Intest Res.
2023 Jul;21(3):375-384. 10.5217/ir.2022.00037.
Inflammatory bowel disease (IBD)-disk accurately predicts the daily life burden and parallels disease activity in patients with IBD
- Affiliations
-
- 1Department of Gastroenterology, Dayanand Medical College, Ludhiana, India
- 2Department of Internal Medicine, Dayanand Medical College, Ludhiana, India
- 3Research and Development Centre, Department of Gastroenterology, Dayanand Medical College, Ludhiana, India
- KMID: 2544760
- DOI: http://doi.org/10.5217/ir.2022.00037
Abstract
- Background/Aims
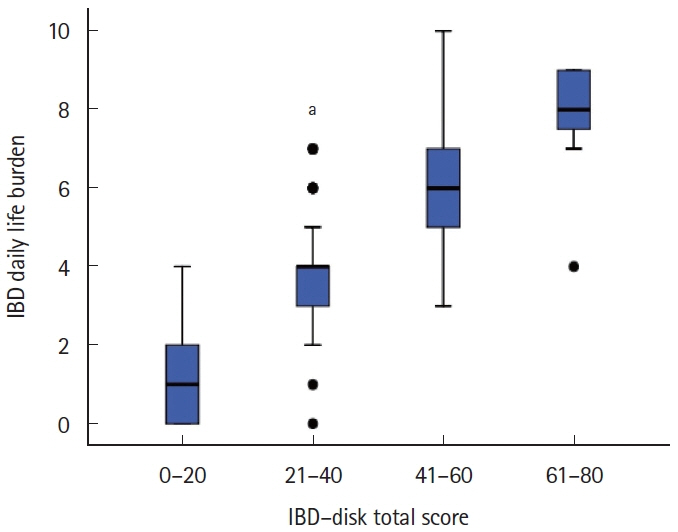
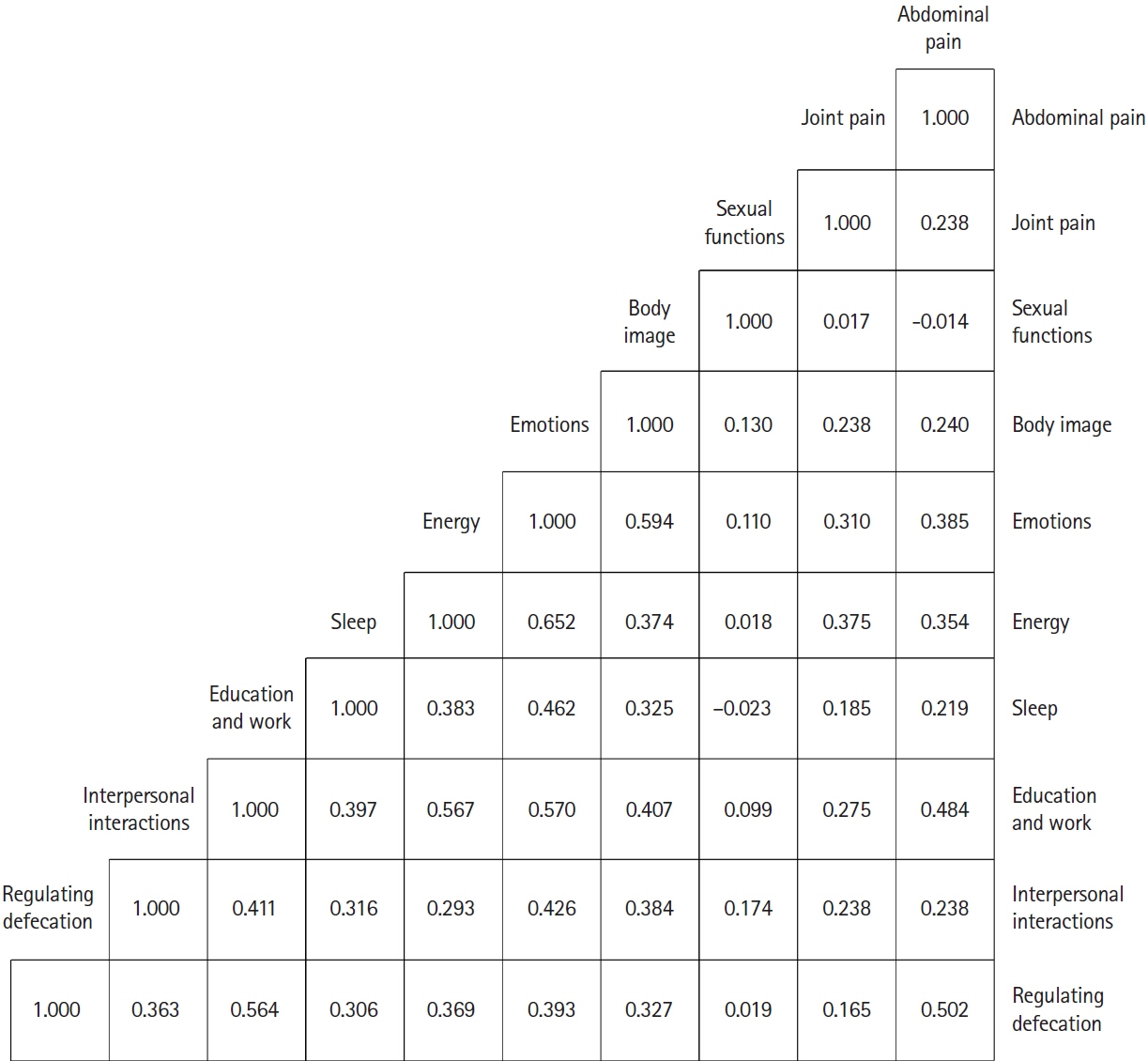
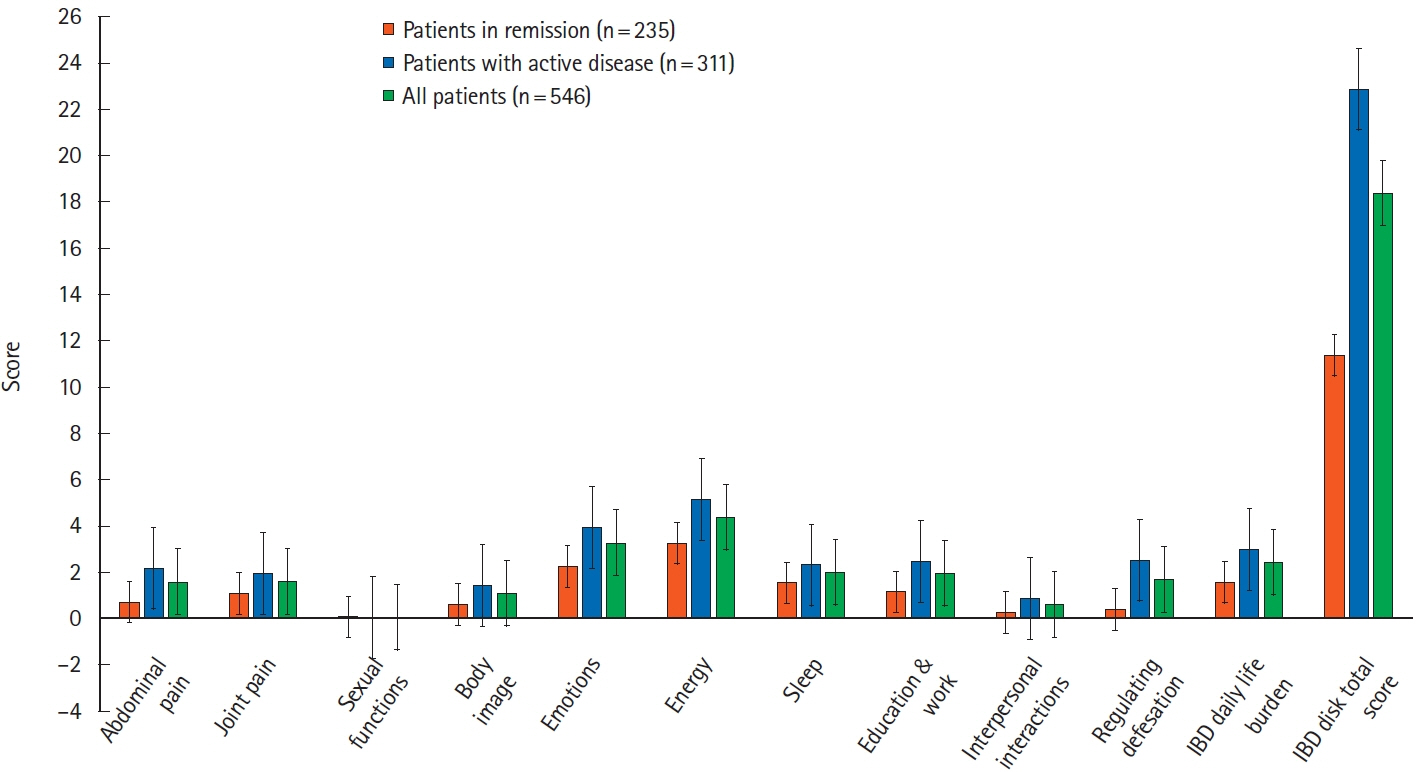
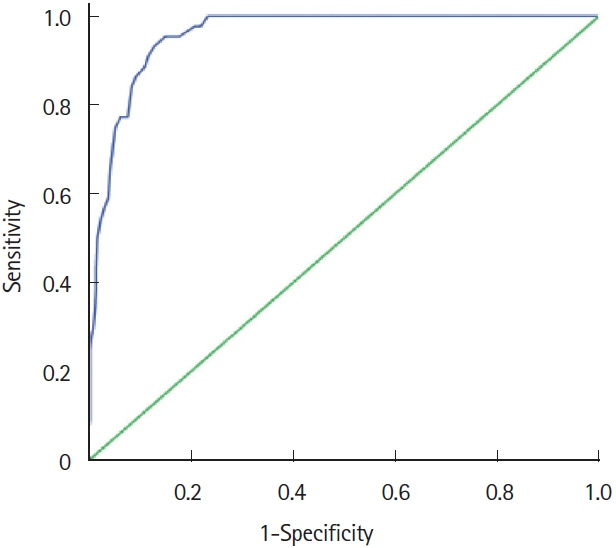
The inflammatory bowel disease (IBD)-disk is a validated, visual, 10-item, self-administered questionnaire used to evaluate IBD-related disability. The present study aimed to evaluate IBD-disk in assessment of IBD daily life burden and its relation with disease activity. Methods: A cross-sectional study was conducted between June 2021 and December 2021. Patients with IBD were asked to complete the IBD-disk and a visual analogue scale of IBD daily-life burden (scored from 0–10, score >5 indicative of high burden). The internal consistency of IBD-disk, correlation with IBD daily life burden and disease activity (assessed by partial Mayo score and Harvey Bradshaw Index in patients with ulcerative colitis [UC] and Crohn’s disease [CD], respectively) and diagnostic performance of IBD-disk to detect high burden were analyzed. Results: Out of the 546 patients (mean age 40.33±13.74 years, 282 [51.6%] males) who completed the IBD-disk, 464 (84.98%) had UC and the remaining (n=82, 15.02%) had CD. A total of 311 patients (291 UC and 20 CD; 56.95%) had active disease. The mean IBD-disk total score and IBD daily life burden were 18.39±15.23 and 2.45±2.02, respectively. The IBD-disk total score correlated strongly with the IBD daily life burden (ρ=0.94, P<0.001), moderately with partial Mayo score (ρ=0.50) and weakly with Harvey Bradshaw Index (ρ=0.34). The IBD-disk total score >30 predicted high IBD daily-life burden. Conclusions: The IBD-disk accurately predicts the daily life burden and parallels disease activity in patients with IBD and can be applied in clinical practice. (Intest Res, Published online)
Keyword
Figure
Reference
-
1. Ramos A, Calvet X, Sicilia B, et al. IBD-related work disability in the community: prevalence, severity and predictive factors: a cross-sectional study. United European Gastroenterol J. 2015; 3:335–342.
Article2. World Health Oraganization. International Classification of Functioning, Disability and Health (ICF) [Internet]. c2022 [cited 2022 Feb 21] https://www.who.int/standards/classifications/international-classification-of-functioning-disabilityand-health.3. Peyrin-Biroulet L, Cieza A, Sandborn WJ, et al. Development of the first disability index for inflammatory bowel disease based on the international classification of functioning, disability and health. Gut. 2012; 61:241–247.
Article4. Ghosh S, Louis E, Beaugerie L, et al. Development of the IBD disk: a visual self-administered tool for assessing disability in inflammatory bowel diseases. Inflamm Bowel Dis. 2017; 23:333–340.5. Le Berre C, Flamant M, Bouguen G, et al. VALIDation of the IBD-Disk instrument for assessing disability in inflammatory bowel diseases in a French cohort: the VALIDate Study. J Crohns Colitis. 2020; 14:1512–1523.
Article6. Gnambs T, Kaspar K. Disclosure of sensitive behaviors across self-administered survey modes: a meta-analysis. Behav Res Methods. 2015; 47:1237–1259.
Article7. Maaser C, Sturm A, Vavricka SR, et al. ECCO-ESGAR guideline for diagnostic assessment in IBD Part 1: initial diagnosis, monitoring of known IBD, detection of complications. J Crohns Colitis. 2019; 13:144–164.
Article8. Tadbiri S, Nachury M, Bouhnik Y, et al. The IBD-disk is a reliable tool to assess the daily-life burden of patients with inflammatory bowel disease. J Crohns Colitis. 2021; 15:766–773.
Article9. Sharma N, Savelkoul E, Disney B, et al. A multicenter study of patient acceptability of the IBD Disk tool and patient-reported disabilities. Dig Dis Sci. 2022; 67:457–462.
Article10. Satsangi J, Silverberg MS, Vermeire S, Colombel JF. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut. 2006; 55:749–753.
Article11. Lewis JD, Chuai S, Nessel L, Lichtenstein GR, Aberra FN, Ellenberg JH. Use of the noninvasive components of the Mayo score to assess clinical response in ulcerative colitis. Inflamm Bowel Dis. 2008; 14:1660–1666.
Article12. Turner D, Seow CH, Greenberg GR, Griffiths AM, Silverberg MS, Steinhart AH. A systematic prospective comparison of noninvasive disease activity indices in ulcerative colitis. Clin Gastroenterol Hepatol. 2009; 7:1081–1088.
Article13. Harvey RF, Bradshaw JM. A simple index of Crohn’s-disease activity. Lancet. 1980; 1:514.
Article14. Schober P, Boer C, Schwarte LA. Correlation coefficients: appropriate use and interpretation. Anesth Analg. 2018; 126:1763–1768.
Article15. Shafer LA, Sofia MA, Rubin DT, et al. An international multicenter comparison of IBD-related disability and validation of the IBDDI. Clin Gastroenterol Hepatol. 2021; 19:2524–2531.
Article16. Dang A, Kanukula R, Shah C, Shetye V. The emerging role of patient-reported outcomes (PROs) in clinical trials: an Indian perspective. Value Health Reg Issues. 2017; 12:24–26.
Article17. Zhao S, Wang J, Liu Y, et al. Inflammatory bowel diseases were associated with risk of sexual dysfunction in both sexes: a meta-analysis. Inflamm Bowel Dis. 2019; 25:699–707.
Article18. Zhang J, Wei S, Zeng Q, Wu X, Gan H. Prevalence and risk factors of sexual dysfunction in patients with inflammatory bowel disease: systematic review and meta-analysis. Int J Colorectal Dis. 2021; 36:2027–2038.
Article19. Beese SE, Harris IM, Dretzke J, Moore D. Body image dissatisfaction in patients with inflammatory bowel disease: a systematic review. BMJ Open Gastroenterol. 2019; 6:e000255.
Article20. Greuter T, Manser C, Pittet V, Vavricka SR, Biedermann L; on behalf of Swiss IBDnet, an official working group of the Swiss Society of Gastroenterology. Gender Differences in inflammatory bowel disease. Digestion. 2020; 101 Suppl 1:98–104.
Article21. Trindade IA, Ferreira C, Pinto-Gouveia J. The effects of body image impairment on the quality of life of non-operated Portuguese female IBD patients. Qual Life Res. 2017; 26:429–436.
Article22. Silva Mendes S, Ferreira P, Antunes P, et al. Validation of the IBD-Disk in a Portuguese cohort. Eur J Gastroenterol Hepatol. 2021; 33(1S Suppl 1):e961–e969.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Update on the epidemiology of inflammatory bowel disease in Asia: where are we now?
- Clostridioides Infection in Patients with Inflammatory Bowel Disease
- First aid with color atlas for the use of intestinal ultrasound for inflammatory bowel disease in daily clinical practice
- Pediatric Inflammatory Bowel Disease (IBD): Phenotypic, Genetic and Therapeutic Differences between Early-Onset and Adult-Onset IBD
- Sexual Dysfunction and Fertility Problems in Men with Inflammatory Bowel Disease