Child Kidney Dis.
2022 Dec;26(2):107-110. 10.3339/ckd.22.038.
Desmopressin responding female nephrogenic diabetes insipidus: a case report
- Affiliations
-
- 1Department of Pediatrics, Ajou University School of Medicine, Suwon, Republic of Korea
- 2Department of Pediatrics, Hallym University Sacred Heart Hospital, Anyang, Republic of Korea
- 3Department of Pediatrics, Ewha Womans University College of Medicine, Seoul, Republic of Korea
- KMID: 2538743
- DOI: http://doi.org/10.3339/ckd.22.038
Abstract
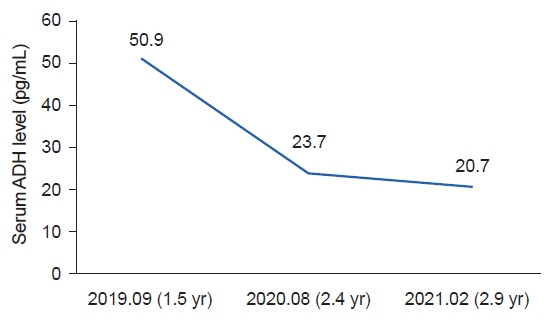
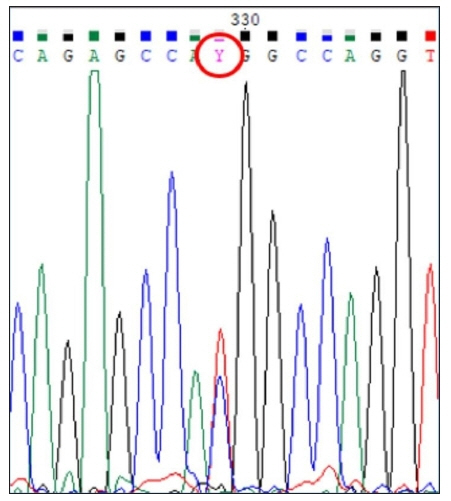
- Nephrogenic diabetes insipidus, decreased ability to concentrate urine, with production of large amounts of urine, is caused by the refractory response of renal tubules to the action of antidiuretic hormone. This rare disorder, known as X-linked nephrogenic diabetes insipidus, is caused by a mutation in the arginine vasopressin receptor 2 gene. Because it is hereditary, most patients are male. This report highlights a case of nephrogenic diabetes insipidus in a 3-year 5-month-old female; upon presentation to the hospital, her symptoms included frequent urination and consumption of a significant amount of water, which had begun 2 years ago. The results of blood tests showed increased levels of serum antidiuretic hormone, and sellar magnetic resonance imaging showed no abnormality. The results of the water restriction test and the desmopressin administration test confirmed the diagnosis of nephrogenic diabetes insipidus showing a partial response to desmopressin. The results of genetic testing indicated the presence of an arginine vasopressin receptor 2 mutation, a heterozygous missense mutation (p.Val88Met), suggesting inheritance of X-linked nephrogenic diabetes insipidus. This report describes a significant case of symptomatic X-linked nephrogenic diabetes insipidus in a female patient who showed a partial response to desmopressin.
Figure
Reference
-
References
1. Kim MJ, Cho JY, Park JS, Park ES, Seo JH, Lim JY, et al. A case of nephrogenic diabetes insipidus with a rare x-linked recessive mutation in an infant with developmental and growth retardation tracked by the Korean National Health Screening Program. Child Kidney Dis. 2020; 24:131–7.
Article2. Arthus MF, Lonergan M, Crumley MJ, Naumova AK, Morin D, De Marco LA, et al. Report of 33 novel AVPR2 mutations and analysis of 117 families with X-linked nephrogenic diabetes insipidus. J Am Soc Nephrol. 2000; 11:1044–54.3. Spanakis E, Milord E, Gragnoli C. AVPR2 variants and mutations in nephrogenic diabetes insipidus: review and missense mutation significance. J Cell Physiol. 2008; 217:605–17.
Article4. Ding C, Beetz R, Rittner G, Bartsch O. A female with X-linked nephrogenic diabetes insipidus in a family with inherited central diabetes insipidus: case report and review of the literature. Am J Med Genet A. 2020; 182:1032–40.
Article5. Rege T, Polsani S, Jim B. A rare case of congenital diabetes insipidus. Front Med (Lausanne). 2015; 2:43.
Article6. Bockenhauer D, Carpentier E, Rochdi D, van't Hoff W, Breton B, Bernier V, et al. Vasopressin type 2 receptor V88M mutation: molecular basis of partial and complete nephrogenic diabetes insipidus. Nephron Physiol. 2010; 114:1–10.
Article7. Ishida A, Mizuno H, Aoyama K, Sasaki S, Negishi Y, Arakawa T, et al. Partial nephrogenic diabetes insipidus with a novel arginine vasopressin receptor 2 gene variant. Clin Pediatr Endocrinol. 2022; 31:44–9.
Article8. Kim WK, Lee JS, Ha TS. A familial case of nephrogenic diabetes insipidus associated with a mutation of the AVPR2 gene. J Korean Soc Pediatr Nephrol. 2011; 15:172–8.
Article9. Garcia Castano A, Perez de Nanclares G, Madariaga L, Aguirre M, Chocron S, Madrid A, et al. Novel mutations associated with nephrogenic diabetes insipidus: a clinical-genetic study. Eur J Pediatr. 2015; 174:1373–85.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Nephrogenic Diabetes Insipidus Associated with Hydronephrosis
- A case of nephrogenic diabetes insipidus associated with urinary incontinence
- Nephrogenic Diabetes Insipidus Associated with Nonobstructive Dilation of the Urinary Tract and Voiding Difficulty
- A case of nephrogenic diabetes insipidus due to vesicoureteral reflux
- A Familial Case of Nephrogenic Diabetes Insipidus Associated with a Mutation of the AVPR2 Gene