J Korean Med Sci.
2023 Dec;38(47):e402. 10.3346/jkms.2023.38.e402.
Association Between Acid-Suppressive Drugs and Risk of Rosacea: Retrospective Study Using the Korean National Health Insurance ServiceNational Sample Cohort
- Affiliations
-
- 1Department of Gastroenterology and Hepatology, Kangwon National University Hospital, Kangwon National University School of Medicine, Chuncheon, Korea
- 2Department of Dermatology, Kangwon National University Hospital, Kangwon National University School of Medicine, Chuncheon, Korea
- 3Department of Applied Statistics, Korea University Sejong Campus, Sejong, Korea
- 4Division of Allergy and Clinical Immunology, Kangwon National University School of Medicine, Chuncheon, Korea
- KMID: 2548804
- DOI: http://doi.org/10.3346/jkms.2023.38.e402
Abstract
- Background
Rosacea is a common inflammatory skin disease with multiple etiologies. Proton pump inhibitors (PPIs) and histamine-2 receptor antagonists (H2RA) are acid suppressive drugs widely used for gastrointestinal (GI) diseases, and long-term use has been reported to be associated with dysbiosis which is a potential risk for development of rosacea. This study aimed to study the association between rosacea and acid suppressants in the Korean national cohort.
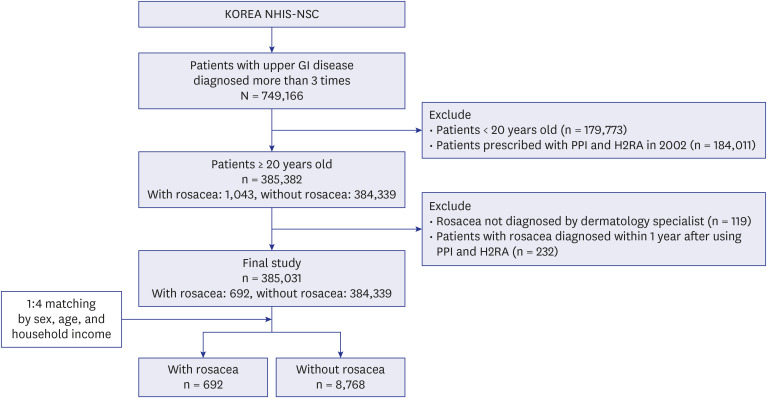
Methods
We used Korean National Health Insurance Service-National Sample Cohort data of 749,166 patients with upper GI diseases between 2001 and 2013. Duration of acid suppressants was compared between patients with and without rosacea together with other sociodemographic characteristics and hazard ratios were estimated.
Results
Longer use of acid suppressants was significantly associated with increased risk of rosacea. After adjustment for possible confounders, increased cumulative defined daily dose was significantly associated with risk of rosacea (odds ratio [OR], 1.55; 95% confidence interval [CI], 1.20–2.00; P = 0.001). Other factors significantly associated with risk of rosacea include residing in the rural area (OR, 2.58; 95% CI, 2.18–3.06; P < 0.001), greater Charlson Comorbidity Index score (OR, 1.45; 95% CI, 1.15–1.83; P = 0.002), and comorbidities (malignancy, thyroid disease, and depression).
Conclusion
Results from our study indicate that H2RA or PPI is associated with the occurrence of rosacea among patients with GI diseases in the Korean population. The risk was increased in dose-dependent manner, even after adjusting for confounding variables. Clinicians should be aware of risks associated with prolonged use of acid suppressive drugs.
Keyword
Figure
Reference
-
1. Pounder R. Histamine H2-receptor antagonists. Baillieres Clin Gastroenterol. 1988; 2(3):593–608. PMID: 2901868.
Article2. Strand DS, Kim D, Peura DA. 25 Years of proton pump inhibitors: a comprehensive review. Gut Liver. 2017; 11(1):27–37. PMID: 27840364.
Article3. Rostom A, Dube C, Wells G, Tugwell P, Welch V, Jolicoeur E, et al. Prevention of NSAID-induced gastroduodenal ulcers. Cochrane Database Syst Rev. 2002; (4):CD002296. PMID: 12519573.
Article4. Singh G, Triadafilopoulos G. Appropriate choice of proton pump inhibitor therapy in the prevention and management of NSAID-related gastrointestinal damage. Int J Clin Pract. 2005; 59(10):1210–1217. PMID: 16178990.
Article5. Savarino V, Tosetti C, Benedetto E, Compare D, Nardone G. Appropriateness in prescribing PPIs: a position paper of the Italian Society of Gastroenterology (SIGE) - study section “Digestive Diseases in Primary Care”. Dig Liver Dis. 2018; 50(9):894–902. PMID: 30093304.
Article6. Vaezi MF, Yang YX, Howden CW. Complications of proton pump inhibitor therapy. Gastroenterology. 2017; 153(1):35–48. PMID: 28528705.
Article7. D’sa FF, Fernandes EZ, Kesarkar SV, Swaminathan L, Kunhikatta V, Rashid M, et al. Use of histamine-2 receptor antagonists and risk of inflammatory bowel diseases: a systematic review and meta-analysis of observational studies. J Clin Pharm Ther. 2022; 47(8):1103–1111. PMID: 35403222.
Article8. Tleyjeh IM, Abdulhak AB, Riaz M, Garbati MA, Al-Tannir M, Alasmari FA, et al. The association between histamine 2 receptor antagonist use and Clostridium difficile infection: a systematic review and meta-analysis. PLoS One. 2013; 8(3):e56498. PMID: 23469173.
Article9. Lin HC, Chen YY, Lin HL, Uang YS, Ho Y, Wang LH. Association between acid-suppressive drug use and atopic dermatitis in patients with upper gastrointestinal diseases: a population-based retrospective cohort study. J Clin Pharm Ther. 2021; 46(3):786–793. PMID: 33403692.
Article10. Hojo M, Asahara T, Nagahara A, Takeda T, Matsumoto K, Ueyama H, et al. Gut microbiota composition before and after use of proton pump inhibitors. Dig Dis Sci. 2018; 63(11):2940–2949. PMID: 29796911.
Article11. Ortigão R, Pimentel-Nunes P, Dinis-Ribeiro M, Libânio D. Gastrointestinal microbiome - what we need to know in clinical practice. Port J Gastroenterol. 2020; 27(5):336–351.
Article12. Ahn CS, Huang WW. Rosacea pathogenesis. Dermatol Clin. 2018; 36(2):81–86. PMID: 29499802.
Article13. Steinhoff M, Schauber J, Leyden JJ. New insights into rosacea pathophysiology: a review of recent findings. J Am Acad Dermatol. 2013; 69(6):Suppl 1. S15–S26. PMID: 24229632.
Article14. van Zuuren EJ, Arents BW, van der Linden MM, Vermeulen S, Fedorowicz Z, Tan J. Rosacea: new concepts in classification and treatment. Am J Clin Dermatol. 2021; 22(4):457–465. PMID: 33759078.
Article15. Dai YX, Tai YH, Chen CC, Chang YT, Chen TJ, Chen MH. Use of proton pump inhibitors and risk of rosacea: a nationwide population-based study. J Dermatol. 2020; 47(10):1126–1130. PMID: 32613686.16. Jackson MA, Goodrich JK, Maxan ME, Freedberg DE, Abrams JA, Poole AC, et al. Proton pump inhibitors alter the composition of the gut microbiota. Gut. 2016; 65(5):749–756. PMID: 26719299.
Article17. Imhann F, Bonder MJ, Vich Vila A, Fu J, Mujagic Z, Vork L, et al. Proton pump inhibitors affect the gut microbiome. Gut. 2016; 65(5):740–748. PMID: 26657899.
Article18. Le ST, Toussi A, Maverakis N, Marusina AI, Barton VR, Merleev AA, et al. The cutaneous and intestinal microbiome in psoriatic disease. Clin Immunol. 2020; 218:108537. PMID: 32679247.
Article19. Sikora M, Stec A, Chrabaszcz M, Knot A, Waskiel-Burnat A, Rakowska A, et al. Gut microbiome in psoriasis: an updated review. Pathogens. 2020; 9(6):463. PMID: 32545459.
Article20. Szántó M, Dózsa A, Antal D, Szabó K, Kemény L, Bai P. Targeting the gut-skin axis-probiotics as new tools for skin disorder management? Exp Dermatol. 2019; 28(11):1210–1218. PMID: 31386766.
Article21. O’Neill CA, Monteleone G, McLaughlin JT, Paus R. The gut-skin axis in health and disease: a paradigm with therapeutic implications. BioEssays. 2016; 38(11):1167–1176. PMID: 27554239.
Article22. Parodi A, Paolino S, Greco A, Drago F, Mansi C, Rebora A, et al. Small intestinal bacterial overgrowth in rosacea: clinical effectiveness of its eradication. Clin Gastroenterol Hepatol. 2008; 6(7):759–764. PMID: 18456568.
Article23. Chapat L, Chemin K, Dubois B, Bourdet-Sicard R, Kaiserlian D. Lactobacillus casei reduces CD8+ T cell-mediated skin inflammation. Eur J Immunol. 2004; 34(9):2520–2528. PMID: 15307184.
Article24. Guéniche A, Benyacoub J, Buetler TM, Smola H, Blum S. Supplementation with oral probiotic bacteria maintains cutaneous immune homeostasis after UV exposure. Eur J Dermatol. 2006; 16(5):511–517. PMID: 17101471.25. Fitz-Gibbon S, Tomida S, Chiu BH, Nguyen L, Du C, Liu M, et al. Propionibacterium acnes strain populations in the human skin microbiome associated with acne. J Invest Dermatol. 2013; 133(9):2152–2160. PMID: 23337890.
Article26. Gao Z, Tseng CH, Strober BE, Pei Z, Blaser MJ. Substantial alterations of the cutaneous bacterial biota in psoriatic lesions. PLoS One. 2008; 3(7):e2719. PMID: 18648509.
Article27. Kong HH, Oh J, Deming C, Conlan S, Grice EA, Beatson MA, et al. Temporal shifts in the skin microbiome associated with disease flares and treatment in children with atopic dermatitis. Genome Res. 2012; 22(5):850–859. PMID: 22310478.
Article28. Song H, Yoo Y, Hwang J, Na YC, Kim HS. Faecalibacterium prausnitzii subspecies-level dysbiosis in the human gut microbiome underlying atopic dermatitis. J Allergy Clin Immunol. 2016; 137(3):852–860. PMID: 26431583.
Article29. Arck P, Handjiski B, Hagen E, Pincus M, Bruenahl C, Bienenstock J, et al. Is there a ‘gut-brain-skin axis’? Exp Dermatol. 2010; 19(5):401–405. PMID: 20113345.
Article30. Nam JH, Yun Y, Kim HS, Kim HN, Jung HJ, Chang Y, et al. Rosacea and its association with enteral microbiota in Korean females. Exp Dermatol. 2018; 27(1):37–42. PMID: 28636759.
Article31. Chen YJ, Lee WH, Ho HJ, Tseng CH, Wu CY. An altered fecal microbial profiling in rosacea patients compared to matched controls. J Formos Med Assoc. 2021; 120(1 Pt 1):256–264. PMID: 32446756.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Nationwide Population-Based Study on the Association between Rosacea and Psychiatric Disorders: New Findings of Behavioral Disorders
- Risk of Pancreatic Cancer After Acute Pancreatitis: A Retrospective Analysis of the Korean National Sample Cohort
- Status of Diabetic Neuropathy in Korea: A National Health Insurance Service-National Sample Cohort Analysis (2006 to 2015)
- Two Cases of Rosacea Fulminans during Pregnancy
- Uric Acid and Risk of Cardiovascular Disease and Mortality: A Longitudinal Cohort Study