J Neurocrit Care.
2023 Jun;16(1):51-52. 10.18700/jnc.220084.
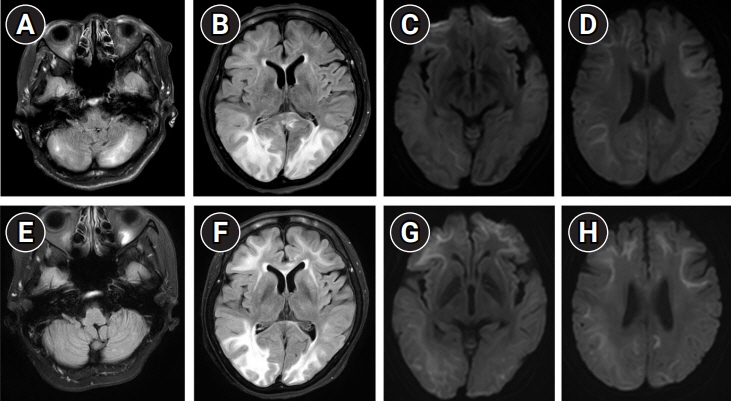
Posterior reversible encephalopathy syndrome superimposed on neuronal intranuclear inclusion disease
- Affiliations
-
- 1Department of Neurology, Hanyang University College of Medicine, Seoul, Korea
- KMID: 2543394
- DOI: http://doi.org/10.18700/jnc.220084
Figure
Reference
-
1. Triplett JD, Kutlubaev MA, Kermode AG, Hardy T. Posterior reversible encephalopathy syndrome (PRES): diagnosis and management. Pract Neurol. 2022; 22:183–9.2. Fugate JE, Rabinstein AA. Posterior reversible encephalopathy syndrome: clinical and radiological manifestations, pathophysiology, and outstanding questions. Lancet Neurol. 2015; 14:914–25.3. Sone J, Mori K, Inagaki T, Katsumata R, Takagi S, Yokoi S, et al. Clinicopathological features of adult-onset neuronal intranuclear inclusion disease. Brain. 2016; 139(Pt 12):3170–86.4. Chi X, Li M, Huang T, Tong K, Xing H, Chen J. Neuronal intranuclear inclusion disease with mental abnormality: a case report. BMC Neurol. 2020; 20:356.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Posterior reversible encephalopathy syndrome and reversible cerebral vasoconstriction syndrome associated with acute exacerbation of chronic obstructive pulmonary disease
- Posterior Reversible Encephalopathy Syndrome in a Patient with Intoxication of Arisaema amurense
- Neuronal Intranuclear Inclusion Disease with Abnormal Peripheral Nerve Conduction
- Posterior Reversible Encephalopathy Syndrome after Massive Blood Transfusion in a Normotensive Patient
- A Case of Posterior Reversible Encephalopathy Syndrome in a Patient having Continuous Ambulatory Peritoneal Dialysis