Nutr Res Pract.
2023 Dec;17(6):1143-1154. 10.4162/nrp.2023.17.6.1143.
Association between body shape misperception and unhealthy eating behaviors among Korean adolescents
- Affiliations
-
- 1Department of Public Health, Graduate School, Yonsei University, Seoul 03722, Korea
- 2Department of Healthcare Management, Graduate School of Public Health, Yonsei University, Seoul 03722, Korea
- 3Department of Preventive Medicine, College of Medicine, Yonsei University, Seoul 03722, Korea
- KMID: 2548870
- DOI: http://doi.org/10.4162/nrp.2023.17.6.1143
Abstract
- BACKGROUND/OBJECTIVES
Body shape misperception (BSM) is the disagreement between the subjectively perceived body size and body mass index. This study investigated the association between BSM and unhealthy eating behaviors (UEB) among Korean adolescents.
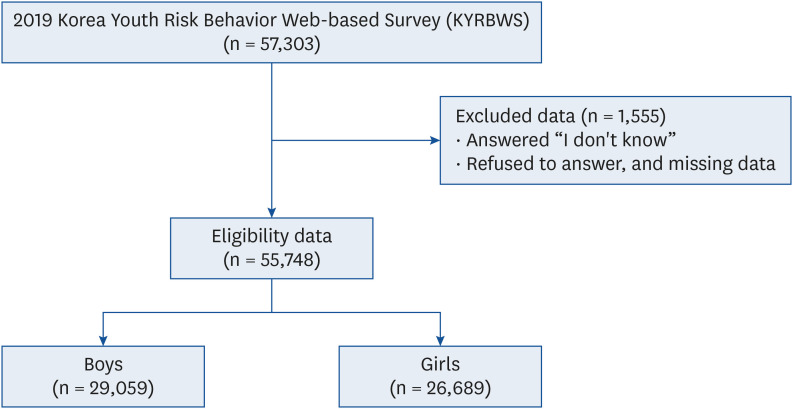
SUBJECTS/METHODS
This cross-sectional study used data from the 2019 Korea Youth Risk Behavior Web-based Survey with 55,748 participants. UEB were measured according to the weekly consumption frequency of caffeinated energy drinks, fast food, carbonated beverages, and sugar-sweetened beverages. The covariates included demographic and socioeconomic characteristics and health-related factors. Multiple logistic regression analysis determined the association between BSM and UEB.
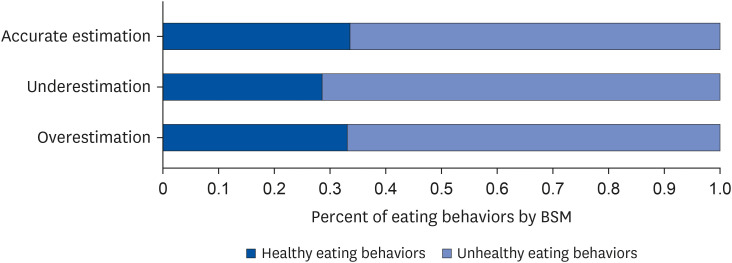
RESULTS
Among the participants, 37,607 (67.5%) reported UEB. The gap between UEB among those with BSM was the largest between the underestimated and accurately estimated groups. Participants who underestimated their body shape were likelier to engage in UEB (adjusted odds ratio [AOR], 1.18; 95% confidence interval [CI], 1.11–1.25). Both sexes with underestimation of body size showed an association with UEB compared to those with accurate estimations (girls: AOR, 1.19; 95% CI, 1.09–1.30; boys: AOR, 1.16; 95% CI, 1.08–1.26).
CONCLUSIONS
Underestimating body shape can provoke UEB among Korean adolescents. The need for appropriate school health interventional programs to prevent underestimating body shape is emphasized to avoid UEB.
Figure
Reference
-
1. Eisenmann JC. Secular trends in variables associated with the metabolic syndrome of North American children and adolescents: a review and synthesis. Am J Hum Biol. 2003; 15:786–794. PMID: 14595870.2. Moreno LA, Rodriguez G, Fleta J, Bueno-Lozano M, Lazaro A, Bueno G. Trends of dietary habits in adolescents. Crit Rev Food Sci Nutr. 2010; 50:106–112. PMID: 20112152.3. Hong CH. Current health issues in Korean adolescents. Korean J Pediatr. 2011; 54:395–400. PMID: 22232620.4. Bucher Della Torre S, Keller A, Laure Depeyre J, Kruseman M. Sugar-sweetened beverages and obesity risk in children and adolescents: a systematic analysis on how methodological quality may influence conclusions. J Acad Nutr Diet. 2016; 116:638–659. PMID: 26194333.5. Sami W, Ansari T, Butt NS, Hamid MRA. Effect of diet on type 2 diabetes mellitus: a review. Int J Health Sci (Qassim). 2017; 11:65–71.6. Park E, Ko Y. Trends in obesity and obesity-related risk factors among adolescents in Korea from 2009 to 2019. Int J Environ Res Public Health. 2022; 19:5672. PMID: 35565066.7. Pereira MA, Kartashov AI, Ebbeling CB, Van Horn L, Slattery ML, Jacobs DR Jr, Ludwig DS. Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis. Lancet. 2005; 365:36–42. PMID: 15639678.8. Martin-Calvo N, Martínez-González MA, Bes-Rastrollo M, Gea A, Ochoa MC, Marti A. GENOI Members. Sugar-sweetened carbonated beverage consumption and childhood/adolescent obesity: a case-control study. Public Health Nutr. 2014; 17:2185–2193. PMID: 24485091.9. van Dam RM, Hu FB, Willett WC. Coffee, caffeine, and health. N Engl J Med. 2020; 383:369–378. PMID: 32706535.10. Liechty JM, Lee MJ. Body size estimation and other psychosocial risk factors for obesity onset among US adolescents: findings from a longitudinal population level study. Int J Obes. 2015; 39:601–607.11. Ali MM, Fang H, Rizzo JA. Body weight, self-perception and mental health outcomes among adolescents. J Ment Health Policy Econ. 2010; 13:53–63. PMID: 20919592.12. Phelps L, Johnston LS, Jimenez DP, Wilczenski FL, Andrea RK, Healy RW. Figure preference, body dissatisfaction, and body distortion in adolescence. J Adolesc Res. 1993; 8:297–310.13. Kim DS, Kim HS, Cho Y, Cho SI. The effects of actual and perceived body weight on unhealthy weight control behaviors and depressed mood among adult women in Seoul, Korea. J Prev Med Public Health. 2008; 41:323–330. PMID: 18827500.14. Lim H, Wang Y. Body weight misperception patterns and their association with health-related factors among adolescents in South Korea. Obesity (Silver Spring). 2013; 21:2596–2603. PMID: 23512737.15. Sonneville KR, Thurston IB, Milliren CE, Gooding HC, Richmond TK. Weight misperception among young adults with overweight/obesity associated with disordered eating behaviors. Int J Eat Disord. 2016; 49:937–946. PMID: 27218865.16. Lee JH, Lee HS, Kim H, Kwon YJ, Shin J, Lee JW. Association between nutrition education, dietary habits, and body image misperception in adolescents. Asia Pac J Clin Nutr. 2021; 30:512–521. PMID: 34587711.17. Silva SUD, Alves MA, Vasconcelos FAG, Gonçalves VSS, Barufaldi LA, Carvalho KMB. Association between body weight misperception and dietary patterns in Brazilian adolescents: cross-sectional study using ERICA data. PLoS One. 2021; 16:e0257603. PMID: 34555063.18. Yan H, Wu Y, Oniffrey T, Brinkley J, Zhang R, Zhang X, Wang Y, Chen G, Li R, Moore JB. Body weight misperception and its association with unhealthy eating behaviors among adolescents in China. Int J Environ Res Public Health. 2018; 15:936. PMID: 29738429.19. Verzijl CL, Ahlich E, Lang B, Rancourt D. Body mass index as a moderator of the association between weight status misperception and disordered eating behaviors. Eat Behav. 2018; 30:98–103. PMID: 29990654.20. Story M, French SA, Resnick MD, Blum RW. Ethnic/racial and socioeconomic differences in dieting behaviors and body image perceptions in adolescents. Int J Eat Disord. 1995; 18:173–179. PMID: 7581420.21. Heiman T, Olenik-Shemesh D. Perceived body appearance and eating habits: the voice of young and adult students attending higher education. Int J Environ Res Public Health. 2019; 16:451. PMID: 30720728.22. Fischetti F, Latino F, Cataldi S, Greco G. Gender differences in body image dissatisfaction: the role of physical education and sport. J Hum Sport Exerc. 2020; 15:241–250.23. Bovet J. The evolution of feminine beauty. Exploring Transdisciplinarity in art and sciences. 2018; 327–357.24. Sadowska J, Dziaduch I, Bruszkowska M, Ziółkowska K. BMI, body perception, and approach to eating and diet in adolescent girls. SAGE Open. 2020; 10:215824402096281.25. Pope HG Jr, Khalsa JH, Bhasin S. Body image disorders and abuse of anabolic-androgenic steroids among men. JAMA. 2017; 317:23–24. PMID: 27930760.26. Murray SB, Accurso EC, Griffiths S, Nagata JM. Boys, biceps, and bradycardia: the hidden dangers of muscularity-oriented disordered eating. J Adolesc Health. 2018; 62:352–355. PMID: 29241987.27. Nagata JM, Bibbins-Domingo K, Garber AK, Griffiths S, Vittinghoff E, Murray SB. Boys, bulk, and body ideals: sex differences in weight-gain attempts among adolescents in the United States. J Adolesc Health. 2019; 64:450–453. PMID: 30482658.28. Joeng EH, Lee IS. Multilevel analysis of factors associated with subjective weight perception among normal body weight adolescents based on the 2017 Korean Youth’s Risk Behavior Survey (KYRBS). J Korean Acad Community Health Nurs. 2018; 29:476–487.29. Shin J, Choi Y, Han KT, Cheon SY, Kim JH, Lee SG, Park EC. The combined effect of subjective body image and body mass index (distorted body weight perception) on suicidal ideation. J Prev Med Public Health. 2015; 48:94–104. PMID: 25857647.30. Lee SA, Jang SY, Shin J, Ju YJ, Nam JY, Park EC. The association between inappropriate weight control behaviors and suicide ideation and attempt among Korean adolescents. J Korean Med Sci. 2016; 31:1529–1537. PMID: 27550479.31. Ministry of Health and Welfare of Korea, Centers for Disease Control and Prevention, and Ministry of Education. Statistics from the fifteenth Korea Youth Risk Behavior Web-based Survey [Internet]. Cheongju: Korea Centers for Disease Control and Prevention;2019. cited 2022 April 7. Available from: https://www.kdca.go.kr/yhs/.32. Kim Y, Choi S, Chun C, Park S, Khang YH, Oh K. Data resource profile: the Korea Youth Risk Behavior Web-based Survey (KYRBS). Int J Epidemiol. 2016; 45:1076–1076e. PMID: 27380796.33. Lee Y, Jeon YJ, Shim JS, Jung SJ. Association between dietary and suicidal behaviors based on the Youth Risk Behavior Survey (2015–2020). Epidemiol Health. 2022; 44:e2022033. PMID: 35381168.34. Kim JH. Overview of pediatric obesity: diagnosis, epidemiology, and significance. J Korean Med Assoc. 2021; 64:401–409.35. Google. Google trends 2018 [Internet]. Mountain View: Google;2019. cited 2022 June 3. Available from: https://trends.google.com.36. Strand M, Gustafsson SA. Mukbang and disordered eating: a netnographic analysis of online eating broadcasts. Cult Med Psychiatry. 2020; 44:586–609. PMID: 32277331.37. An S, Lim Y, Lee H. A content analysis of eating show (Mukbang) programs on television and online program content in South Korea. Korean J Broadcast Telecommun Stud. 2020; 34:39–79.38. Kim SK, Kim J, Kim H, An S, Lim Y, Park H. Association between food-related media program watching and dietary behaviors in Korean adolescents. Korean Public Health Res. 2020; 46:31–46.39. Gaylis JB, Levy SS, Hong MY. Relationships between body weight perception, body mass index, physical activity, and food choices in Southern California male and female adolescents. Int J Adolesc Youth. 2020; 25:264–275.40. Hernández Camacho JD, Rodríguez Lazo M, Bolaños Ríos P, Ruiz Prieto I, Jáuregui-Lobera I. Eating habits, excess weight and weight self-perception at school. Nutr Hosp. 2015; 32:1334–1343. PMID: 26319858.41. Lu J, Tan C, Zhou J, Sha M, Xu Y, Qiu J, Liu N. Compared with girls, boys’ psychological symptoms are more likely to be influenced by lifestyle in Chinese middle school students. Front Psychol. 2022; 13:899273. PMID: 35874346.42. Rideout V, Robb M. The common sense census: media use by tweens and teens [Internet]. San Francisco: Common Sense Media;2019. cited 2022 June 17. Available from: https://www.commonsensemedia.org/sites/default/files/research/report/2019-census-8-to-18-full-report-updated.pdf.43. Mingoia J, Hutchinson AD, Gleaves DH, Wilson C. The relationship between posting and photo manipulation activities on social networking sites and internalization of a tanned ideal among Australian adolescents and young adults. Social Media + Society. 2019; 5:2056305118820419.44. Pope HG Jr, Gruber AJ, Choi P, Olivardia R, Phillips KA. Muscle dysmorphia. An underrecognized form of body dysmorphic disorder. Psychosomatics. 1997; 38:548–557. PMID: 9427852.45. Thompson JK, Heinberg LJ. The media’s influence on body image disturbance and eating disorders: we’ve reviled them, now can we rehabilitate them? J Soc Issues. 1999; 55:339–353.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Secular Trends for Body-shape Perception, Weight-loss Efforts, and Weight-loss Behaviors in Korean Adults Using the Korea National Health and Nutrition Examination Survey from 2001 to 2014
- Weight misperception and its association with dieting methods and eating behaviors in South Korean adolescents
- Body Weight Perception, Mental Health, and Weight Control Behavior in Normal Weight Adolescents: Based on the Korea National Health and Nutrition Examination Survey 2013-2015
- Gender Differences in the Association between Eating Behavior and Depression of Adolescents: Evidence from a National Korean Cross-sectional Survey
- A survey of body shape perception and weight control of adolescent girls in three areas of Korea