Obstet Gynecol Sci.
2024 Jan;67(1):58-66. 10.5468/ogs.23154.
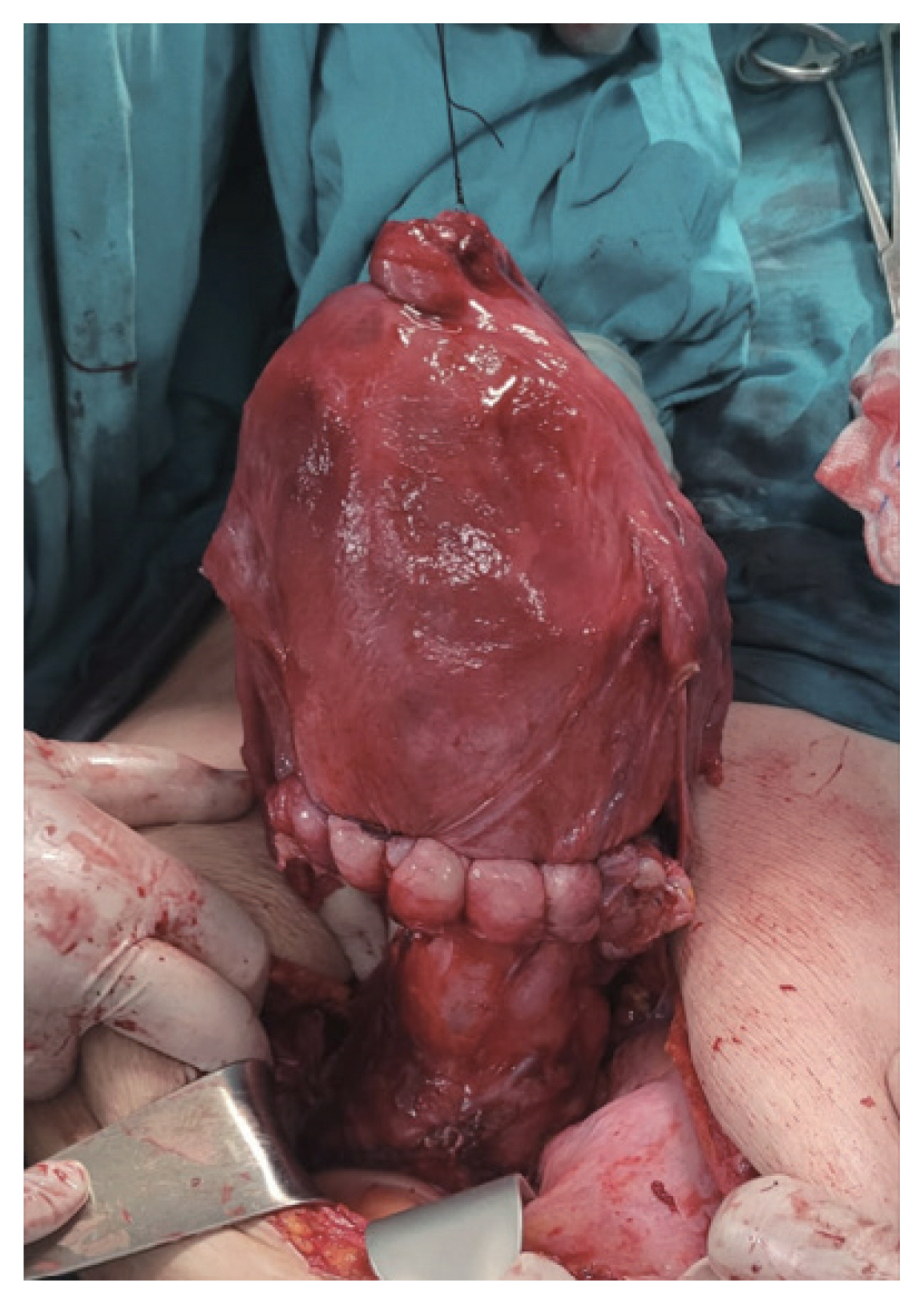
Fetal and maternal outcomes of segmental uterine resection in emergency and planned placenta percreta deliveries
- Affiliations
-
- 1Division of Perinatology, Department of Obstetrics and Gynecology, Necmettin Erbakan University Medical School of Meram, Konya, Turkey
- 2Department of Obstetrics and Gynecology, Necmettin Erbakan University Medical School of Meram, Konya, Turkey
- 3Department of public health, Necmettin Erbakan University Medical School of Meram, Konya, Turkey
- KMID: 2550486
- DOI: http://doi.org/10.5468/ogs.23154
Abstract
Objective
This study evaluated maternal and fetal outcomes of emergency uterine resection versus planned segmental uterine resection in patients with placenta percreta (PPC) and placenta previa (PP).
Methods
Patients with PP and PPC who underwent planned or emergency segmental uterine resection were included in this study. Demographic data, hemorrhagic morbidities, intra- and postoperative complications, length of hospital stay, surgical duration, and peri- and neonatal morbidities were compared.
Results
A total of 141 PPC and PP cases were included in this study. Twenty-five patients (17.73%) underwent emergency uterine resection, while 116 (82.27%) underwent planned segmental uterine resections. The postoperative hemoglobin changes, operation times, total blood transfusion, bladder injury, and length of hospital stay did not differ significantly between groups (P=0.7, P=0.6, P=0.9, P=0.9, and P=0.2, respectively). Fetal weights, 5-minute Apgar scores, and neonatal intensive care unit admission rates did not differ significantly between groups. The gestational age at delivery of patients presenting with bleeding was lower than that of patients who were admitted in active labor and underwent elective surgery (32 weeks [95% confidence interval [CI], 26-37] vs. 35 weeks [95% CI, 34-35]; P=0.037).
Conclusion
Using a multidisciplinary approach, this study performed at a tertiary center showed that maternal and fetal morbidity and mortality did not differ significantly between emergency versus planned segmental uterine resection.
Keyword
Figure
Reference
-
References
1. Mogos MF, Salemi JL, Ashley M, Whiteman VE, Salihu HM. Recent trends in placenta accreta in the United States and its impact on maternal-fetal morbidity and healthcare-associated costs, 1998–2011. J Matern Fetal Neonatal Med. 2016; 29:1077–82.2. Jauniaux E, Bunce C, Grønbeck L, Langhoff-Roos J. Prevalence and main outcomes of placenta accreta spectrum: a systematic review and meta-analysis. Am J Obstet Gynecol. 2019; 221:208–18.3. Goffman D, Nathan L, Chazotte C. Obstetric hemorrhage: a global review. Semin Perinatol. 2016; 40:96–8.4. Erfani H, Kassir E, Fox KA, Clark SL, Karbasian N, Salmanian B, et al. Placenta previa without morbidly adherent placenta: comparison of characteristics and outcomes between planned and emergent deliveries in a tertiary center. J Matern Fetal Neonatal Med. 2019; 32:906–9.5. Durukan H, Durukan ÖB, Yazıcı FG. Planned versus urgent deliveries in placenta previa: maternal, surgical and neonatal results. Arch Gynecol Obstet. 2019; 300:1541–9.6. Jauniaux E, Kingdom JC, Silver RM. A comparison of recent guidelines in the diagnosis and management of placenta accreta spectrum disorders. Best Pract Res Clin Obstet Gynaecol. 2021; 72:102–16.7. Acar A, Ercan F, Pekin A, Elci Atilgan A, Sayal HB, Balci O, et al. Conservative management of placental invasion anomalies with an intracavitary suture technique. Int J Gynaecol Obstet. 2018; 143:184–90.8. Varlas VN, Bors RG, Birsanu S, Maxim B, Clotea E, Mihailov M. Maternal and fetal outcome in placenta accreta spectrum (PAS) associated with placenta previa: a retrospective analysis from a tertiary center. J Med Life. 2021; 14:367–75.9. Obstetric care consensus no. 7: placenta accreta spectrum. Obstet Gynecol. 2018; 132:e259–75.10. Daney de Marcillac F, Lecointre L, Guillaume A, Sananes N, Fritz G, Viville B, et al. Maternal morbidity and mortality associated with conservative management for placenta morbidly adherent (accreta) diagnosed during pregnancy. Report of 15 cases. J Gynecol Obstet Biol Reprod (Paris). 2016; 45:849–58.11. Pegu B, Thiagaraju C, Nayak D, Subbaiah M. Placenta accreta spectrum-a catastrophic situation in obstetrics. Obstet Gynecol Sci. 2021; 64:239–47.12. Ma Y, Liu R, Zhang J, Chen Y. An analysis of maternal-fetal prognosis in patients with placenta accreta. J Matern Fetal Neonatal Med. 2021; 34:725–31.13. Shamshirsaz AA, Fox KA, Erfani H, Clark SL, Shamshirsaz AA, Nassr AA, et al. Outcomes of planned compared with urgent deliveries using a multidisciplinary team approach for morbidly adherent placenta. Obstet Gynecol. 2018; 131:234–41.14. Morlando M, Schwickert A, Stefanovic V, Gziri MM, Pateisky P, Chalubinski KM, et al. Maternal and neonatal outcomes in planned versus emergency cesarean delivery for placenta accreta spectrum: a multinational database study. Acta Obstet Gynecol Scand. 2021; 100(Suppl 1):41–9.15. Jauniaux E, Chantraine F, Silver RM, Langhoff-Roos J. FIGO consensus guidelines on placenta accreta spectrum disorders: epidemiology. Int J Gynaecol Obstet. 2018; 140:265–73.16. Doğru Ş, Atcı AA, Akkuş F, Eren G, Acar A. Use of ureteral catheter in uterine-sparing surgery for placenta accreta. Perinat J. 2022; 30:158–64.17. Dawood AS, Elgergawy AE, Elhalwagy AE. Evaluation of three-step procedure (Shehata’s technique) as a conservative management for placenta accreta at a tertiary care hospital in Egypt. J Gynecol Obstet Hum Reprod. 2019; 48:201–5.18. Kilicci C, Ozkaya E, Eser A, Bostanci EE, Sanverdi I, Abide Yayla C, et al. Planned cesarean hysterectomy versus modified form of segmental resection in patients with placenta percreta. J Matern Fetal Neonatal Med. 2018; 31:2935–40.19. Karaman E, Kolusarı A, Çetin O, Çim N, Alkış İ, Yıldızhan R, et al. Local resection may be a strong alternative to cesarean hysterectomy in conservative surgical management of placenta percreta: experiences from a tertiary hospital. J Matern Fetal Neonatal Med. 2017; 30:947–52.20. Jolley JA, Nageotte MP, Wing DA, Shrivastava VK. Management of placenta accreta: a survey of maternal-fetal medicine practitioners. J Matern Fetal Neonatal Med. 2012; 25:756–60.21. Eller AG, Bennett MA, Sharshiner M, Masheter C, Soisson AP, Dodson M, et al. Maternal morbidity in cases of placenta accreta managed by a multidisciplinary care team compared with standard obstetric care. Obstet Gynecol. 2011; 117:331–7.22. Shamshirsaz AA, Fox KA, Erfani H, Clark SL, Salmanian B, Baker BW, et al. Multidisciplinary team learning in the management of the morbidly adherent placenta: outcome improvements over time. Am J Obstet Gynecol. 2017; 216:612.e1–5.23. Thang NM, Anh NTH, Thanh PH, Linh PT, Cuong TD. Emergent versus planned delivery in patients with placenta accreta spectrum disorders: a retrospective study. Medicine (Baltimore). 2021; 100:e28353.24. Bowman ZS, Manuck TA, Eller AG, Simons M, Silver RM. Risk factors for unscheduled delivery in patients with placenta accreta. Am J Obstet Gynecol. 2014; 210:241.e1–6.25. Wang Y, Zeng L, Niu Z, Chong Y, Zhang A, Mol B, et al. An observation study of the emergency intervention in placenta accreta spectrum. Arch Gynecol Obstet. 2019; 299:1579–86.26. Flores-Mendoza H, Chandran AR, Hernandez-Nieto C, Murji A, Allen L, Windrim RC, et al. Outcomes in emergency versus electively scheduled cases of placenta accreta spectrum disorder managed by cesarean-hysterectomy within a multidisciplinary care team. Int J Gynaecol Obstet. 2022; 159:404–11.27. Warshak CR, Ramos GA, Eskander R, Benirschke K, Saenz CC, Kelly TF, et al. Effect of predelivery diagnosis in 99 consecutive cases of placenta accreta. Obstet Gynecol. 2010; 115:65–9.28. Erfani H, Fox KA, Clark SL, Rac M, Rocky Hui SK, Rezaei A, et al. Maternal outcomes in unexpected placenta accreta spectrum disorders: single-center experience with a multidisciplinary team. Am J Obstet Gynecol. 2019; 221:337.e1–5.29. Meller CH, Izbizky GH, Otaño L. Timing of delivery in placenta accreta. Am J Obstet Gynecol. 2014; 211:438–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spontaneous uterine rupture from placenta percreta at 33 weeks' gestation after a single gynecologic surgery
- A Case of Spontaneous Uterine Rupture due to Placenta Percreta on 1st Trimester
- A Case of Placenta Percreta Involving the Urinary Bladder
- A Case of Spontaneous Uterine Rupture in 17 Weeks of Pregnancy
- Spontaneous Uterine Rupture with Placenta Percreta