Prog Med Phys.
2023 Dec;34(4):41-47. 10.14316/pmp.2023.34.4.41.
Dosimetric Comparison of Three-Dimensional Conformal, Intensity-Modulated Radiotherapy, Volumetric Modulated Arc Therapy, and Dynamic Conformal Arc Therapy Techniques in Prophylactic Cranial Irradiation
- Affiliations
-
- 1Department of Radiation Oncology, Istanbul Yeni Yüzyil University Gaziosmanpaşa Hospital, Istanbul, Turkey
- 2Department of Radiation Oncology, Vocational School of Health Services, Istanbul Medipol University, Istanbul, Turkey
- KMID: 2550124
- DOI: http://doi.org/10.14316/pmp.2023.34.4.41
Abstract
- Purpose
This study aimed to dosimetrically compare the technique of three-dimensional conformal radiotherapy (3D CRT), which is a traditional prophylactic cranial irradiation method, and the intensity-modulated radiotherapy (IMRT) and volumetric modulated arc therapy (VMAT) techniques used in the last few decades with the dynamic conformal arc therapy (DCAT) technique.
Methods
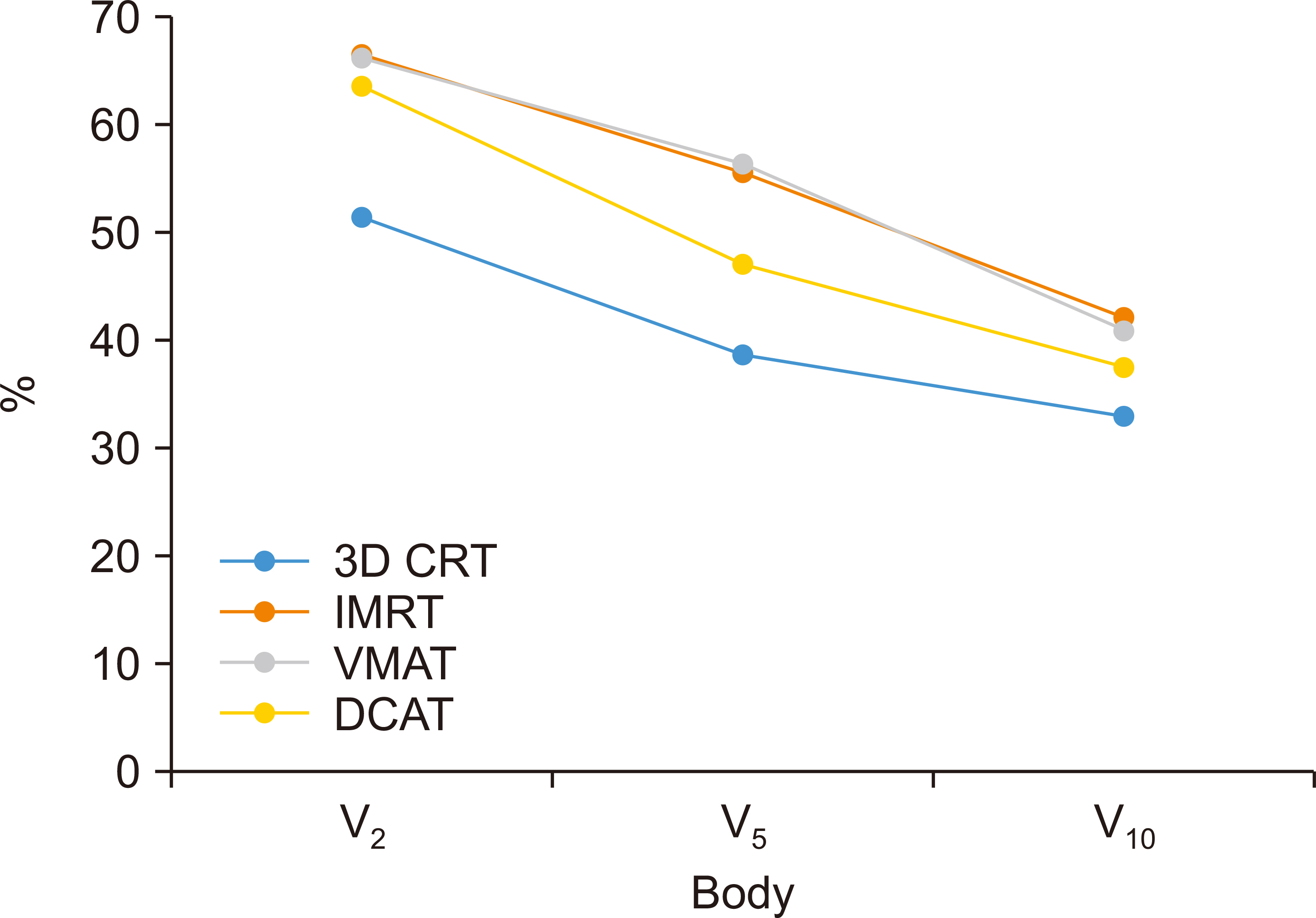
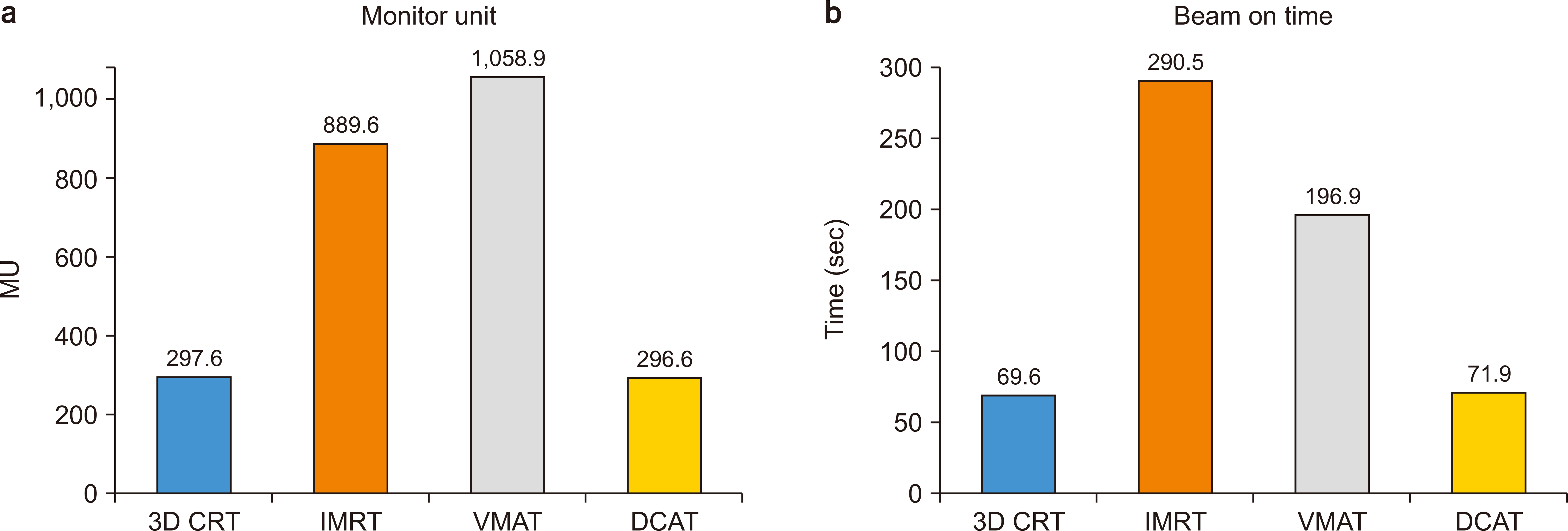
The 3D CRT, VMAT, IMRT, and DCAT plans were prepared with 25 Gy in 10 fractions in a Monaco planning system. The target volume and the critical organ doses were compared. A comparison of the body V2, V5, and V10 doses, monitor unit (MU), and beam on-time values was also performed.
Results
In planned target volume of the brain (PTVBrain), the highest D99 dose value (P<0.001) and the most homogeneous (P =0.049) dose distribution according to the heterogeneity index were obtained using the VMAT technique. In contrast, the lowest values were obtained using the 3D CRT technique in the body V2, V5, and V10 doses. The MU values were the lowest when DCAT (P =0.001) was used. These values were 0.34% (P =0.256) lower with the 3D CRT technique, 66% (P =0.001) lower with IMRT, and 72% (P =0.001) lower with VMAT. The beam on-time values were the lowest with the 3D CRT planning (P<0.001), 3.8% (P =0.008) lower than DCAT, 65% (P =0.001) lower than VMAT planning, and 76% (P =0.001) lower than IMRT planning.
Conclusions
Without sacrificing the homogeneous dose distribution and the critical organ doses in IMRTs, three to four times less treatment time, less low-dose volume, less leakage radiation, and less radiation scattering could be achieved when the DCAT technique is used similar to conventional methods. In short, DCAT, which is applicable in small target volumes, can also be successfully planned in large target volumes, such as the whole-brain.
Keyword
Figure
Reference
-
References
1. van Meerbeeck JP, Fennell DA, De Ruysscher DK. 2011; Small-cell lung cancer. Lancet. 378:1741–1755. DOI: 10.1016/S0140-6736(11)60165-7. PMID: 21565397.
Article2. Manapov F, Käsmann L, Roengvoraphoj O, Dantes M, Schmidt-Hegemann NS, Belka C, et al. 2018; Prophylactic cranial irradiation in small-cell lung cancer: update on patient selection, efficacy and outcomes. Lung Cancer (Auckl). 9:49–55. DOI: 10.2147/LCTT.S137577. PMID: 30323698. PMCID: PMC6181088.
Article3. Seute T, Leffers P, ten Velde GP, Twijnstra A. 2004; Neurologic disorders in 432 consecutive patients with small cell lung carcinoma. Cancer. 100:801–806. DOI: 10.1002/cncr.20043. PMID: 14770437.
Article4. Hirsch FR, Paulson OB, Hansen HH, Vraa-Jensen J. 1982; Intracranial metastases in small cell carcinoma of the lung: correlation of clinical and autopsy findings. Cancer. 50:2433–2437. DOI: 10.1002/1097-0142(19821201)50:11<2433::AID-CNCR2820501131>3.0.CO;2-E. PMID: 6182974.
Article5. Aupérin A, Arriagada R, Pignon JP, Le Péchoux C, Gregor A, Stephens RJ, et al. 1999; Prophylactic cranial irradiation for patients with small-cell lung cancer in complete remission. Prophylactic cranial irradiation overview collaborative group. N Engl J Med. 341:476–484. DOI: 10.1056/NEJM199908123410703. PMID: 10441603.
Article6. Slotman B, Faivre-Finn C, Kramer G, Rankin E, Snee M, Hatton M, et al. 2007; Prophylactic cranial irradiation in extensive small-cell lung cancer. N Engl J Med. 357:664–672. DOI: 10.1056/NEJMoa071780. PMID: 17699816.
Article7. Bernhardt D, Bozorgmehr F, Adeberg S, Opfermann N, von Eiff D, Rieber J, et al. 2016; Outcome in patients with small cell lung cancer re-irradiated for brain metastases after prior prophylactic cranial irradiation. Lung Cancer. 101:76–81. DOI: 10.1016/j.lungcan.2016.09.010. PMID: 27794411.
Article8. Ramlov A, Tietze A, Khalil AA, Knap MM. 2012; Prophylactic cranial irradiation in patients with small cell lung cancer. A retrospective study of recurrence, survival and morbidity. Lung Cancer. 77:561–566. DOI: 10.1016/j.lungcan.2012.05.101. PMID: 22677428.
Article9. Scharp M, Hauswald H, Bischof M, Debus J, Combs SE. 2014; Re-irradiation in the treatment of patients with cerebral metastases of solid tumors: retrospective analysis. Radiat Oncol. 9:4. DOI: 10.1186/1748-717X-9-4. PMID: 24387239. PMCID: PMC3904456.
Article10. Kirakli EK, Gayaf M, Deniz S, Bozkurt T, Yılmaz U, Kömürcüoğlu B. 2018; The role of reirredation in recurrences after prophylactic cranial irradiation in small cell lung cancer: is it necessary? Göğüs Hastanesi Dergisi. 32:83–89.11. Otto K. 2008; Volumetric modulated arc therapy: IMRT in a single gantry arc. Med Phys. 35:310–317. DOI: 10.1118/1.2818738. PMID: 18293586.
Article12. Durmus IF, Okumus A. 2022; Dosimetric comparison of mDCAT and VMAT techniques according to 6MV-FFF and 10MV-FFF energies in patients with single adrenal metastasis. J Xray Sci Technol. 30:1023–1032. DOI: 10.3233/XST-221192. PMID: 35848004.
Article13. Kataria T, Sharma K, Subramani V, Karrthick KP, Bisht SS. 2012; Homogeneity Index: an objective tool for assessment of conformal radiation treatments. J Med Phys. 37:207–213. DOI: 10.4103/0971-6203.103606. PMID: 23293452. PMCID: PMC3532749.
Article14. Li J, Tang XB, Wang BH, Chen XM, Chen D, Chai L. 2016; Comparison between dual arc VMAT and 7F-IMRT in the protection of hippocampus for patients during whole brain radiotherapy. J Xray Sci Technol. 24:457–466. DOI: 10.3233/XST-160561. PMID: 27257881.
Article15. Marsh JC, Godbole R, Diaz AZ, Gielda BT, Turian JV. 2011; Sparing of the hippocampus, limbic circuit and neural stem cell compartment during partial brain radiotherapy for glioma: a dosimetric feasibility study. J Med Imaging Radiat Oncol. 55:442–449. DOI: 10.1111/j.1754-9485.2011.02282.x. PMID: 21843181.
Article16. Marsh JC, Godbole RH, Herskovic AM, Gielda BT, Turian JV. 2010; Sparing of the neural stem cell compartment during whole-brain radiation therapy: a dosimetric study using helical tomotherapy. Int J Radiat Oncol Biol Phys. 78:946–954. DOI: 10.1016/j.ijrobp.2009.12.012. PMID: 20472348.
Article17. Emami B, Lyman J, Brown A, Coia L, Goitein M, Munzenrider JE, et al. 1991; Tolerance of normal tissue to therapeutic irradiation. Int J Radiat Oncol Biol Phys. 21:109–122. DOI: 10.1016/0360-3016(91)90171-Y. PMID: 2032882.
Article18. Wang JZ, Li XA, D'Souza WD, Stewart RD. 2003; Impact of prolonged fraction delivery times on tumor control: a note of caution for intensity-modulated radiation therapy (IMRT). Int J Radiat Oncol Biol Phys. 57:543–552. DOI: 10.1016/S0360-3016(03)00499-1. PMID: 12957268.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dosimetric comparison between modulated arc therapy and static intensity modulated radiotherapy in thoracic esophageal cancer: a single institutional experience
- Benefit of volumetric-modulated arc therapy over three-dimensional conformal radiotherapy for stage I-II extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue in the stomach: a dosimetric comparison
- Intensity-modulated radiation therapy: a review with a physics perspective
- Introduction of intensity modulated radiation therapy
- Dosimetric comparison of intensity-modulated radiotherapy (IMRT) and volumetric modulated arc therapy (VMAT) in total scalp irradiation: a single institutional experience