Pediatr Emerg Med J.
2023 Jul;10(3):94-98. 10.22470/pemj.2023.00710.
Impact of non-pharmaceutical interventions on the rate of respiratory viruses other than severe acute respiratory syndrome coronavirus 2 in the coronavirus disease 2019 pandemic
- Affiliations
-
- 1Department of Pediatrics, Wonkwang University Hospital, Iksan, Republic of Korea
- KMID: 2543576
- DOI: http://doi.org/10.22470/pemj.2023.00710
Abstract
- Purpose
We aimed to evaluate the impact of non-pharmaceutical interventions (NPIs) on the transmission of respiratory viruses other than severe acute respiratory syndrome coronavirus 2 among children during the coronavirus disease 2019 pandemic.
Methods
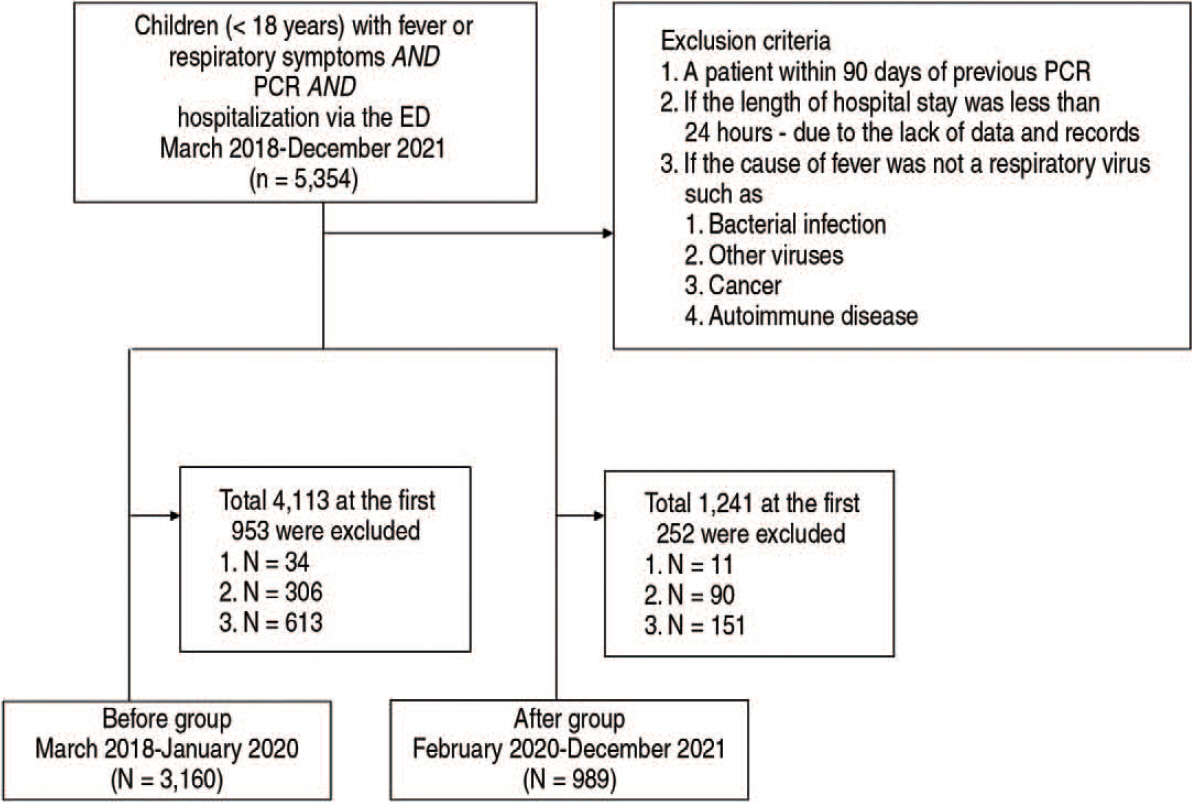
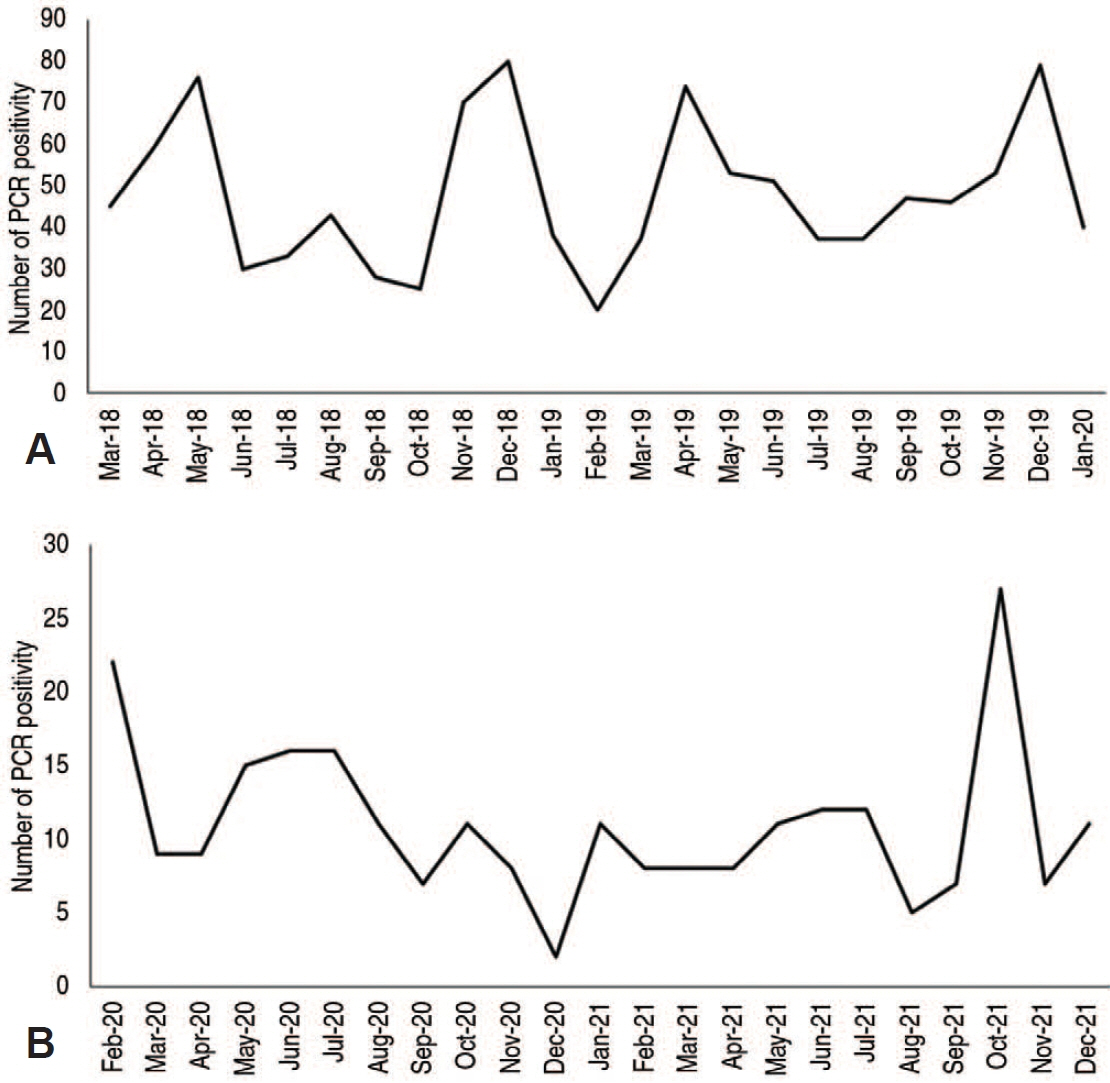
We analyzed the clinical and polymerase chain reaction (PCR) findings using electronic medical records of children (< 18 years) with fever or respiratory symptoms who were hospitalized via the emergency department of Wonkwang University Hospital (Iksan, Korea), from March 2018 through December 2021. The children were divided into before and after groups based on the hospitalization date relative to February 2020, starting point of the implementation of NPIs. PCR was performed using nasopharyngeal swab samples. Between the 2 groups, we compared age, sex, length of hospital stay, and PCR findings.
Results
The before and after groups consisted of 3,160 and 989, respectively, showing a 68.7% decrease in the number of children undergoing PCRs after the implantation of NPIs. The after group showed higher median values of the age and length of hospital stay than the before group (Ps < 0.001). A 76.9% decrease was noted in the number of children having PCR positivities (from 1,101 [34.8%] to 254 [25.7%]; P < 0.001). Among detected viruses, an increase in the proportion was noted only in human bocavirus (from 81 [2.6%] to 54 [5.5%]; P < 0.001). In contrast, significant decreases in the proportions were found in adenovirus, enterovirus, influenza A and B, respiratory syncytial viruses A and B, human coronaviruses (229E, NL63, and OC43) and human metapneumovirus.
Conclusion
NPIs may be effective in reducing the transmission of respiratory viruses other than severe acute respiratory syndrome coronavirus 2 among children during the pandemic.
Keyword
Figure
Reference
-
References
1. Gostin LO, Wiley LF. Governmental public health powers during the COVID-19 pandemic: stay-at-home orders, business closures, and travel restrictions. JAMA. 2020; 323:2137–8.
Article2. Ahn JG. Epidemiological changes in infectious diseases during the coronavirus disease 2019 pandemic in Korea: a systematic review. Clin Exp Pediatr. 2022; 65:167–71.
Article3. Central Disease Control Headquarters, Central Disaster Management Headquarters. COVID-19 response guidelines (for local governments) 9-5th ed [Internet]. Cheongju, Korea: Korea Disease Control and Prevention Agency; c2019 [cited 2021 Jan 22]. Available from: https://policy.nl.go.kr/search/searchDetail.do?rec_key=SH2_PLC20210260008. Korean.4. Kutter JS, Spronken MI, Fraaij PL, Fouchier RA, Herfst S. Transmission routes of respiratory viruses among humans. Curr Opin Virol. 2018; 28:142–51.
Article5. Gerba CP. Environmentally transmitted pathogens. In : Pepper IL, Gerba CP, Gentry TJ, editors. Environmental microbiology. 3rd ed. San Diego (CA): Academic Press;2015. p. 509–50.6. Ison MG, Lee N. Noninfluenza respiratory viruses. In : Cohen J, Powderly WG, Opal SM, editors. Infectious diseases. 4th ed. Amsterdam: Elsevier;2017. p. 1472–1482.e5.7. Karimzadeh S, Bhopal R, Nguyen Tien H. Review of infective dose, routes of transmission and outcome of COVID-19 caused by the SARS-COV-2: comparison with other respiratory viruses. Epidemiol Infect. 2021; 149:e96.
Article8. Fletcher GJ, Christopher S, Gnanamony M. Why does size matter for viruses--a new paradigm on viral size. Med Hypotheses. 2009; 73:133–7.9. Gelderblom HR. Structure and classification of viruses. In: Albrecht T, Baron S, National Center for Biotechnology Information, editors. Medical microbiology. 4th ed. Galveston (TX): Department of Microbiology & Immunology, University of Texas Medical Branch; 1996.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lessons Learned from SARS-CoV and MERS-CoV: Preparation for SARS-CoV-2 induced COVID-19
- Epidemiology, virology, and clinical features of severe acute respiratory syndrome -coronavirus-2 (SARS-CoV-2; Coronavirus Disease-19)
- Epidemiology, Virology, and Clinical Features of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2; Coronavirus Disease-19)
- Clinical and Epidemiological Characteristics of Coronavirus Disease 2019 in the Early Stage of Outbreak
- Coronavirus Disease 2019-Liver InjuryLiterature Review and Guidelines Based on the Recommendations of Hepatological Societies