J Rhinol.
2022 Nov;29(3):127-133. 10.18787/jr.2022.00407.
Practical Review of Olfactory Training and COVID-19
- Affiliations
-
- 1Department of Otolaryngology-Head and Neck Surgery, Bucheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea
- 2Department of Otolaryngology-Head and Neck Surgery, Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea
- 3Department of Otorhinolaryngology-Head and Neck Surgery, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Republic of Korea
- KMID: 2536580
- DOI: http://doi.org/10.18787/jr.2022.00407
Abstract
- Olfactory disorders one of the most frequent distinctive symptoms of COVID-19 infection. COVID-19-induced olfactory disorder can be classified as post-infectious olfactory dysfunction (PIOD). The effect of drugs on olfactory disorder following upper respiratory infection, including PIOD, has not been clearly established, which adds to the difficulty with treating the disorder. However, the effect of olfactory training on PIOD has been confirmed by numerous studies. As such, olfactory training is gaining attention, and has taken on greater importance, as the sole treatment for COVID-19–induced olfactory disorder in this pandemic age. This review describes the effect of olfactory training for COVID-19–induced olfactory disorder by analyzing the relevant literature.
Figure
Cited by 1 articles
-
Efficacy of Steroid-Impregnated Spacers After Endoscopic Sinus Surgery in Chronic Rhinosinusitis: A Systematic Review and Meta-Analysis
Se Hwan Hwang, Sung Won Kim, Mohammed Abdullah Basurrah, Do Hyun Kim
Clin Exp Otorhinolaryngol. 2023;16(2):148-158. doi: 10.21053/ceo.2022.01718.
Reference
-
References
1. Brämerson A, Johansson L, Ek L, Nordin S, Bende M. Prevalence of olfactory dysfunction: the Skövde population-based study. Laryngoscope. 2004; 114(4):733–7.
Article2. Croy I, Nordin S, Hummel T. Olfactory disorders and quality of life--an updated review. Chem Senses. 2014; 39(3):185–94.
Article3. Croy I, Hummel T. Olfaction as a marker for depression. J Neurol. 2017; 264(4):631–8.
Article4. Temmel AF, Quint C, Schickinger-Fischer B, Klimek L, Stoller E, Hummel T. Characteristics of olfactory disorders in relation to major causes of olfactory loss. Arch Otolaryngol Head Neck Surg. 2002; 128(6):635–41.
Article5. Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. JAMA. 2020; 324(8):782–93.
Article6. Saniasiaya J, Islam MA, Abdullah B. Prevalence of olfactory dysfunction in coronavirus disease 2019 (COVID‐19): a meta‐analysis of 27,492 patients. Laryngoscope. 2021; 131(4):865–78.7. Kowalski LP, Sanabria A, Ridge JA, Ng WT, de Bree R, Rinaldo A, et al. COVID-19 pandemic: effects and evidence-based recommendations for otolaryngology and head and neck surgery practice. Head Neck. 2020; 42(6):1259–67.8. Menni C, Valdes AM, Freidin MB, Sudre CH, Nguyen LH, Drew DA, et al. Real-time tracking of self-reported symptoms to predict potential COVID-19. Nat Med. 2020; 26(7):1037–40.
Article9. Gerkin RC, Ohla K, Veldhuizen MG, Joseph PV, Kelly CE, Bakke AJ, et al. Recent smell loss is the best predictor of COVID-19 among individuals with recent respiratory symptoms. Chem Senses. 2021; 46:bjaa081.10. Kirschenbaum D, Imbach LL, Ulrich S, Rushing EJ, Keller E, Reimann RR, et al. Inflammatory olfactory neuropathy in two patients with COVID-19. Lancet. 2020; 396(10245):166.
Article11. Torabi A, Mohammadbagheri E, Akbari Dilmaghani N, Bayat AH, Fathi M, Vakili K, et al. Proinflammatory cytokines in the olfactory mucosa result in COVID-19 induced anosmia. ACS Chem Neurosci. 2020; 11(13):1909–13.
Article12. Vaira LA, Hopkins C, Petrocelli M, Lechien JR, Cutrupi S, Salzano G, et al. Efficacy of corticosteroid therapy in the treatment of long- lasting olfactory disorders in COVID-19 patients. Rhinology. 2021; 59(1):21–5.
Article13. Hummel T, Rissom K, Reden J, Hähner A, Weidenbecher M, Hüttenbrink KB. Effects of olfactory training in patients with olfactory loss. Laryngoscope. 2009; 119(3):496–9.
Article14. Konstantinidis I, Tsakiropoulou E, Constantinidis J. Long term effects of olfactory training in patients with post-infectious olfactory loss. Rhinology. 2016; 54(2):170–5.
Article15. Damm M, Pikart LK, Reimann H, Burkert S, Göktas Ö, Haxel B, et al. Olfactory training is helpful in postinfectious olfactory loss: a randomized, controlled, multicenter study. Laryngoscope. 2014; 124(4):826–31.
Article16. Luskin MB. Restricted proliferation and migration of postnatally generated neurons derived from the forebrain subventricular zone. Neuron. 1993; 11(1):173–89.
Article17. Lois C, Alvarez-Buylla A. Long-distance neuronal migration in the adult mammalian brain. Science. 1994; 264(5162):1145–8.
Article18. Youngentob SL, Kent PF. Enhancement of odorant-induced mucosal activity patterns in rats trained on an odorant identification task. Brain Res. 1995; 670(1):82–8.
Article19. Wang HW, Wysocki CJ, Gold GH. Induction of olfactory receptor sensitivity in mice. Science. 1993; 260(5110):998–1000.
Article20. Jones SV, Choi DC, Davis M, Ressler KJ. Learning-dependent structural plasticity in the adult olfactory pathway. J Neurosci. 2008; 28(49):13106–11.
Article21. Wang L, Chen L, Jacob T. Evidence for peripheral plasticity in human odour response. J Physiol. 2004; 554(Pt 1):236–44.
Article22. Li W, Luxenberg E, Parrish T, Gottfried JA. Learning to smell the roses: experience-dependent neural plasticity in human piriform and orbitofrontal cortices. Neuron. 2006; 52(6):1097–108.
Article23. Kollndorfer K, Kowalczyk K, Hoche E, Mueller CA, Pollak M, Trattnig S, et al. Recovery of olfactory function induces neuroplasticity effects in patients with smell loss. Neural Plast. 2014; 2014:140419.
Article24. Negoias S, Pietsch K, Hummel T. Changes in olfactory bulb volume following lateralized olfactory training. Brain Imaging Behav. 2017; 11(4):998–1005.
Article25. Kim DH, Kim SW, Stybayeva G, Lim SY, Hwang SH. Predictive value of olfactory and taste symptoms in the diagnosis of COVID-19: a systematic review and meta-analysis. Clin Exp Otorhinolaryngol. 2021; 14(3):312–20.
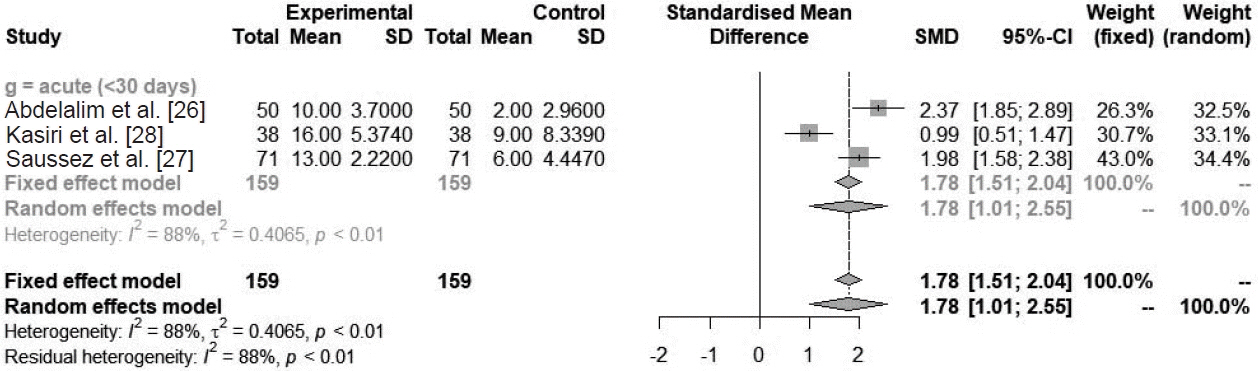
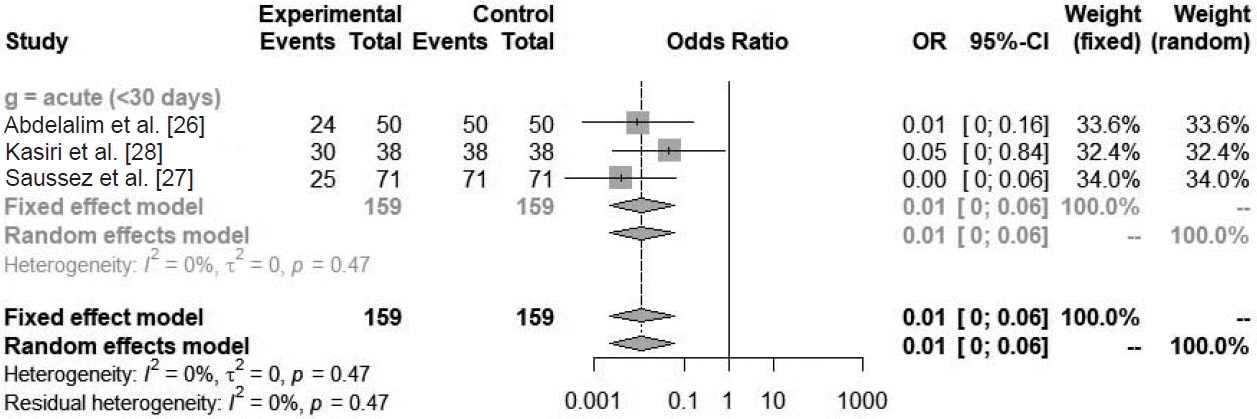
Article26. Abdelalim AA, Mohamady AA, Elsayed RA, Elawady MA, Ghallab AF. Corticosteroid nasal spray for recovery of smell sensation in COVID-19 patients: a randomized controlled trial. Am J Otolaryngol. 2021; 42(2):102884.
Article27. Saussez S, Vaira LA, Chiesa-Estomba CM, Bon SL, Horoi M, Deiana G, et al. Short-term efficacy and safety of oral and nasal corticosteroids in COVID-19 patients with olfactory dysfunction: a European multicenter study. Pathogens. 2021; 10(6):698.
Article28. Kasiri H, Rouhani N, Salehifar E, Ghazaeian M, Fallah S. Mometasone furoate nasal spray in the treatment of patients with COVID-19 olfactory dysfunction: a randomized, double blind clinical trial. Int Immunopharmacol. 2021; 98:107871.
Article29. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011; 343:d5928.
Article30. Harless L, Liang J. Pharmacologic treatment for postviral olfactory dysfunction: a systematic review. Int Forum Allergy Rhinol. 2016; 6(7):760–7.
Article31. Seo BS, Lee HJ, Mo JH, Lee CH, Rhee CS, Kim JW. Treatment of postviral olfactory loss with glucocorticoids, Ginkgo biloba, and mometasone nasal spray. Arch Otolaryngol Head Neck Surg. 2009; 135(10):1000–4.
Article32. Rashid RA, Zgair A, Al-Ani RM. Effect of nasal corticosteroid in the treatment of anosmia due to COVID-19: a randomised double-blind placebo-controlled study. Am J Otolaryngol. 2021; 42(5):103033.
Article33. Le Bon SD, Konopnicki D, Pisarski N, Prunier L, Lechien JR, Horoi M. Efficacy and safety of oral corticosteroids and olfactory training in the management of COVID-19-related loss of smell. Eur Arch Otorhinolaryngol. 2021; 278(8):3113–7.
Article34. Mazzatenta A, Neri G, D'Ardes D, De Luca C, Marinari S, Porreca E, et al. Smell and taste in severe CoViD-19: self-reported vs. testing. Front Med (Lausanne). 2020; 7:589409.
Article35. Sorokowska A, Drechsler E, Karwowski M, Hummel T. Effects of olfactory training: a meta-analysis. Rhinology. 2017; 55(1):17–26.
Article36. Pekala K, Chandra RK, Turner JH. Efficacy of olfactory training in patients with olfactory loss: a systematic review and meta-analysis. Int Forum Allergy Rhinol. 2016; 6(3):299–307.
Article37. Qiao XF, Wang GP, Li X, Bai YH, Zheng W. Analysis of the clinical effect of olfactory training on olfactory dysfunction after upper respiratory tract infection. Acta Otolaryngol. 2019; 139(7):643–6.
Article38. Oleszkiewicz A, Hanf S, Whitcroft KL, Haehner A, Hummel T. Examination of olfactory training effectiveness in relation to its complexity and the cause of olfactory loss. Laryngoscope. 2018; 128(7):1518–22.
Article39. Patel ZM. The evidence for olfactory training in treating patients with olfactory loss. Curr Opin Otolaryngol Head Neck Surg. 2017; 25(1):43–6.
Article40. Altundag A, Cayonu M, Kayabasoglu G, Salihoglu M, Tekeli H, Saglam O, et al. Modified olfactory training in patients with postinfectious olfactory loss. Laryngoscope. 2015; 125(8):1763–6.
Article41. Fleiner F, Lau L, Göktas Ö. Active olfactory training for the treatment of smelling disorders. Ear Nose Throat J. 2012; 91(5):198–215.
Article42. Kattar N, Do TM, Unis GD, Migneron MR, Thomas AJ, McCoul ED. Olfactory training for postviral olfactory dysfunction: systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2021; 164(2):244–54.
Article43. Kollndorfer K, Fischmeister FP, Kowalczyk K, Hoche E, Mueller CA, Trattnig S, et al. Olfactory training induces changes in regional functional connectivity in patients with long-term smell loss. Neuroimage Clin. 2015; 9:401–10.
Article44. Kim YK, Hong SL, Yoon EJ, Kim SE, Kim JW. Central presentation of postviral olfactory loss evaluated by positron emission tomography scan: a pilot study. Am J Rhinol Allergy. 2012; 26(3):204–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparative Analysis of Olfactory and Gustatory Function of Patients With COVID-19 Olfactory Dysfunction and Non-COVID-19 Postinfectious Olfactory Dysfunction
- Contemporary Review of Olfactory Dysfunction in COVID-19
- The Sniffing Bead System as a Useful Diagnostic Tool for Olfactory Dysfunction in COVID-19
- Clinical Features of Olfactory Dysfunction in COVID-19 Patients
- A review on photobiomodulation therapy for olfactory dysfunction caused by COVID-19