Endocrinol Metab.
2023 Aug;38(4):436-444. 10.3803/EnM.2023.1684.
Prevalence, Treatment Status, and Comorbidities of Hyperthyroidism in Korea from 2003 to 2018: A Nationwide Population Study
- Affiliations
-
- 1Department of Internal Medicine, Chung-Ang University College of Medicine, Seoul, Korea
- 2Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea
- 3Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea
- 4Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea
- 5Department of Internal Medicine and Genomic Medicine Institute, Medical Research Center, Seoul National University College of Medicine, Seoul, Korea
- 6Department of Molecular Medicine and Biopharmaceutical Sciences, Graduate School of Convergence Science and Technology, Seoul National University, Seoul, Korea
- 7Department of Otolaryngology-Head and Neck Surgery, Chungnam National University College of Medicine, Daejeon, Korea
- 8Department of Surgery, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 9Department of Internal Medicine, Seoul Metropolitan Government Seoul National University Boramae Medical Center, Seoul, Korea
- KMID: 2545276
- DOI: http://doi.org/10.3803/EnM.2023.1684
Abstract
- Background
This study aimed to investigate the changes of incidence and treatment of choice for hyperthyroidism from 2003 to 2018 and explore the treatment-related complications and concomitant comorbidities in South Korea using data from the National Health Insurance Service.
Methods
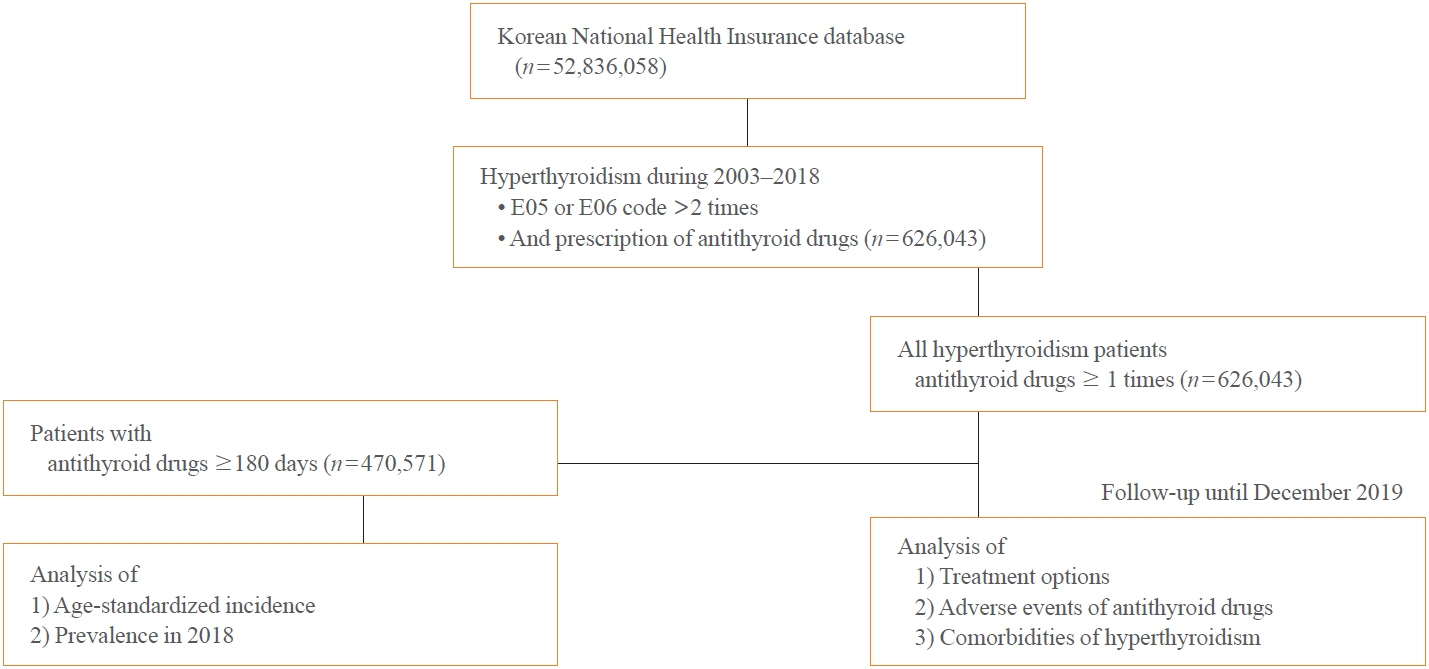
This is a retrospective observational study. Hyperthyroidism was defined as a case having two or more diagnostic codes of thyrotoxicosis, with antithyroid drug intake for more than 6 months.
Results
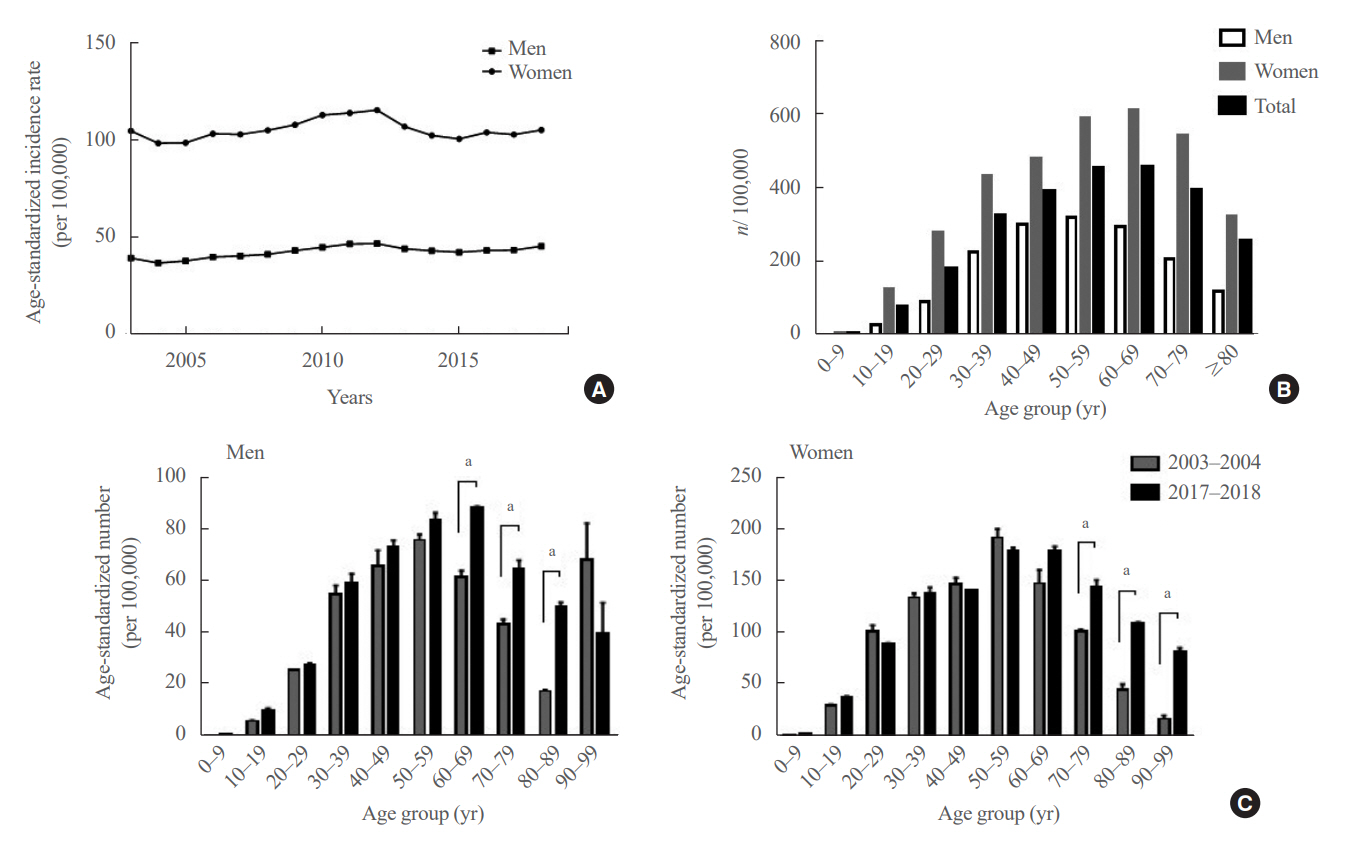
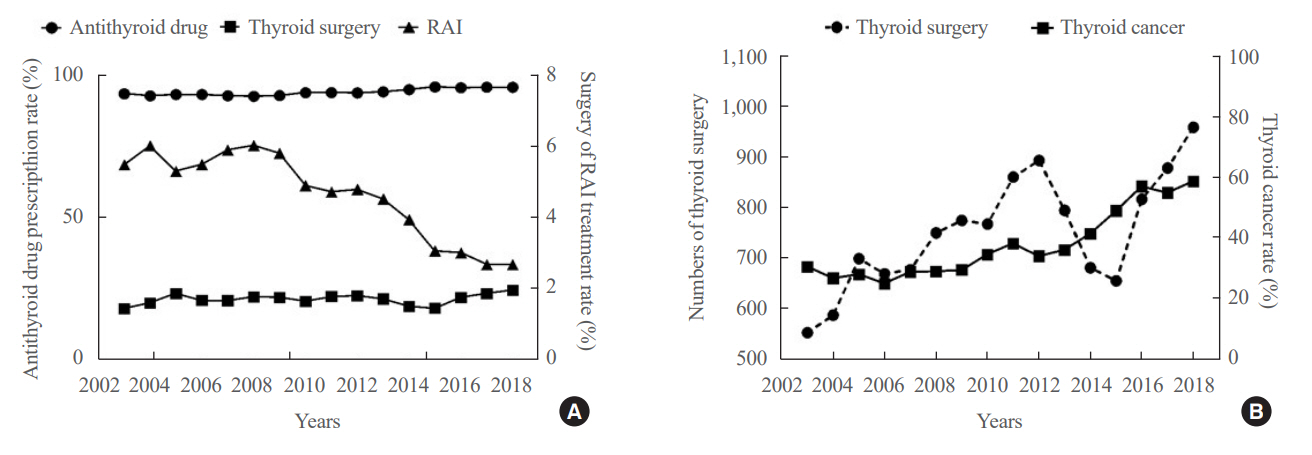
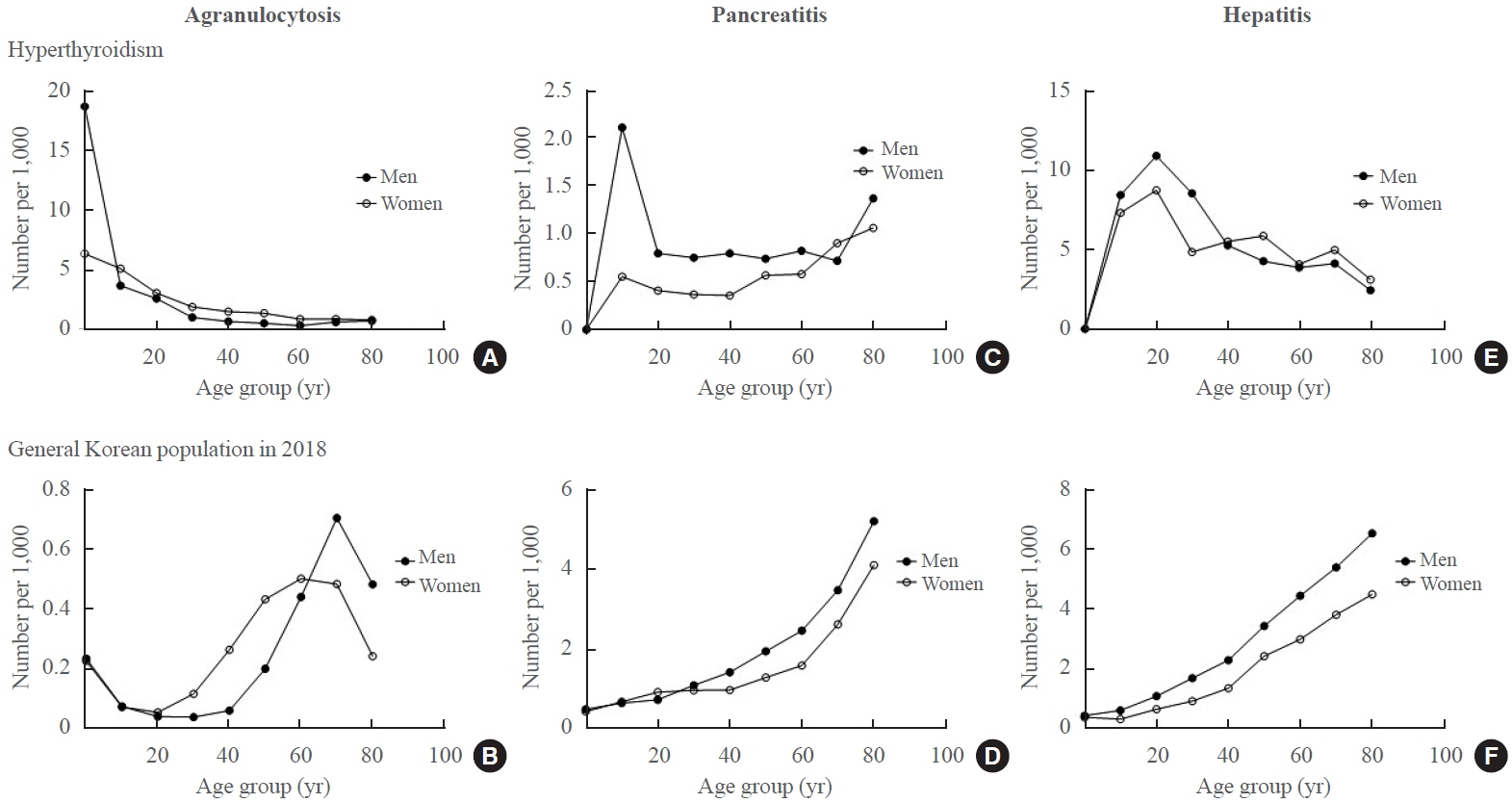
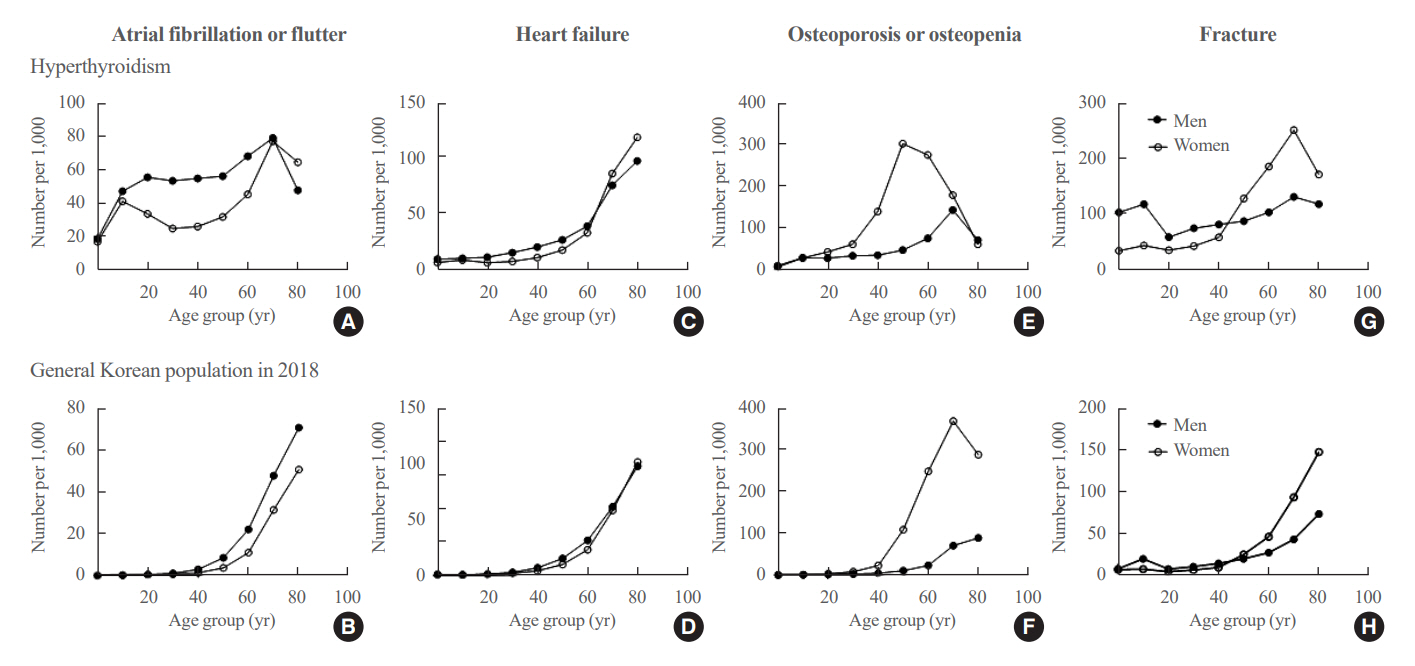
The average age-standardized incidence of hyperthyroidism from 2003 to 2018 was 42.23 and 105.13 per 100,000 men and women, respectively. In 2003 to 2004, hyperthyroidism was most often diagnosed in patients in their 50s, but in 2017 to 2018, people were most often diagnosed in their 60s. During the entire period, about 93.7% of hyperthyroidism patients were prescribed with antithyroid drugs, and meanwhile, the annual rates of ablation therapy decrease from 7.68% in 2008 to 4.56% in 2018. Antithyroid drug-related adverse events, mainly agranulocytosis and acute hepatitis, as well as complications of hyperthyroidism such as atrial fibrillation or flutter, osteoporosis, and fractures, occurred more often in younger patients.
Conclusion
In Korea, hyperthyroidism occurred about 2.5 times more in women than in men, and antithyroid drugs were most preferred as the first-line treatment. Compared to the general population, hyperthyroid patients may have a higher risk of atrial fibrillation or flutter, osteoporosis, and fractures at a younger age.
Keyword
Figure
Reference
-
1. Pearce EN. Diagnosis and management of thyrotoxicosis. BMJ. 2006; 332:1369–73.2. Ross DS, Burch HB, Cooper DS, Greenlee MC, Laurberg P, Maia AL, et al. 2016 American Thyroid Association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid. 2016; 26:1343–421.3. Seo GH, Kim SW, Chung JH. Incidence & prevalence of hyperthyroidism and preference for therapeutic modalities in Korea. J Korean Thyroid Assoc. 2013; 6:56–63.4. Franklyn JA, Boelaert K. Thyrotoxicosis. Lancet. 2012; 379:1155–66.5. Guo JY, Chang CL, Chen CC. Association between thionamides and acute pancreatitis: a case-control study. Thyroid. 2020; 30:1574–8.6. Woeber KA. Thyrotoxicosis and the heart. N Engl J Med. 1992; 327:94–8.7. Nicholls JJ, Brassill MJ, Williams GR, Bassett JH. The skeletal consequences of thyrotoxicosis. J Endocrinol. 2012; 213:209–21.8. Kwon H, Jung JH, Han KD, Park YG, Cho JH, Lee DY, et al. Prevalence and annual incidence of thyroid disease in Korea from 2006 to 2015: a nationwide population-based cohort study. Endocrinol Metab (Seoul). 2018; 33:260–7.9. Lee YH, Han K, Ko SH, Ko KS, Lee KU; Taskforce Team of Diabetes Fact Sheet of the Korean Diabetes Association. Data analytic process of a nationwide population-based study using national health information database established by National Health Insurance Service. Diabetes Metab J. 2016; 40:79–82.10. Cho SW, Kim JH, Choi HS, Ahn HY, Kim MK, Rhee EJ. Big data research in the field of endocrine diseases using the Korean National Health Information Database. Endocrinol Metab (Seoul). 2023; 38:10–24.11. Kim HI, Oh HK, Park SY, Jang HW, Shin MH, Kim SW, et al. Urinary iodine concentration and thyroid hormones: Korea National Health and Nutrition Examination Survey 2013-2015. Eur J Nutr. 2019; 58:233–40.12. Taylor PN, Albrecht D, Scholz A, Gutierrez-Buey G, Lazarus JH, Dayan CM, et al. Global epidemiology of hyperthyroidism and hypothyroidism. Nat Rev Endocrinol. 2018; 14:301–16.13. Kornelius E, Yang YS, Huang CN, Wang YH, Lo SC, Lai YR, et al. The trends of hyperthyroidism treatment in Taiwan: a nationwide population-based study. Endocr Pract. 2018; 24:573–9.14. Brito JP, Schilz S, Singh Ospina N, Rodriguez-Gutierrez R, Maraka S, Sangaralingham LR, et al. Antithyroid drugs: the most common treatment for Graves’ disease in the United States: a nationwide population-based study. Thyroid. 2016; 26:1144–5.15. Yoon JH, Jin M, Kim M, Hong AR, Kim HK, Kim BH, et al. Clinical characteristics and prognosis of coexisting thyroid cancer in patients with Graves’ disease: a retrospective multicenter study. Endocrinol Metab (Seoul). 2021; 36:1268–76.16. Varadharajan K, Choudhury N. A systematic review of the incidence of thyroid carcinoma in patients undergoing thyroidectomy for thyrotoxicosis. Clin Otolaryngol. 2020; 45:538–44.17. Li M, Dal Maso L, Vaccarella S. Global trends in thyroid cancer incidence and the impact of overdiagnosis. Lancet Diabetes Endocrinol. 2020; 8:468–70.18. Scappaticcio L, Maiorino MI, Maio A, Esposito K, Bellastella G. Neutropenia in patients with hyperthyroidism: systematic review and meta-analysis. Clin Endocrinol (Oxf). 2021; 94:473–83.19. Wang MT, Lee WJ, Huang TY, Chu CL, Hsieh CH. Antithyroid drug-related hepatotoxicity in hyperthyroidism patients: a population-based cohort study. Br J Clin Pharmacol. 2014; 78:619–29.20. Suzuki N, Noh JY, Hiruma M, Kawaguchi A, Morisaki M, Ohye H, et al. Analysis of antithyroid drug-induced severe liver injury in 18,558 newly diagnosed patients with Graves’ disease in Japan. Thyroid. 2019; 29:1390–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Incidence & Prevalence of Hyperthyroidism and Preference for Therapeutic Modalities in Korea
- Prevalence and Annual Incidence of Thyroid Disease in Korea from 2006 to 2015: A Nationwide Population-Based Cohort Study
- Treatment of hyperthyroidism
- Evaluation of Thyroid Hormone Levels and Urinary Iodine Concentrations in Koreans Based on the Data from Korea National Health and Nutrition Examination Survey VI (2013 to 2015)
- Hyperthyroidism