Nutr Res Pract.
2023 Oct;17(5):883-898. 10.4162/nrp.2023.17.5.883.
Probiotic supplementation has sexdependent effects on immune responses in association with the gut microbiota in community-dwelling older adults: a randomized, double-blind, placebocontrolled, multicenter trial
- Affiliations
-
- 1Department of Food and Nutrition, College of Natural Information Sciences, Dongduk Women's University, Seoul 02748, Korea
- 2Department of Biomedical Sciences, Seoul National University College of Medicine, Seoul 03080, Korea
- 3Department of Food and Nutrition, College of Human Ecology, Seoul National University, Seoul 08826, Korea
- KMID: 2546946
- DOI: http://doi.org/10.4162/nrp.2023.17.5.883
Abstract
- BACKGROUND/OBJECTIVES
Probiotics have been suggested as potent modulators of agerelated disorders in immunological functions, yet little is known about sex-dependent effects of probiotic supplements. Therefore, we aimed to investigate sex-dependent effects of probiotics on profiles of the gut microbiota and peripheral immune cells in healthy older adults.
SUBJECTS/METHODS
In a randomized, double-blind, placebo-controlled, multicenter trial, healthy elderly individuals ≥ 65 yrs old were administered probiotic capsules (or placebo) for 12 wk. Gut microbiota was analyzed using 16S rRNA gene sequencing and bioinformatic analyses. Peripheral immune cells were profiled using flow cytometry for lymphocytes (natural killer, B, CD4 + T, and CD8 + T cells), dendritic cells, monocytes, and their subpopulations.
RESULTS
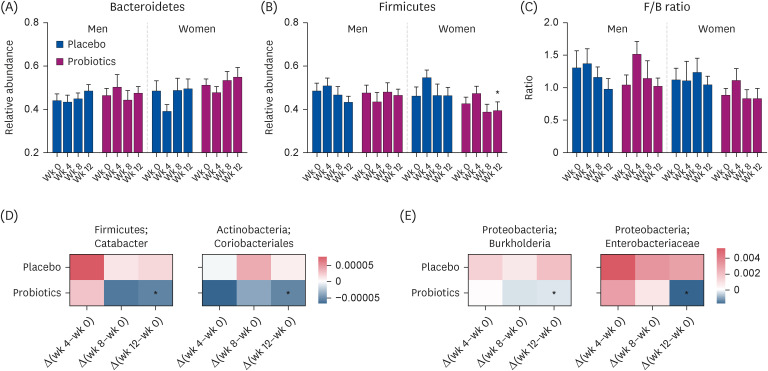
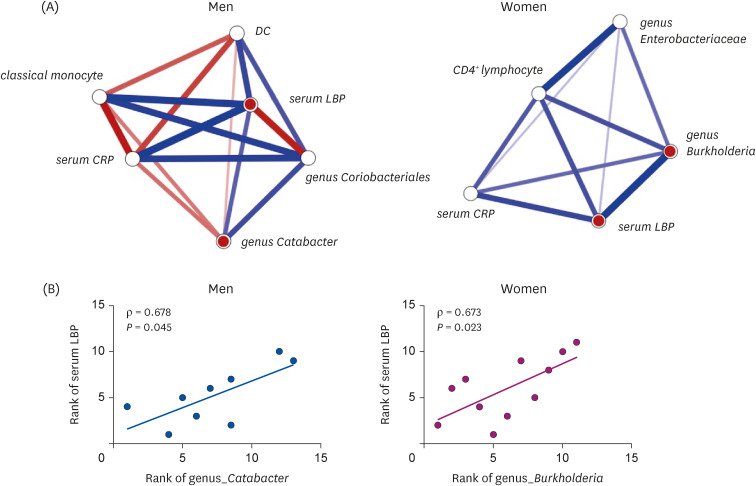
Compared with placebo, phylum Firmicutes was significantly reduced in the probiotic group in women, but not in men. At the genus level, sex-specific responses included reductions in the relative abundances of pro-inflammatory gut microbes, including Catabacter and unclassified_Coriobacteriales, and Burkholderia and unclassified Enterobacteriaceae, in men and women, respectively. Peripheral immune cell profiling analysis revealed that in men, probiotics significantly reduced the proportions of dendritic cells and CD14 + CD16 - monocytes; however, these effects were not observed in women. In contrast, the proportion of total CD4 + T cells was significantly reduced in women in the probiotic group. Additionally, serum lipopolysaccharide-binding protein levels showed a decreasing tendency that were positively associated with changes in gut bacteria, including Catabacter (ρ = 0.678, P < 0.05) and Burkholderia (ρ = 0.673, P < 0.05) in men and women, respectively.
CONCLUSIONS
These results suggest that probiotic supplementation may reduce the incidence of inflammation-related diseases by regulating the profiles of the gut microbiota and peripheral immune cells in healthy elders in a sex-specific manner.
Keyword
Figure
Reference
-
1. Nikolich-Žugich J. The twilight of immunity: emerging concepts in aging of the immune system. Nat Immunol. 2018; 19:10–19. PMID: 29242543.2. Franceschi C, Garagnani P, Parini P, Giuliani C, Santoro A. Inflammaging: a new immune-metabolic viewpoint for age-related diseases. Nat Rev Endocrinol. 2018; 14:576–590. PMID: 30046148.3. Deleidi M, Jäggle M, Rubino G. Immune aging, dysmetabolism, and inflammation in neurological diseases. Front Neurosci. 2015; 9:172. PMID: 26089771.4. Marchesi JR, Adams DH, Fava F, Hermes GD, Hirschfield GM, Hold G, Quraishi MN, Kinross J, Smidt H, Tuohy KM, et al. The gut microbiota and host health: a new clinical frontier. Gut. 2016; 65:330–339. PMID: 26338727.5. Rooks MG, Garrett WS. Gut microbiota, metabolites and host immunity. Nat Rev Immunol. 2016; 16:341–352. PMID: 27231050.6. Sharma R, Padwad Y. Probiotic bacteria as modulators of cellular senescence: emerging concepts and opportunities. Gut Microbes. 2020; 11:335–349. PMID: 31818183.7. Vaiserman AM, Koliada AK, Marotta F. Gut microbiota: a player in aging and a target for anti-aging intervention. Ageing Res Rev. 2017; 35:36–45. PMID: 28109835.8. Gill HS, Rutherfurd KJ, Cross ML, Gopal PK. Enhancement of immunity in the elderly by dietary supplementation with the probiotic Bifidobacterium lactis HN019. Am J Clin Nutr. 2001; 74:833–839. PMID: 11722966.9. Gill HS, Rutherfurd KJ, Cross ML. Dietary probiotic supplementation enhances natural killer cell activity in the elderly: an investigation of age-related immunological changes. J Clin Immunol. 2001; 21:264–271. PMID: 11506196.10. Leblanc V, Hudon AM, Royer MM, Corneau L, Dodin S, Bégin C, Lemieux S. Differences between men and women in dietary intakes and metabolic profile in response to a 12-week nutritional intervention promoting the Mediterranean diet. J Nutr Sci. 2015; 4:e13. PMID: 26090094.11. Bédard A, Riverin M, Dodin S, Corneau L, Lemieux S. Sex differences in the impact of the Mediterranean diet on cardiovascular risk profile. Br J Nutr. 2012; 108:1428–1434. PMID: 22221517.12. Yaqoob P. Ageing alters the impact of nutrition on immune function. Proc Nutr Soc. 2017; 76:347–351. PMID: 27821203.13. Kim CS, Cha L, Sim M, Jung S, Chun WY, Baik HW, Shin DM. Probiotic supplementation improves cognitive function and mood with changes in gut microbiota in community-dwelling older adults: a randomized, double-blind, placebo-controlled, multicenter trial. J Gerontol A Biol Sci Med Sci. 2021; 76:32–40. PMID: 32300799.14. Caporaso JG, Kuczynski J, Stombaugh J, Bittinger K, Bushman FD, Costello EK, Fierer N, Peña AG, Goodrich JK, Gordon JI, et al. QIIME allows analysis of high-throughput community sequencing data. Nat Methods. 2010; 7:335–336. PMID: 20383131.15. Maijó M, Clements SJ, Ivory K, Nicoletti C, Carding SR. Nutrition, diet and immunosenescence. Mech Ageing Dev. 2014; 136-137:116–128. PMID: 24373813.16. Pae M, Meydani SN, Wu D. The role of nutrition in enhancing immunity in aging. Aging Dis. 2012; 3:91–129. PMID: 22500273.17. Fortes C, Forastiere F, Agabiti N, Fano V, Pacifici R, Virgili F, Piras G, Guidi L, Bartoloni C, Tricerri A, et al. The effect of zinc and vitamin A supplementation on immune response in an older population. J Am Geriatr Soc. 1998; 46:19–26. PMID: 9434661.18. Arunachalam K, Gill HS, Chandra RK. Enhancement of natural immune function by dietary consumption of Bifidobacterium lactis (HN019). Eur J Clin Nutr. 2000; 54:263–267. PMID: 10713750.19. Dong H, Rowland I, Thomas LV, Yaqoob P. Immunomodulatory effects of a probiotic drink containing Lactobacillus casei Shirota in healthy older volunteers. Eur J Nutr. 2013; 52:1853–1863. PMID: 23307112.20. Cancro MP, Hao Y, Scholz JL, Riley RL, Frasca D, Dunn-Walters DK, Blomberg BB. B cells and aging: molecules and mechanisms. Trends Immunol. 2009; 30:313–318. PMID: 19540810.21. Panda A, Arjona A, Sapey E, Bai F, Fikrig E, Montgomery RR, Lord JM, Shaw AC. Human innate immunosenescence: causes and consequences for immunity in old age. Trends Immunol. 2009; 30:325–333. PMID: 19541535.22. Franceschi C, Garagnani P, Vitale G, Capri M, Salvioli S. Inflammaging and ‘Garb-aging’. Trends Endocrinol Metab. 2017; 28:199–212. PMID: 27789101.23. Aziz M, Holodick NE, Rothstein TL, Wang P. The role of B-1 cells in inflammation. Immunol Res. 2015; 63:153–166. PMID: 26427372.24. Pence BD. Fanning the flames of inflammaging: impact of monocyte metabolic reprogramming. Immunometabolism. 2020; 2:e200025. PMID: 32742735.25. Hearps AC, Martin GE, Angelovich TA, Cheng WJ, Maisa A, Landay AL, Jaworowski A, Crowe SM. Aging is associated with chronic innate immune activation and dysregulation of monocyte phenotype and function. Aging Cell. 2012; 11:867–875. PMID: 22708967.26. Brestoff JR, Artis D. Commensal bacteria at the interface of host metabolism and the immune system. Nat Immunol. 2013; 14:676–684. PMID: 23778795.27. Schroeder BO, Birchenough GM, Ståhlman M, Arike L, Johansson ME, Hansson GC, Bäckhed F. Bifidobacteria or fiber protects against diet-induced microbiota-mediated colonic mucus deterioration. Cell Host Microbe. 2018; 23:27–40.e7. PMID: 29276171.28. Bergmann KR, Liu SX, Tian R, Kushnir A, Turner JR, Li HL, Chou PM, Weber CR, De Plaen IG. Bifidobacteria stabilize claudins at tight junctions and prevent intestinal barrier dysfunction in mouse necrotizing enterocolitis. Am J Pathol. 2013; 182:1595–1606. PMID: 23470164.29. Quince C, Ijaz UZ, Loman N, Eren AM, Saulnier D, Russell J, Haig SJ, Calus ST, Quick J, Barclay A, et al. Extensive modulation of the fecal metagenome in children with Crohn’s disease during exclusive enteral nutrition. Am J Gastroenterol. 2015; 110:1718–1729. PMID: 26526081.30. Sampson T. The impact of indigenous microbes on Parkinson’s disease. Neurobiol Dis. 2020; 135:104426. PMID: 30885792.31. Zákostelská Z, Málková J, Klimešová K, Rossmann P, Hornová M, Novosádová I, Stehlíková Z, Kostovčík M, Hudcovic T, Štepánková R, et al. Intestinal microbiota promotes psoriasis-like skin inflammation by enhancing Th17 response. PLoS One. 2016; 11:e0159539. PMID: 27434104.32. Linton PJ, Dorshkind K. Age-related changes in lymphocyte development and function. Nat Immunol. 2004; 5:133–139. PMID: 14749784.33. Goronzy JJ, Weyand CM. Immune aging and autoimmunity. Cell Mol Life Sci. 2012; 69:1615–1623. PMID: 22466672.34. Weksler ME, Hütteroth TH. Impaired lymphocyte function in aged humans. J Clin Invest. 1974; 53:99–104. PMID: 4855547.35. Mittelbrunn M, Kroemer G. Hallmarks of T cell aging. Nat Immunol. 2021; 22:687–698. PMID: 33986548.36. Vaiserman A, Romanenko M, Piven L, Moseiko V, Lushchak O, Kryzhanovska N, Guryanov V, Koliada A. Differences in the gut Firmicutes to Bacteroidetes ratio across age groups in healthy Ukrainian population. BMC Microbiol. 2020; 20:221. PMID: 32698765.37. Magrone T, Jirillo E. The interaction between gut microbiota and age-related changes in immune function and inflammation. Immun Ageing. 2013; 10:31. PMID: 23915308.38. Fink J, Steer JH, Joyce DA, McWilliam AS, Stewart GA. Pro-inflammatory effects of Burkholderia cepacia on cystic fibrosis respiratory epithelium. FEMS Immunol Med Microbiol. 2003; 38:273–282. PMID: 14522463.39. Shrivastava SR, Shrivastava PS, Ramasamy J. World health organization releases global priority list of antibiotic-resistant bacteria to guide research, discovery, and development of new antibiotics. J Med Soc. 2018; 32:76.40. Hegazy AN, West NR, Stubbington MJ, Wendt E, Suijker KI, Datsi A, This S, Danne C, Campion S, Duncan SH, et al. Circulating and tissue-resident CD4+ T cells with reactivity to intestinal microbiota are abundant in healthy individuals and function is altered during inflammation. Gastroenterology. 2017; 153:1320–1337.e16. PMID: 28782508.41. Cassotta A, Goldstein JD, Durini G, Jarrossay D, Baggi Menozzi F, Venditti M, Russo A, Falcone M, Lanzavecchia A, Gagliardi MC, et al. Broadly reactive human CD4+ T cells against Enterobacteriaceae are found in the naïve repertoire and are clonally expanded in the memory repertoire. Eur J Immunol. 2021; 51:648–661. PMID: 33226131.42. Djuric Z. Obesity-associated cancer risk: the role of intestinal microbiota in the etiology of the host proinflammatory state. Transl Res. 2017; 179:155–167. PMID: 27522986.43. Kavanagh K, Hsu FC, Davis AT, Kritchevsky SB, Rejeski WJ, Kim S. Biomarkers of leaky gut are related to inflammation and reduced physical function in older adults with cardiometabolic disease and mobility limitations. Geroscience. 2019; 41:923–933. PMID: 31654268.44. Roberts LM, Buford TW. Lipopolysaccharide binding protein is associated with CVD risk in older adults. Aging Clin Exp Res. 2021; 33:1651–1658. PMID: 32895891.45. Stehle JR Jr, Leng X, Kitzman DW, Nicklas BJ, Kritchevsky SB, High KP. Lipopolysaccharide-binding protein, a surrogate marker of microbial translocation, is associated with physical function in healthy older adults. J Gerontol A Biol Sci Med Sci. 2012; 67:1212–1218. PMID: 22960476.46. Everard A, Lazarevic V, Gaïa N, Johansson M, Ståhlman M, Backhed F, Delzenne NM, Schrenzel J, François P, Cani PD. Microbiome of prebiotic-treated mice reveals novel targets involved in host response during obesity. ISME J. 2014; 8:2116–2130. PMID: 24694712.47. González-Sarrías A, Núñez-Sánchez MA, Ávila-Gálvez MA, Monedero-Saiz T, Rodríguez-Gil FJ, Martínez-Díaz F, Selma MV, Espín JC. Consumption of pomegranate decreases plasma lipopolysaccharide-binding protein levels, a marker of metabolic endotoxemia, in patients with newly diagnosed colorectal cancer: a randomized controlled clinical trial. Food Funct. 2018; 9:2617–2622. PMID: 29770393.48. Pei R, DiMarco DM, Putt KK, Martin DA, Gu Q, Chitchumroonchokchai C, White HM, Scarlett CO, Bruno RS, Bolling BW. Low-fat yogurt consumption reduces biomarkers of chronic inflammation and inhibits markers of endotoxin exposure in healthy premenopausal women: a randomised controlled trial. Br J Nutr. 2017; 118:1043–1051. PMID: 29179781.49. Wiersinga WJ, de Vos AF, de Beer R, Wieland CW, Roelofs JJ, Woods DE, van der Poll T. Inflammation patterns induced by different Burkholderia species in mice. Cell Microbiol. 2008; 10:81–87. PMID: 17645551.50. Bolnick DI, Snowberg LK, Hirsch PE, Lauber CL, Org E, Parks B, Lusis AJ, Knight R, Caporaso JG, Svanbäck R. Individual diet has sex-dependent effects on vertebrate gut microbiota. Nat Commun. 2014; 5:4500. PMID: 25072318.51. David LA, Maurice CF, Carmody RN, Gootenberg DB, Button JE, Wolfe BE, Ling AV, Devlin AS, Varma Y, Fischbach MA, et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 2014; 505:559–563. PMID: 24336217.52. Markle JG, Frank DN, Mortin-Toth S, Robertson CE, Feazel LM, Rolle-Kampczyk U, von Bergen M, McCoy KD, Macpherson AJ, Danska JS. Sex differences in the gut microbiome drive hormone-dependent regulation of autoimmunity. Science. 2013; 339:1084–1088. PMID: 23328391.53. Moore RJ, Stanley D. Experimental design considerations in microbiota/inflammation studies. Clin Transl Immunology. 2016; 5:e92. PMID: 27525065.54. Xyda SE, Vuckovic I, Petterson XM, Dasari S, Lalia AZ, Parvizi M, Macura SI, Lanza IR. Distinct influence of omega-3 fatty acids on the plasma metabolome of healthy older adults. J Gerontol A Biol Sci Med Sci. 2020; 75:875–884. PMID: 31168623.55. Nagpal R, Neth BJ, Wang S, Craft S, Yadav H. Modified Mediterranean-ketogenic diet modulates gut microbiome and short-chain fatty acids in association with Alzheimer’s disease markers in subjects with mild cognitive impairment. EBioMedicine. 2019; 47:529–542. PMID: 31477562.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Probiotic Supplementation for Treatment of Helicobacter pylori Infection: A Double-Blind Randomized Clinical Trial
- Comments on Efficacy of a Synbiotic Containing Lactobacillus paracasei DKGF1 and Opuntia humifusa in Elderly Patients with Irritable Bowel Syndrome: A Randomized, Double-Blind, PlaceboControlled Trial
- Effects of Auricular Acupressure Therapy on Psychological Factors, Sleep Quality, and Salivary Cortisol Levels in South Korean Older Adults in the Community: A Single-blind, Randomized Controlled Trial
- Effects of a Psychobiotic Supplement on Serum Brain-derived Neurotrophic Factor Levels in Depressive Patients: A Post Hoc Analysis of a Randomized Clinical Trial
- Microbial Modulation in Inflammatory Bowel Diseases