J Rhinol.
2023 Nov;30(3):129-134. 10.18787/jr.2023.00040.
Trends in Palate Surgery for Obstructive Sleep Apnea in Korea Over the Past 12 Years
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Konkuk University School of Medicine, Seoul, Republic of Korea
- 2Department of Otorhinolaryngology-Head and Neck Surgery, Soonchunhyang University College of Medicine, Bucheon Hospital, Bucheon, Republic of Korea
- KMID: 2548188
- DOI: http://doi.org/10.18787/jr.2023.00040
Abstract
- Background and Objectives
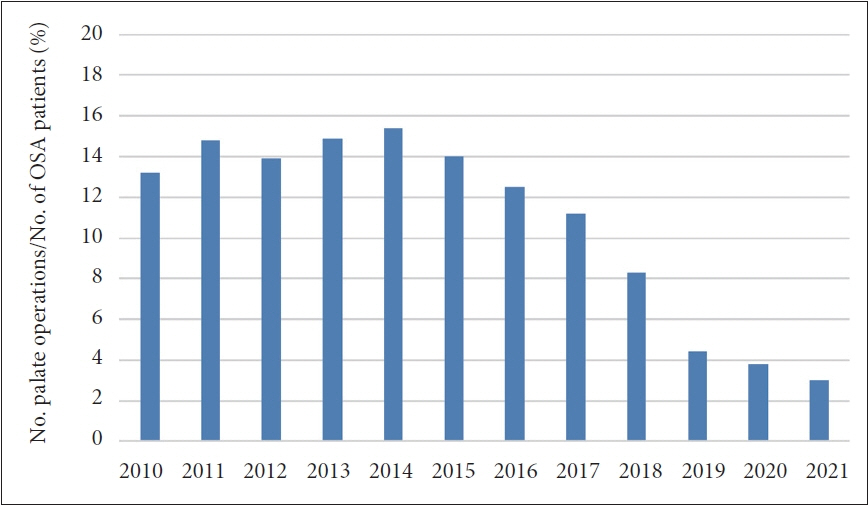
In the past, palate surgery, such as uvulopalatopharyngoplasty (UPPP), was widely performed to treat obstructive sleep apnea (OSA). However, since the introduction of reimbursement for positive airway pressure (PAP) therapy in 2018, it is believed that the frequency of these operations has significantly declined. Despite this, there are currently no definitive data to support this assertion.
Methods
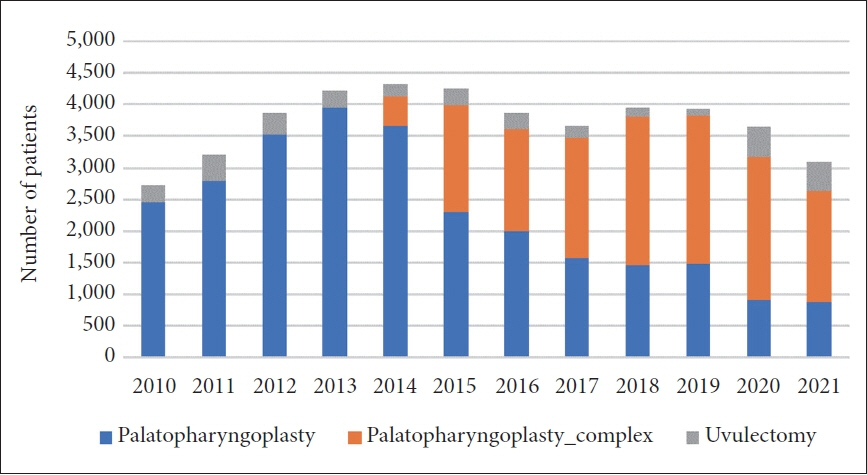
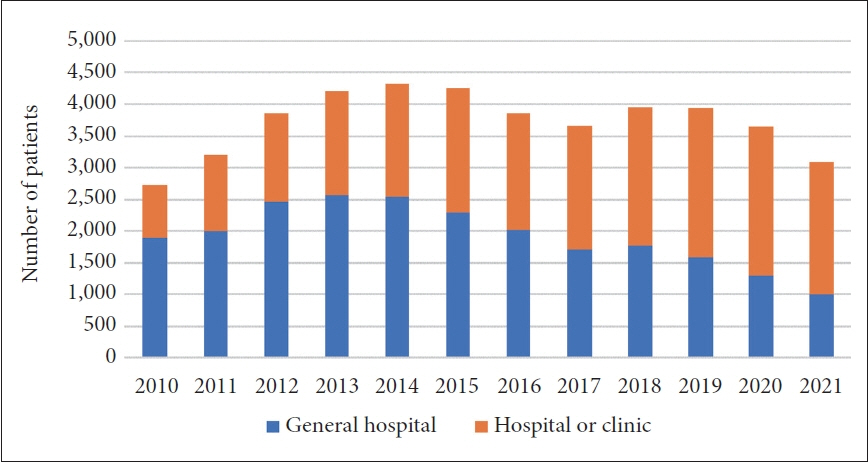
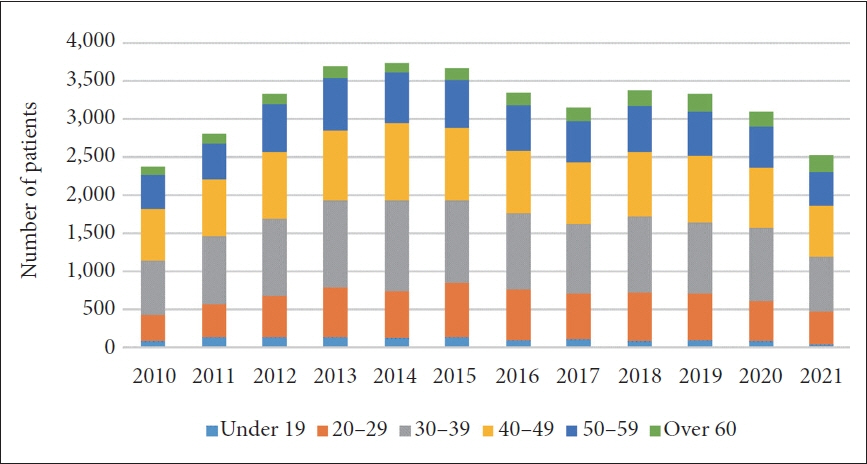
We examined the number of palate operations conducted by utilizing medical statistical data from the Health Insurance Review and Assessment Service (HIRA) Bigdata Open portal. Within this system, we queried UPPP (Q2196), UPPP_complex (Q2195), and uvulectomy (Q2197), and collected data spanning from 2010 to 2021. The data were then analyzed according to hospital type, sex, and age groups.
Results
In total, 2,728 palate operations were performed in 2010; this number peaked at 4,330 cases in 2014, and then steadily decreased to 3,096 cases in 2021. Of the operations in 2010, 1,892 were conducted in general hospitals, while 836 took place in primary hospitals and clinics. However, by 2021, the number of operations performed in general hospitals had decreased to 1,002, while those performed in primary hospitals and clinics had increased to 2,093. The most common age group for these operations was 30–39 for men and 40–49 for women. Since 2019, the proportion of palate operations relative to the number of OSA patients has decreased.
Conclusion
The frequency of palate surgery in Korea started to decrease after 2014. Despite this, there was an increase in the number of these operations performed in hospitals and clinics, with middle-aged patients being the primary recipients. The ratio of palate operations to OSA patients has shown a notable decrease after the introduction of reimbursement of polysomnography and PAP therapy.
Figure
Reference
-
References
1. Guilleminault C, Tilkian A, Dement WC. The sleep apnea syndromes. Annu Rev Med. 1976; 27:465–84.2. Kim J, In K, Kim J, You S, Kang K, Shim J, et al. Prevalence of sleep-disordered breathing in middle-aged Korean men and women. Am J Respir Crit Care Med. 2004; 170(10):1108–13.
Article3. Veasey SC, Rosen IM. Obstructive sleep apnea in adults. N Engl J Med. 2019; 380(15):1442–9.
Article4. Nieto FJ, Young TB, Lind BK, Shahar E, Samet JM, Redline S, et al. Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. JAMA. 2000; 283(14):1829–36.
Article5. Aronson D, Nakhleh M, Zeidan-Shwiri T, Mutlak M, Lavie P, Lavie L. Clinical implications of sleep disordered breathing in acute myocardial infarction. PLoS One. 2014; 9(2):e88878.
Article6. Redline S, Yenokyan G, Gottlieb DJ, Shahar E, O’Connor GT, Resnick HE, et al. Obstructive sleep apnea-hypopnea and incident stroke: the sleep heart health study. Am J Respir Crit Care Med. 2010; 182(2):269–77.
Article7. Pocobelli G, Akosile MA, Hansen RN, Eavey J, Wellman RD, Johnson RL, et al. Obstructive sleep apnea and risk of motor vehicle accident. Sleep Med. 2021; 85:196–203.
Article8. Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG. Treatment of adult obstructive sleep apnea with positive airway pressure: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2019; 15(2):335–43.
Article9. Ramar K, Dort LC, Katz SG, Lettieri CJ, Harrod CG, Thomas SM, et al. Clinical practice guideline for the treatment of obstructive sleep apnea and snoring with oral appliance therapy: an update for 2015. J Clin Sleep Med. 2015; 11(7):773–827.
Article10. Lee MK, Lee JY, Choi JH. Surgical outcomes for obstructive sleep apnea in Korea. Sleep Med Res. 2022; 13(2):63–7.
Article11. Kim B, Choi JH. Weight loss for obstructive sleep apnea: pharmacological and surgical management. J Rhinol. 2023; 30(1):1–5.
Article12. Lee E, Choi JH, Lee B, Jung JH, Seon SW, Lee S, et al. Effect of positional therapy on patients with obstructive sleep apnea: meta-analysis. J Rhinol. 2017; 24(2):94–103.
Article13. Choi JH. Treatments for adult obstructive sleep apnea. Sleep Med Res. 2021; 12(1):9–14.
Article14. Caples SM, Rowley JA, Prinsell JR, Pallanch JF, Elamin MB, Katz SG, et al. Surgical modifications of the upper airway for obstructive sleep apnea in adults: a systematic review and meta-analysis. Sleep. 2010; 33(10):1396–407.
Article15. Choi JH. Positive airway pressure prescription and management for patients with obstructive sleep apnea. J Rhinol. 2020; 27(2):73–82.
Article16. Tang JA, Salapatas AM, Bonzelaar LB, Friedman M. Long-term incidence of velopharyngeal insufficiency and other sequelae following uvulopalatopharyngoplasty. Otolaryngol Head Neck Surg. 2017; 156(4):606–10.
Article17. Cho JH. Cost-effectiveness analysis of uvulopalatopharyngoplasty versus positive airway pressure in patient with obstructive sleep apnea in South Korea. J Rhinol. 2023; 30(1):15–22.
Article18. Kim JH, Kwon MS, Song HM, Lee BJ, Jang YJ, Chung YS. Compliance with positive airway pressure treatment for obstructive sleep apnea. Clin Exp Otorhinolaryngol. 2009; 2(2):90–6.
Article19. Perger E, Mattaliano P, Lombardi C. Menopause and sleep apnea. Maturitas. 2019; 124:35–8.
Article20. Koo SK, Song CY, Kim HK, Han CW, Lee SW, Chon KM. A comparative study between male and female patients with obstructive sleep apnea. Korean J Otorhinolaryngol-Head Neck Surg. 2004; 47(12):1247–50.21. Choi JH, Lee JY, Cha J, Kim K, Hong SN, Lee SH. Predictive models of objective oropharyngeal OSA surgery outcomes: success rate and AHI reduction ratio. PLoS One. 2017; 12(9):e0185201.
Article22. Kwak KH, Lee YJ, Lee JY, Cho JH, Choi JH. The effect of pharyngeal surgery on positive airway pressure therapy in obstructive sleep apnea: a meta-analysis. J Clin Med. 2022; 11(21):6443.
Article