Nutr Res Pract.
2023 Jun;17(3):464-474. 10.4162/nrp.2023.17.3.464.
Resting energy expenditure in Korean type 2 diabetes patients: comparison between measured and predicted values
- Affiliations
-
- 1Department of Food and Nutrition, Changwon National University, Changwon 51140, Korea
- 2Department of Endocrinology, Changwon Fatima Hospital, Changwon 51394, Korea
- 3Interdisciplinary Program in Senior Human Ecology, Changwon National University, Changwon 51140, Korea
- KMID: 2542843
- DOI: http://doi.org/10.4162/nrp.2023.17.3.464
Abstract
- BACKGROUND/OBJECTIVES
Estimation of energy demand using resting energy expenditure (REE) is a reasonable approach for optimizing glycemic control and weight management in patients with type 2 diabetes mellitus (T2DM). This study aimed to compare REE predictions and objective measurements in patients with T2DM in Korea.
SUBJECTS/METHODS
This study enrolled 36 participants with T2DM (age range, 20–60 years). Anthropometric variables including height, weight, waist-hip ratio, blood pressure, body fat, body fat percentage, and total body weight were measured using bioimpedance. REE was evaluated using indirect calorimetry. The measured REE values were compared to values estimated using five predictive equations: the Harris-Benedict, Mifflin, Owen, Food and Agriculture Organization of the United Nations/World Health Organization (FAO/WHO), and Schofield equations. This study evaluated the associations between measured REE values and anthropometric/clinical data, including height, weight, and age, using multivariate linear regression.
RESULTS
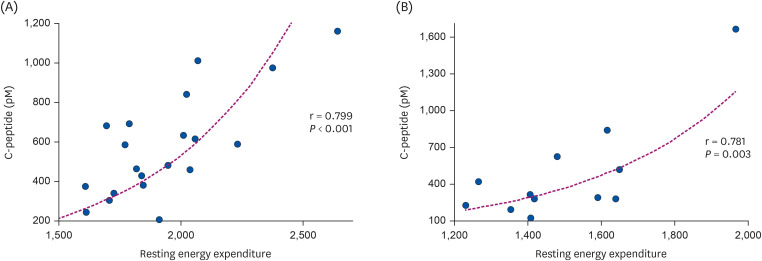
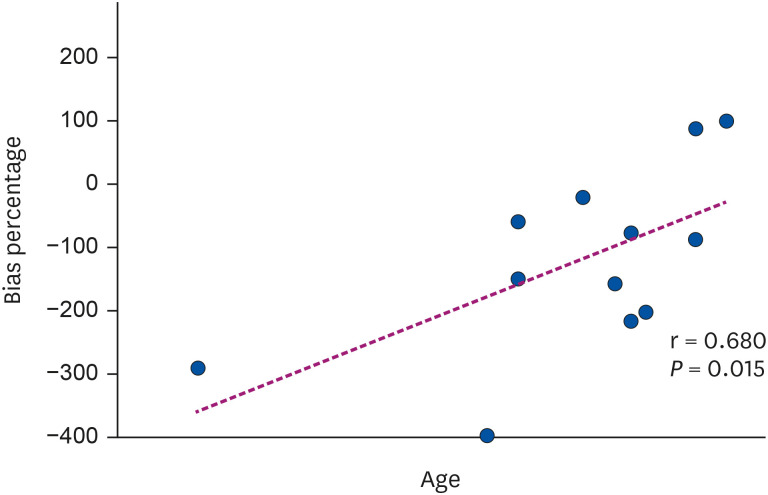
The mean measured REE value was 1891.79 ± 288.03 kcal/day (male), 1,502.00 ± 202.96 kcal/day (female). REE estimates generated from the Mifflin equation showed the largest differences from measured REE values, whereas estimates derived from the FAO/ WHO equation were the closest to the measured REE values. This study also identified associations between measured REE values and various anthropometric/clinical variables.
CONCLUSION
The accuracy of REE prediction equations is critically important in promoting the efficacy of dietary counseling and the effective treatment of diabetes. Our results indicate the need for additional studies informing more suitable methods for determining the energy requirements of Korean patients with T2DM.
Keyword
Figure
Reference
-
1. Kim DJ, Lee MS, Kim KW, Lee MK. Insulin secretory dysfunction and insulin resistance in the pathogenesis of Korean type 2 diabetes mellitus. Metabolism. 2001; 50:590–593. PMID: 11319722.2. International Diabetes Federation. Diabetes atlas 7th edition [Internet]. Brussels: International Diabetes Federation;c2022. cited 2022 May 10. Available from: http://www.diabetesatlas.org.3. Yoon KH, Lee JH, Kim JW, Cho JH, Choi YH, Ko SH, Zimmet P, Son HY. Epidemic obesity and type 2 diabetes in Asia. Lancet. 2006; 368:1681–1688. PMID: 17098087.4. Ministry of Health and Welfare, Korea Disease Control and Prevention Agency. Korea Health Statistics 2019: Korea National Health and Nutrition Examination Survey (KNHANES VI-3). Cheongju: Korea Disease Control and Prevention Agency;2020.5. Beckman JA, Creager MA, Libby P. Diabetes and atherosclerosis: epidemiology, pathophysiology, and management. JAMA. 2002; 287:2570–2581. PMID: 12020339.6. Evert AB, Boucher JL, Cypress M, Dunbar SA, Franz MJ, Mayer-Davis EJ, Neumiller JJ, Nwankwo R, Verdi CL, Urbanski P, et al. Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care. 2013; 36:3821–3842. PMID: 24107659.7. American Diabetes Association (ADA). Standards of medical care in diabetes: Lifestyle management. Diabetes Care. 2018; 41:S38–S50. PMID: 29222375.8. Compher C, Frankenfield D, Keim N, Roth-Yousey L. Evidence Analysis Working Group. Best practice methods to apply to measurement of resting metabolic rate in adults: a systematic review. J Am Diet Assoc. 2006; 106:881–903. PMID: 16720129.9. Hill JO, Wyatt HR, Peters JC. The importance of energy balance. Eur Endocrinol. 2013; 9:111–115. PMID: 29922364.10. Wang Z, Heshka S, Gallagher D, Boozer CN, Kotler DP, Heymsfield SB. Resting energy expenditure-fat-free mass relationship: new insights provided by body composition modeling. Am J Physiol Endocrinol Metab. 2000; 279:E539–E545. PMID: 10950820.11. Delsoglio M, Achamrah N, Berger MM, Pichard C. Indirect calorimetry in clinical practice. J Clin Med. 2019; 8:1387. PMID: 31491883.12. Harris JA, Benedict FG. A biometric study of human basal metabolism. Proc Natl Acad Sci U S A. 1918; 4:370–373. PMID: 16576330.13. Mifflin MD, St Jeor ST, Hill LA, Scott BJ, Daugherty SA, Koh YO. A new predictive equation for resting energy expenditure in healthy individuals. Am J Clin Nutr. 1990; 51:241–247. PMID: 2305711.14. Schofield WN. Predicting basal metabolic rate, new standards and review of previous work. Hum Nutr Clin Nutr. 1985; 39(Suppl 1):5–41. PMID: 4044297.15. Food and Agriculture Organization of the United Nations (FAO). Energy and Protein Requirements: Report of a joint FAO/WHO/UNO Expert Consultation. Geneva: World Health Organization;1985.16. Sabounchi NS, Rahmandad H, Ammerman A. Best-fitting prediction equations for basal metabolic rate: informing obesity interventions in diverse populations. Int J Obes. 2013; 37:1364–1370.17. Madden AM, Mulrooney HM, Shah S. Estimation of energy expenditure using prediction equations in overweight and obese adults: a systematic review. J Hum Nutr Diet. 2016; 29:458–476. PMID: 26923904.18. de Figueiredo Ferreira M, Detrano F, Coelho GM, Barros ME, Serrão Lanzillotti R, Firmino Nogueira Neto J, Portella ES, Serrão Lanzillotti H, Soares Ede A. Body composition and basal metabolic rate in women with type 2 diabetes mellitus. J Nutr Metab. 2014; 2014:574057. PMID: 25436144.19. Miyake R, Ohkawara K, Ishikawa-Takata K, Morita A, Watanabe S, Tanaka S. Obese Japanese adults with type 2 diabetes have higher basal metabolic rates than non-diabetic adults. J Nutr Sci Vitaminol (Tokyo). 2011; 57:348–354. PMID: 22293212.20. Alawad AO, Merghani TH, Ballal MA. Resting metabolic rate in obese diabetic and obese non-diabetic subjects and its relation to glycaemic control. BMC Res Notes. 2013; 6:382. PMID: 24070224.21. Ikeda K, Fujimoto S, Goto M, Yamada C, Hamasaki A, Shide K, Kawamura T, Inagaki N. Impact of endogenous and exogenous insulin on basal energy expenditure in patients with type 2 diabetes under standard treatment. Am J Clin Nutr. 2011; 94:1513–1518. PMID: 22049163.22. Miyake R, Tanaka S, Ohkawara K, Ishikawa-Takata K, Hikihara Y, Taguri E, Kayashita J, Tabata I. Validity of predictive equations for basal metabolic rate in Japanese adults. J Nutr Sci Vitaminol (Tokyo). 2011; 57:224–232. PMID: 21908945.23. Tabata S, Kinoshita N, Yamada S, Matsumoto H. Accuracy of basal metabolic rate estimated by predictive equations in Japanese with type 2 diabetes. Asia Pac J Clin Nutr. 2018; 27:763–769. PMID: 30045419.24. Son HR, Yeon SE, Choi JS, Kim EK. The measurements of the resting metabolic rate (RMR) and the accuracy of RMR predictive equations for Korean farmers. Korean J Community Nutr. 2014; 19:568–580.25. Behera KK, Joseph M, Shetty SK, Chacko A, Sahoo MK, Mahendri NV, Nair V, Nadig S, Thomas N. Resting energy expenditure in subjects with fibro-calculous pancreatic diabetes. J Diabetes. 2014; 6:158–163. PMID: 23773615.26. Ramos FM, Rossato LT, Ramires BR, Pimentel GD, Venâncio LS, Orsatti FL, de Oliveira EP. Comparison of predictive equations of resting energy expenditure in older adults with chronic obstructive pulmonary disease. Rev Port Pneumol (2006). 2017; 23:40–42. PMID: 27771344.27. Khor SM, Mohd BB. Assessing the resting energy expenditure of cancer patients in the Penang General Hospital. Malays J Nutr. 2011; 17:43–53. PMID: 22135864.28. Frankenfield D, Roth-Yousey L, Compher C. Comparison of predictive equations for resting metabolic rate in healthy nonobese and obese adults: a systematic review. J Am Diet Assoc. 2005; 105:775–789. PMID: 15883556.29. Gougeon R. Thermic and metabolic responses to oral glucose in obese subjects with non-insulin-dependent diabetes mellitus treated with insulin or a very-low-energy diet. Am J Clin Nutr. 1996; 64:78–86. PMID: 8669419.30. Nyenwe EA, Ogwo CC, Owei I, Wan JY, Dagogo-Jack S. Parental history of type 2 diabetes is associated with lower resting energy expenditure in normoglycemic subjects. BMJ Open Diabetes Res Care. 2018; 6:e000511.31. Taguchi M, Ishikawa-Takata K, Tatsuta W, Katsuragi C, Usui C, Sakamoto S, Higuchi M. Resting energy expenditure can be assessed by fat-free mass in female athletes regardless of body size. J Nutr Sci Vitaminol (Tokyo). 2011; 57:22–29. PMID: 21512287.32. Heshka S, Feld K, Yang MU, Allison DB, Heymsfield SB. Resting energy expenditure in the obese: a cross-validation and comparison of prediction equations. J Am Diet Assoc. 1993; 93:1031–1036. PMID: 8360408.33. Hunter GR, Weinsier RL, Gower BA, Wetzstein C. Age-related decrease in resting energy expenditure in sedentary white women: effects of regional differences in lean and fat mass. Am J Clin Nutr. 2001; 73:333–337. PMID: 11157332.34. Elia M, Ritz P, Stubbs RJ. Total energy expenditure in the elderly. Eur J Clin Nutr. 2000; 54(Suppl 3):S92–103. PMID: 11041080.35. Poehlman ET, Toth MJ, Webb GD. Sodium-potassium pump activity contributes to the age-related decline in resting metabolic rate. J Clin Endocrinol Metab. 1993; 76:1054–1057. PMID: 8386182.36. Melanson EL, Gavin KM, Shea KL, Wolfe P, Wierman ME, Schwartz RS, Kohrt WM. Regulation of energy expenditure by estradiol in premenopausal women. J Appl Physiol. 2015; 119:975–981. PMID: 26338457.37. Park JS, Yim JE. Comparison of predicted and measured resting energy expenditure in overweight and obese Korean women. Korean J Community Nutr. 2018; 23:424–430.38. Buscemi S, Donatelli M, Grosso G, Vasto S, Galvano F, Costa F, Rosafio G, Verga S. Resting energy expenditure in type 2 diabetic patients and the effect of insulin bolus. Diabetes Res Clin Pract. 2014; 106:605–610. PMID: 25312871.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Predicted and Measured Resting Energy Expenditure in Overweight and Obese Korean Women
- Comparision of measured resting energy expenditure by indirect calorimetry and predicted value in the obese
- Energy Expenditure in Young Adults and Newborns by Indirect Calorimetry
- Accuracy of Predictive Equations for Resting Metabolic Rates and Daily Energy Expenditures of Police Officials Doing Shift Work by Type of Work
- A Comparison of Energy Intake and Energy Expenditure in Normal-Weight and Over-Weight Korean Adults