel M, Motro M, et al. 2021; Longitudinal assessment of salivary vitamin D binding protein during orthodontic tooth movement. BMC Oral Health. 21:332. https://doi.org/10.1186/s12903-021-01689-8. DOI: 10.1186/s12903-021-01689-8. PMID: 34225707. PMCID: PMC8256539. PMID: 4671c610c8ce48a3ae336aaf95329950.34. Tehranchi A, Sadighnia A, Younessian F, Abdi AH, Shirvani A. 2017; Correlation of vitamin D status and orthodontic-induced external apical root resorption. Dent Res J (Isfahan). 14:403–11. https://doi.org/10.4103/1735-3327.218565. DOI: 10.4103/1735-3327.218565. PMID: 29238379. PMCID: PMC5713064. PMID: b391c9b403d54185a6e3e92ba3300893.35. Varughese ST, Shamanna PU, Goyal N, Thomas BS, Lakshmanan L, Pulikkottil VJ, et al. 2019; Effect of vitamin D on canine distalization and alveolar bone density using multi-slice spiral CT: a randomized controlled trial. J Contemp Dent Pract. 20:1430–5. https://doi.org/10.5005/jp-journals-10024-2698. DOI: 10.5005/jp-journals-10024-2698. PMID: 32381845.36. Al-Attar A, Abid M. 2022; The effect of vitamin D3 on the alignment of mandibular anterior teeth: a randomized controlled clinical trial. Int J Dent. 2022:6555883. https://doi.org/10.1155/2022/6555883. DOI: 10.1155/2022/6555883. PMID: 35198025. PMCID: PMC8860536. PMID: 54d5b01becd8497fa7affe63322e7582.37. Azizi F, Karami N, Golshah A, Imani MM, Safari-Faramani R. 2022; Effect of serum level of vitamin D on external apical root resorption in maxillary anterior teeth in patients under fixed orthodontic treatment. Int J Dent. 2022:7942998. https://doi.org/10.1155/2022/7942998. DOI: 10.1155/2022/7942998. PMID: 36203821. PMCID: PMC9532138. PMID: 40c05fccffa645e8a32856f266f329ff.38. Gratton MP, Londono I, Rompré P, Villemure I, Moldovan F, Nishio C. 2022; Effect of vitamin D on bone morphometry and stability of orthodontic tooth movement in rats. Am J Orthod Dentofacial Orthop. 162:e319–27. https://doi.org/10.1016/j.ajodo.2022.08.019. DOI: 10.1016/j.ajodo.2022.08.019. PMID: 36216621.39. Marañón-Vásquez G, Küchler EC, Hermann S, Paddenberg E, Schröder A, Baratto-Filho F, et al. 2023; Association between genetic variants in key vitamin-D-pathway genes and external apical root resorption linked to orthodontic treatment. Eur J Oral Sci. 131:e12916. https://doi.org/10.1111/eos.12916. DOI: 10.1111/eos.12916. PMID: 36683003.40. Moradinejad M, Yazdi M, Mard SA, Razavi SM, Shamohammadi M, Shahsanaei F, et al. 2022; Efficacy of the systemic co-administration of vitamin D3 in reversing the inhibitory effects of sodium alendronate on orthodontic tooth movement: a preliminary experimental animal study. Am J Orthod Dentofacial Orthop. 162:e17–27. https://doi.org/10.1016/j.ajodo.2021.11.014. DOI: 10.1016/j.ajodo.2021.11.014. PMID: 35501223.41. Institute TJB. 2017. JBI critical appraisal tools [Internet]. Institute TJB;Adelaide: Available from: https://jbi.global/critical-appraisal-tools. cited 2023 Sep 21.42. Küchler EC, Schröder A, Corso P, Scariot R, Spanier G, Proff P, et al. 2020; Genetic polymorphisms influence gene expression of human periodontal ligament fibroblasts in the early phases of orthodontic tooth movement. Odontology. 108:493–502. https://doi.org/10.1007/s10266-019-00475-x. DOI: 10.1007/s10266-019-00475-x. PMID: 31741103.43. Mitsea A, Palikaraki G, Karamesinis K, Vastardis H, Gizani S, Sifakakis I. 2022; Evaluation of lateral incisor resorption caused by impacted maxillary canines based on CBCT: a systematic review and meta-analysis. Children (Basel). 9:1006. https://doi.org/10.3390/children9071006. DOI: 10.3390/children9071006. PMID: 35883990. PMCID: PMC9323464. PMID: fb45d8fff8e64eac9e9c14a695604a47.44. Nieto-Nieto N, Solano JE, Yañez-Vico R. 2017; External apical root resorption concurrent with orthodontic forces: the genetic influence. Acta Odontol Scand. 75:280–7. https://doi.org/10.1080/00016357.2017.1294260. DOI: 10.1080/00016357.2017.1294260. PMID: 28358285.45. Bizzarro M, Generali C, Maietta S, Martorelli M, Ferrillo M, Flores-Mir C, et al. 2018; Association between 3D palatal morphology and upper arch dimensions in buccally displaced maxillary canines early in mixed dentition. Eur J Orthod. 40:592–6. https://doi.org/10.1093/ejo/cjy023. DOI: 10.1093/ejo/cjy023. PMID: 29726936.46. Hasan HS, Elkolaly MA, Elmoazen R, Kolemen A, Al Azzawi AM. 2022; Factors that guide the diagnosis and treatment planning for impacted canines using three-dimensional cone-beam computed tomography: a cross-sectional study. Int J Dent. 2022:7582449. https://doi.org/10.1155/2022/7582449. DOI: 10.1155/2022/7582449. PMID: 36225991. PMCID: PMC9550469. PMID: d232ac15f7f94d0ea02428fac57b180b.47. Ferrillo M, Migliario M, Curci C, Roccuzzo A, Invernizzi M, de Sire A. 2021; Reliability of dental calcification compared to hand-wrist X-ray to evaluate skeletal maturation in growing subjects: a systematic review. J Biol Regul Homeost Agents. 35:717–23. https://doi.org/10.23812/21-106-L. DOI: 10.23812/21-106-L. PMID: 33913306.48. Gonzales C, Hotokezaka H, Yoshimatsu M, Yozgatian JH, Darendeliler MA, Yoshida N. 2008; Force magnitude and duration effects on amount of tooth movement and root resorption in the rat molar. Angle Orthod. 78:502–9. https://doi.org/10.2319/052007-240.1. DOI: 10.2319/052007-240.1. PMID: 18416627.49. Küchler EC, Schröder A, Spanier G, Thedei G Jr, Carvalho Ribeiro de Oliveira MB, de Menezes-Oliveira MAH, et al. 2022; Influence of single-nucleotide polymorphisms on vitamin D receptor expression in periodontal ligament fibroblasts as a response to orthodontic compression. Int J Mol Sci. 23:15948. https://doi.org/10.3390/ijms232415948. DOI: 10.3390/ijms232415948. PMID: 36555589. PMCID: PMC9787981. PMID: 88382f37908344fdbae7cb94906e44ab.50. Booij-Vrieling HE, Ferbus D, Tryfonidou MA, Riemers FM, Penning LC, Berdal A, et al. 2010; Increased vitamin D-driven signalling and expression of the vitamin D receptor, MSX2, and RANKL in tooth resorption in cats. Eur J Oral Sci. 118:39–46. https://doi.org/10.1111/j.1600-0722.2009.00707.x. DOI: 10.1111/j.1600-0722.2009.00707.x. PMID: 20156263.51. Yang CY, Jeon HH, Alshabab A, Lee YJ, Chung CH, Graves DT. 2018; RANKL deletion in periodontal ligament and bone lining cells blocks orthodontic tooth movement. Int J Oral Sci. 10:3. https://doi.org/10.1038/s41368-017-0004-8. DOI: 10.1038/s41368-017-0004-8. PMID: 29483595. PMCID: PMC5944595.52. Nebel D, Svensson D, Arosenius K, Larsson E, Jönsson D, Nilsson BO. 2015; 1α,25-dihydroxyvitamin D3 promotes osteogenic activity and downregulates proinflammatory cytokine expression in human periodontal ligament cells. J Periodontal Res. 50:666–73. https://doi.org/10.1111/jre.12249. DOI: 10.1111/jre.12249. PMID: 25495336.53. Andersson U, Wang H, Palmblad K, Aveberger AC, Bloom O, Erlandsson-Harris H, et al. 2000; High mobility group 1 protein (HMG-1) stimulates proinflammatory cytokine synthesis in human monocytes. J Exp Med. 192:565–70. https://doi.org/10.1084/jem.192.4.565. DOI: 10.1084/jem.192.4.565. PMID: 10952726. PMCID: PMC2193240.54. Kirschneck C, Proff P, Maurer M, Reicheneder C, Römer P. 2015; Orthodontic forces add to nicotine-induced loss of periodontal bone: an in vivo and in vitro study. J Orofac Orthop. 76:195–212. https://doi.org/10.1007/s00056-015-0283-7. DOI: 10.1007/s00056-015-0283-7. PMID: 25929709.55. Madureira DF, Taddei Sde A, Abreu MH, Pretti H, Lages EM, da Silva TA. 2012; Kinetics of interleukin-6 and chemokine ligands 2 and 3 expression of periodontal tissues during orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 142:494–500. https://doi.org/10.1016/j.ajodo.2012.05.012. DOI: 10.1016/j.ajodo.2012.05.012. PMID: 22999673.56. Fonseca JE, Santos MJ, Canhão H, Choy E. 2009; Interleukin-6 as a key player in systemic inflammation and joint destruction. Autoimmun Rev. 8:538–42. https://doi.org/10.1016/j.autrev.2009.01.012. DOI: 10.1016/j.autrev.2009.01.012. PMID: 19189867.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A study on the affecting factors on root resorption
- Changes in the titer of tooth root antibodies accompanying root resorption associated with orthodontic tooth movement
- Mechanisms of Osteoclastogenesis in Orthodontic Tooth Movement and Orthodontically Induced Tooth Root Resorption
- Effect of vitamin C deficiency on the rate of orthodontic tooth movement and alveolar bone remodeling
- A study on the pattern of the root resorption following maxillary incisor retraction