J Yeungnam Med Sci.
2023 Oct;40(4):448-453. 10.12701/jyms.2023.00122.
Endovascular treatment of Takayasu arteritis in a middle-aged woman with syncope and limb claudication: a case report
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea
- 2Division of Rheumatology, Department of Internal Medicine, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea
- KMID: 2547372
- DOI: http://doi.org/10.12701/jyms.2023.00122
Abstract
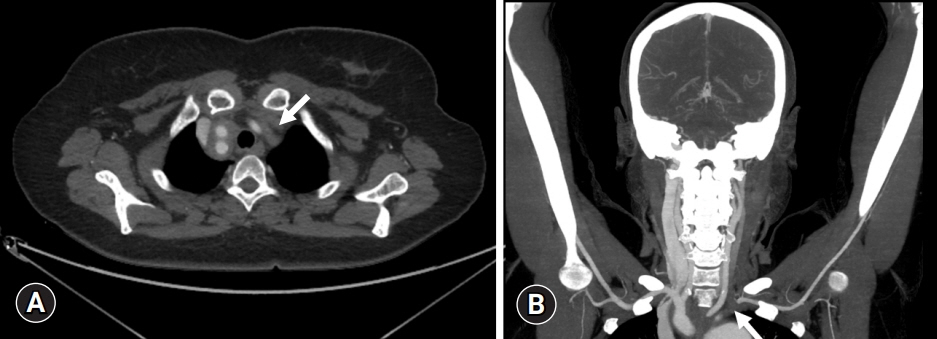
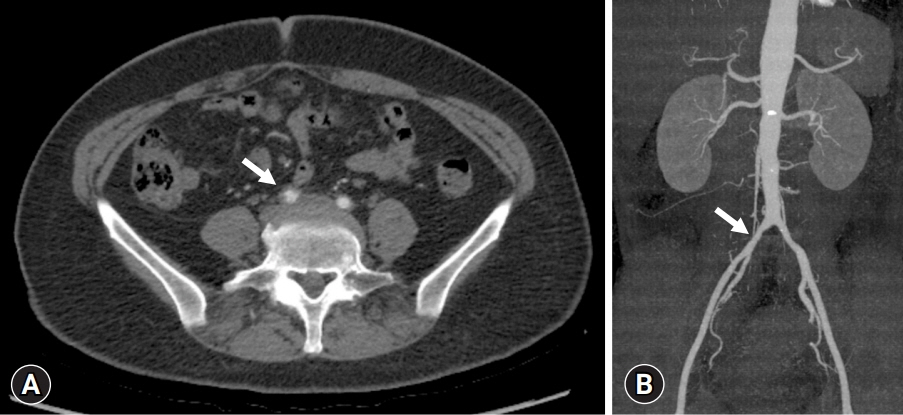
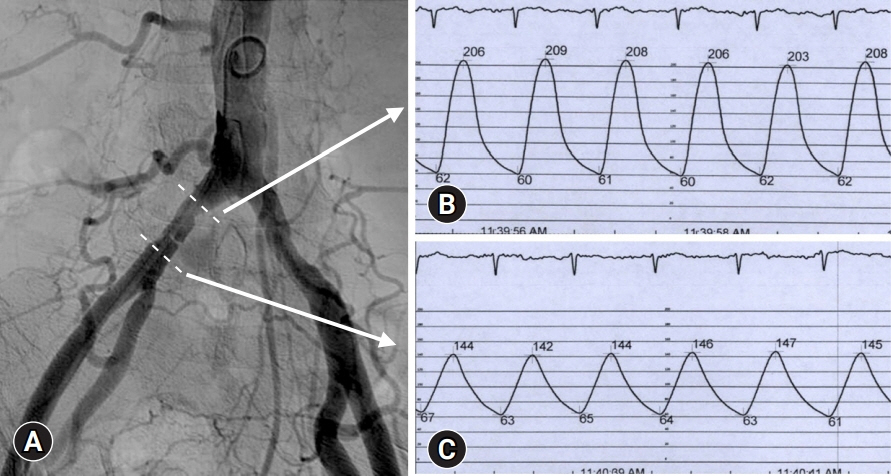
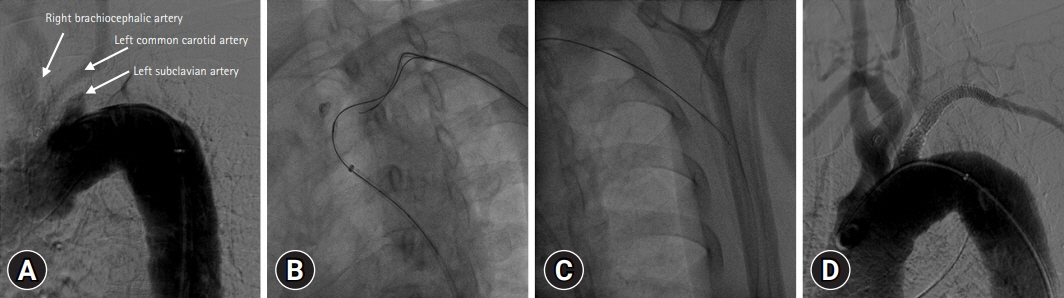
- Takayasu arteritis (TA) is a disease that causes inflammation and stenosis of medium to large blood vessels. We report a case of a 50-year-old female patient with newly developed hypertension, syncope, and claudication of the extremities. Total occlusion of the left subclavian artery at the origin was found and significant stenosis of the right common iliac artery was revealed by hemodynamic analysis. She was successfully treated with percutaneous angioplasty for multiple peripheral arterial diseases and was finally diagnosed with TA. In consultation with a rheumatologist, medical treatment for TA was initiated, the patient’s hypertension disappeared, and her claudication symptoms improved.
Figure
Reference
-
References
1. Ishikawa K. Diagnostic approach and proposed criteria for the clinical diagnosis of Takayasu’s arteriopathy. J Am Coll Cardiol. 1988; 12:964–72.
Article2. Hata A, Noda M, Moriwaki R, Numano F. Angiographic findings of Takayasu arteritis: new classification. Int J Cardiol. 1996; 54(Suppl):S155–63.
Article3. Osiro S, Zurada A, Gielecki J, Shoja MM, Tubbs RS, Loukas M. A review of subclavian steal syndrome with clinical correlation. Med Sci Monit. 2012; 18:RA57–63.
Article4. Gu YQ, Wang ZG. Surgical treatment of cerebral ischaemia caused by cervical arterial lesions due to Takayasu’s arteritis: preliminary results of 49 cases. ANZ J Surg. 2001; 71:89–92.
Article5. de Boer SW, Heinen S, van den Heuvel D, van de Vosse FN, de Vries J; study contributors. How to define the hemodynamic significance of an equivocal iliofemoral artery stenosis: review of literature and outcomes of an international questionnaire. Vascular. 2017; 25:598–608.
Article6. Zhu FP, Luo S, Wang ZJ, Jin ZY, Zhang LJ, Lu GM. Takayasu arteritis: imaging spectrum at multidetector CT angiography. Br J Radiol. 2012; 85:e1282–92.
Article7. Arend WP, Michel BA, Bloch DA, Hunder GG, Calabrese LH, Edworthy SM, et al. The American College of Rheumatology 1990 criteria for the classification of Takayasu arteritis. Arthritis Rheum. 1990; 33:1129–34.
Article8. Hellmich B, Agueda A, Monti S, Buttgereit F, de Boysson H, Brouwer E, et al. 2018 Update of the EULAR recommendations for the management of large vessel vasculitis. Ann Rheum Dis. 2020; 79:19–30.
Article9. Sharma BK, Jain S, Suri S, Numano F. Diagnostic criteria for Takayasu arteritis. Int J Cardiol. 1996; 54(Suppl):S141–7.
Article10. Yoneda S, Nukada T, Tada K, Imaizumi M, Takano T. Subclavian steal in Takayasu’s arteritis: a hemodynamic study by means of ultrasonic Doppler flowmetry. Stroke. 1977; 8:264–8.
Article11. Águeda AF, Monti S, Luqmani RA, Buttgereit F, Cid M, Dasgupta B, et al. Management of Takayasu arteritis: a systematic literature review informing the 2018 update of the EULAR recommendation for the management of large vessel vasculitis. RMD Open. 2019; 5:e001020.
Article12. Patel SN, White CJ, Collins TJ, Daniel GA, Jenkins JS, Reilly JP, et al. Catheter-based treatment of the subclavian and innominate arteries. Catheter Cardiovasc Interv. 2008; 71:963–8.
Article13. Ogino H, Matsuda H, Minatoya K, Sasaki H, Tanaka H, Matsumura Y, et al. Overview of late outcome of medical and surgical treatment for Takayasu arteritis. Circulation. 2008; 118:2738–47.
Article14. Choi YK, Jung YO, Kim HM, Kang MK. A case of a patient with Takayasu arteritis treated with left subclavian artery stent implantation. J Cardiol Cases. 2015; 12:123–5.
Article15. Satti SR, Golwala SN, Vance AZ, Tuerff SN. Subclavian steal: Endovascular treatment of total occlusions of the subclavian artery using a retrograde transradial subintimal approach. Interv Neuroradiol. 2016; 22:340–8.
Article16. Hadjipetrou P, Cox S, Piemonte T, Eisenhauer A. Percutaneous revascularization of atherosclerotic obstruction of aortic arch vessels. J Am Coll Cardiol. 1999; 33:1238–45.
Article17. Kandarpa K, Becker GJ, Hunink MG, McNamara TO, Rundback JH, Trost DW, et al. Transcatheter interventions for the treatment of peripheral atherosclerotic lesions: part I. J Vasc Interv Radiol. 2001; 12:683–95.
Article18. Brountzos EN, Malagari K, Kelekis DA. Endovascular treatment of occlusive lesions of the subclavian and innominate arteries. Cardiovasc Intervent Radiol. 2006; 29:503–10.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Takayasu Arteritis Associated with Sarcoidosis: A Case Report
- Middle aortic syndrome diagnosed at 51 years of age
- A Case Report of Takayaeu's Arteritis Associated with, a Retinopathy
- Extra-anatomic Aortic Bypass for the Management of Mid-Aortic Syndrome Caused by Takayasu arteritis
- A Case of Paroxysmal Atrioventricular Block Complicating Takayasu's Arteritis