Korean J Pain.
2024 Jan;37(1):51-58. 10.3344/kjp.23254.
Comparison of international medical costs for interventional pain treatment: a focus on Korea and Japan
- Affiliations
-
- 1Health Insurance Review and Assessment Service, Gwangju, Korea
- 2Department of Anatomy, Wonkwang University School of Medicine, Iksan, Korea
- 3Jesaeng-Euise Clinical Anatomy Center, Wonkwang University School of Medicine, Iksan, Korea
- 4Sarcopenia Total Solution Center, Wonkwang University School of Medicine, Iksan, Korea
- 5Department of Anesthesiology and Pain Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 6Department of Anesthesiology and Pain Medicine, Wonkwang University School of Medicine, Wonkwang University Hospital, Iksan, Korea
- KMID: 2550132
- DOI: http://doi.org/10.3344/kjp.23254
Abstract
- Background
The rise in national health care costs has emerged as a global problem given the ever-aging population and rapid development of medical technology. The utilization of interventional pain management has, similarly, shown a continued rise worldwide. This study evaluates the differences in the medical costs in the field of interventional pain treatment (IPT) between two countries: Korea and Japan.
Methods
Korean medical insurance costs for 2019 related to pain management focused on IPT were compared to those of Japan. Purchasing power parity (PPP) was used to adjust the exchange rate differences and to compare prices in consideration of the respective societies’ economic power.
Results
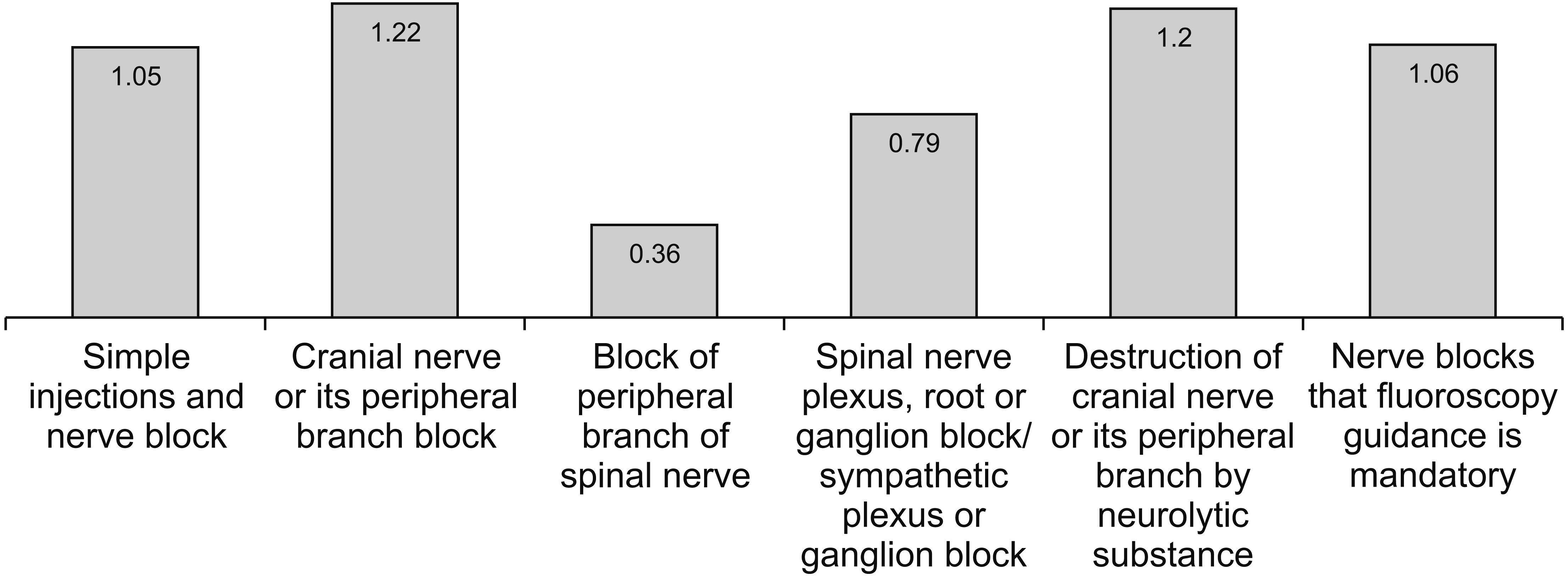
The cost of trigger point injections in Japan was 1.06 times higher than that of Korea, whereas the perineural and intraarticular injection prices were lower in Japan. The cost of epidural blocks was higher in Japan compared to Korea in both cervical/thoracic and lumbar regions. As for blocks of peripheral branches of spinal nerves, the cost of scapular nerve blocks in Japan was lower than that in Korea, given a PPP ratio 0.09. For nerve blocks in which fluoroscopy guidance is mandatory, the costs of epidurography in Japan were greater than those in Korea, given a PPP ratio 1.04.
Conclusions
This is the first comparative study focusing on the medical costs related to IPT between Korea and Japan, which reveals that the costs differed along various categories. Further comparisons reflecting more diverse countries and socio-economic aspects will be required.
Keyword
Figure
Reference
-
1. Shin SM. 2023; Household catastrophic health expenditure related to pain in Korea. Korean J Pain. 36:347–57. DOI: 10.3344/kjp.23041. PMID: 37340630. PMCID: PMC10322657.2. Ma CA. 1994; Health care payment systems: cost and quality incentives. J Econ Manage Strat. 3:93–112. DOI: 10.1111/j.1430-9134.1994.00093.x.3. Kim H, Lee CH, Kim SH, Kim YD. 2018; Epidemiology of complex regional pain syndrome in Korea: an electronic population health data study. PLoS One. 13:e0198147. Erratum in: PLoS One 2018; 13: e0201327. DOI: 10.1371/journal.pone.0198147. PMID: 29864152. PMCID: PMC5986148. PMID: f066ffbc940a443b8e58e5f666206070.4. Park S. 2021; Medical service utilization and out-of-pocket spending among near-poor National Health Insurance members in South Korea. BMC Health Serv Res. 21:886. DOI: 10.1186/s12913-021-06881-8. PMID: 34454499. PMCID: PMC8399721. PMID: 9b6db033937c42bb879e6075933ce78e.5. Lee JH, Song J, Kuk YH, Ha JR, Kim YD. 2020; Dispute cases related to pain management in Korea: analysis of Korea Medical Dispute Mediation and Arbitration Agency data. Anesth Pain Med (Seoul). 15:96–102. DOI: 10.17085/apm.2020.15.1.96. PMID: 33329797. PMCID: PMC7713854. PMID: e7130962e7904fab8002f66c97e44bd0.6. Manchikanti L, Kaye AD, Latchaw RE, Sanapati MR, Pampati V, Gharibo CG, et al. 2023; Impact of the COVID-19 pandemic on utilization patterns of facet joint interventions in managing spinal pain in a Medicare population. Pain Ther. 12:505–27. DOI: 10.1007/s40122-023-00476-3. PMID: 36723804. PMCID: PMC9890434. PMID: 60042cdb77e04835b7ca441829488bfc.7. Manchikanti L, Pampati V, Sanapati MR, Kosanovic R, Beall DP, Atluri S, et al. 2022; COVID-19 pandemic reduced utilization of interventional techniques 18.7% in managing chronic pain in the Medicare population in 2020: analysis of utilization data from 2000 to 2020. Pain Physician. 25:223–38. PMID: 35652763.8. Manchikanti L, Pampati V, Soin A, Sanapati MR, Kaye AD, Hirsch JA. 2021; Declining utilization and inflation-adjusted expenditures for epidural procedures in chronic spinal pain in the Medicare population. Pain Physician. 24:1–15. PMID: 33400424.9. Manchikanti L, Pampati V, Soin A, Vanaparthy R, Sanapati MR, Kaye AD, et al. 2020; Trends of expenditures and utilization of facet joint interventions in fee-for-service (FFS) Medicare population from 2009-2018. Pain Physician. 23:S129–47. DOI: 10.36076/ppj.2020/23/S129. PMID: 32503360.10. Manchikanti L, Pampati V, Vangala BP, Soin A, Sanapati MR, Thota S, et al. 2021; Spinal cord stimulation trends of utilization and expenditures in fee-for-service (FFS) Medicare population from 2009 to 2018. Pain Physician. 24:293–308. DOI: 10.36076/ppj.2021.24.401. PMID: 34323431.11. Manchikanti L, Sanapati MR, Pampati V, Soin A, Atluri S, Kaye AD, et al. 2020; Update of utilization patterns of facet joint interventions in managing spinal pain from 2000 to 2018 in the US fee-for-service Medicare population. Pain Physician. 23:E133–49. DOI: 10.36076/ppj.2020/23/E133. PMID: 32214289.12. Lee MR, Lee YH, Koh KW. 2005; The change of medical care pattern and cost of cataract surgery by the DRG payment system in a general hospital. J Korea Soc Hosp Admin. 10:48–70.13. Shin J. 2012; Private health insurance in South Korea: an international comparison. Health Policy. 108:76–85. DOI: 10.1016/j.healthpol.2012.08.011. PMID: 22958939.14. Dronina Y, Yoon YM, Sakamaki H, Nam EW. 2016; Health system development and performance in Korea and Japan:. a comparative study of 2000-2013. J Lifestyle Med. 6:16–26. DOI: 10.15280/jlm.2016.6.1.16. PMID: 27358836. PMCID: PMC4915763.15. Kim HT, Kim SY, Byun GJ, Shin BC, Lee JY, Choi EJ, et al. 2017; State of education regarding ultrasound-guided interventions during pain fellowships in Korea: a survey of recent fellows. Korean J Pain. 30:287–95. DOI: 10.3344/kjp.2017.30.4.287. PMID: 29123624. PMCID: PMC5665741.16. Kim YD. 2021; Necessity of an exact anatomical understanding for the better pain practice. Korean J Pain. 34:373–4. DOI: 10.3344/kjp.2021.34.4.373. PMID: 34593655. PMCID: PMC8494956.17. Lee SH, Yang M, Won HS, Kim YD. 2023; Coccydynia: anatomic origin and considerations regarding the effectiveness of injections for pain management. Korean J Pain. 36:272–80. DOI: 10.3344/kjp.23175. PMID: 37394271. PMCID: PMC10322656.18. Kim YD, Moon HS. 2015; Review of medical dispute cases in the pain management in Korea: a medical malpractice liability insurance database study. Korean J Pain. 28:254–64. Erratum in: Korean J Pain 2016; 29: 62. DOI: 10.3344/kjp.2015.28.4.254. PMID: 26495080. PMCID: PMC4610939.19. Manchikanti L, Knezevic NN, Navani A, Christo PJ, Limerick G, Calodney AK, et al. 2021; Epidural interventions in the management of chronic spinal pain: American Society of Interventional Pain Physicians (ASIPP) comprehensive evidence-based guidelines. Pain Physician. 24:S27–208. DOI: 10.36076/ppj.2021.24.S27-S208. PMID: 33492918.20. Bogduk N. 2002; Diagnostic nerve blocks in chronic pain. Best Pract Res Clin Anaesthesiol. 16:565–78. DOI: 10.1053/bean.2002.0252. PMID: 12516892.21. Hogan QH, Abram SE. 1997; Neural blockade for diagnosis and prognosis. A review. Anesthesiology. 86:216–41. DOI: 10.1097/00000542-199701000-00026. PMID: 9009957.22. Naidu RK, Chaturvedi R, Engle AM, Mehta P, Su B, Chakravarthy K, et al. 2021; Interventional spine and pain procedure credentialing: guidelines from the American Society of Pain & Neuroscience. J Pain Res. 14:2777–91. DOI: 10.2147/JPR.S309705. PMID: 34531681. PMCID: PMC8439288.23. Doo AR, Kim JW, Lee JH, Han YJ, Son JS. 2015; A comparison of two techniques for ultrasound-guided caudal injection: the influence of the depth of the inserted needle on caudal block. Korean J Pain. 28:122–8. DOI: 10.3344/kjp.2015.28.2.122. PMID: 25852834. PMCID: PMC4387457.24. Yoo SW, Ki MJ, Doo AR, Woo CJ, Kim YS, Son JS. 2021; Prediction of successful caudal epidural injection using color Doppler ultrasonography in the paramedian sagittal oblique view of the lumbosacral spine. Korean J Pain. 34:339–45. DOI: 10.3344/kjp.2021.34.3.339. PMID: 34193640. PMCID: PMC8255148.25. Park S, Kim M, Kim JH. 2022; Radiation safety for pain physicians: principles and recommendations. Korean J Pain. 35:129–39. DOI: 10.3344/kjp.2022.35.2.129. PMID: 35354676. PMCID: PMC8977205.26. Dagenais S, Caro J, Haldeman S. 2008; A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. 8:8–20. DOI: 10.1016/j.spinee.2007.10.005. PMID: 18164449.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Interventional management for postoperative arterial bleeding in gastrointestinal surgery
- Comparison of Medical Education and Requirements for Training in the Interventional Neuroradiology in China, Japan and Korea
- The Deep Dry Needling Techniques, and Interventional Muscle and Nerve Stimulation (IMS) for the Treatment of Chronic Pain
- The role of lymphatic interventional radiology for postoperative lymphorrhea
- Interventional Treatment of Low Back Pain