Korean J Orthod.
2022 Nov;52(6):451-460. 10.4041/kjod22.012.
Orthodontic treatment in a patient with Moebius syndrome: A case report
- Affiliations
-
- 1Department of Medicine, Gachon University Graduate School, Incheon, Korea
- 2Department of Orthodontics, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea
- KMID: 2536338
- DOI: http://doi.org/10.4041/kjod22.012
Abstract
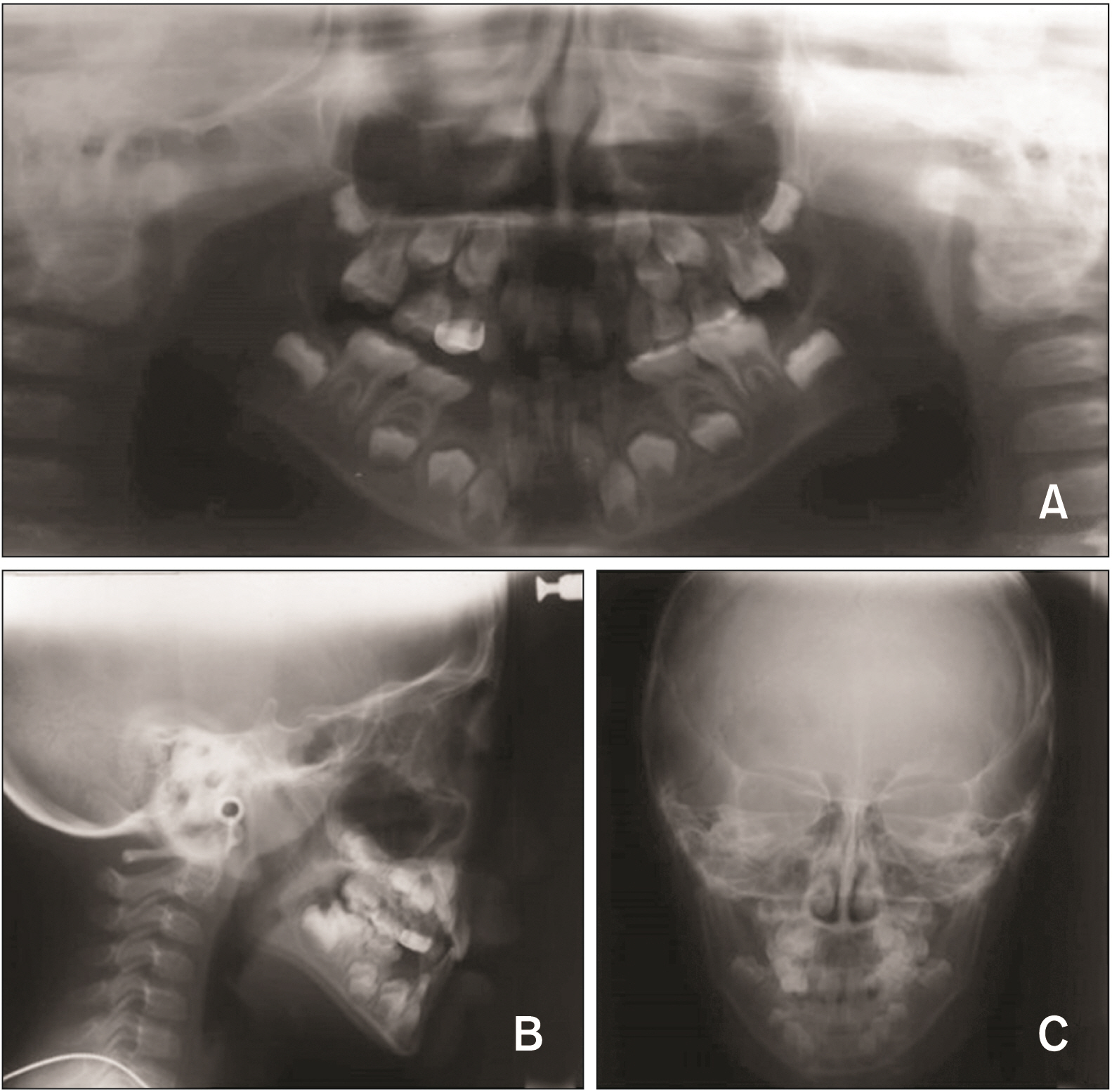
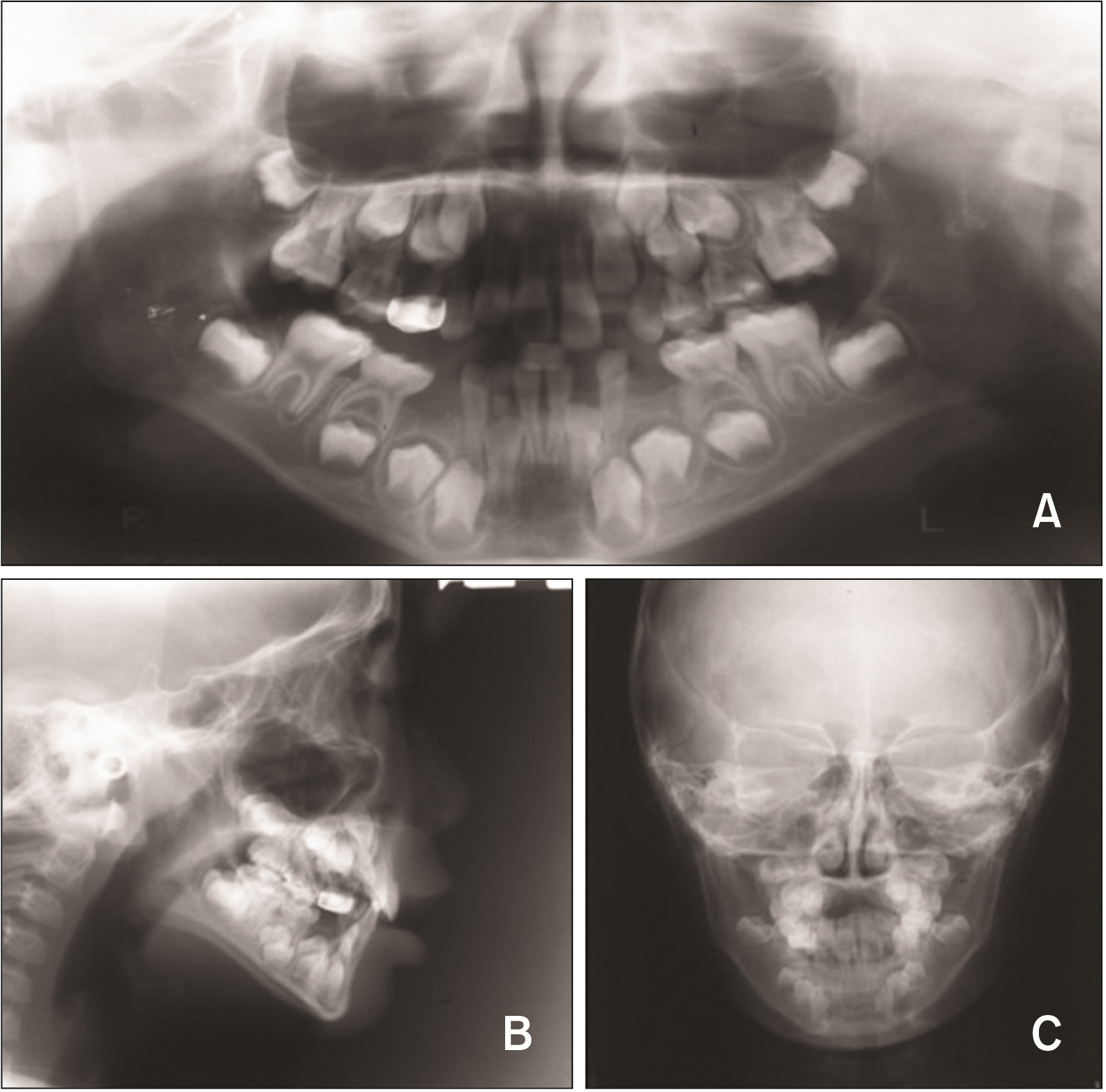
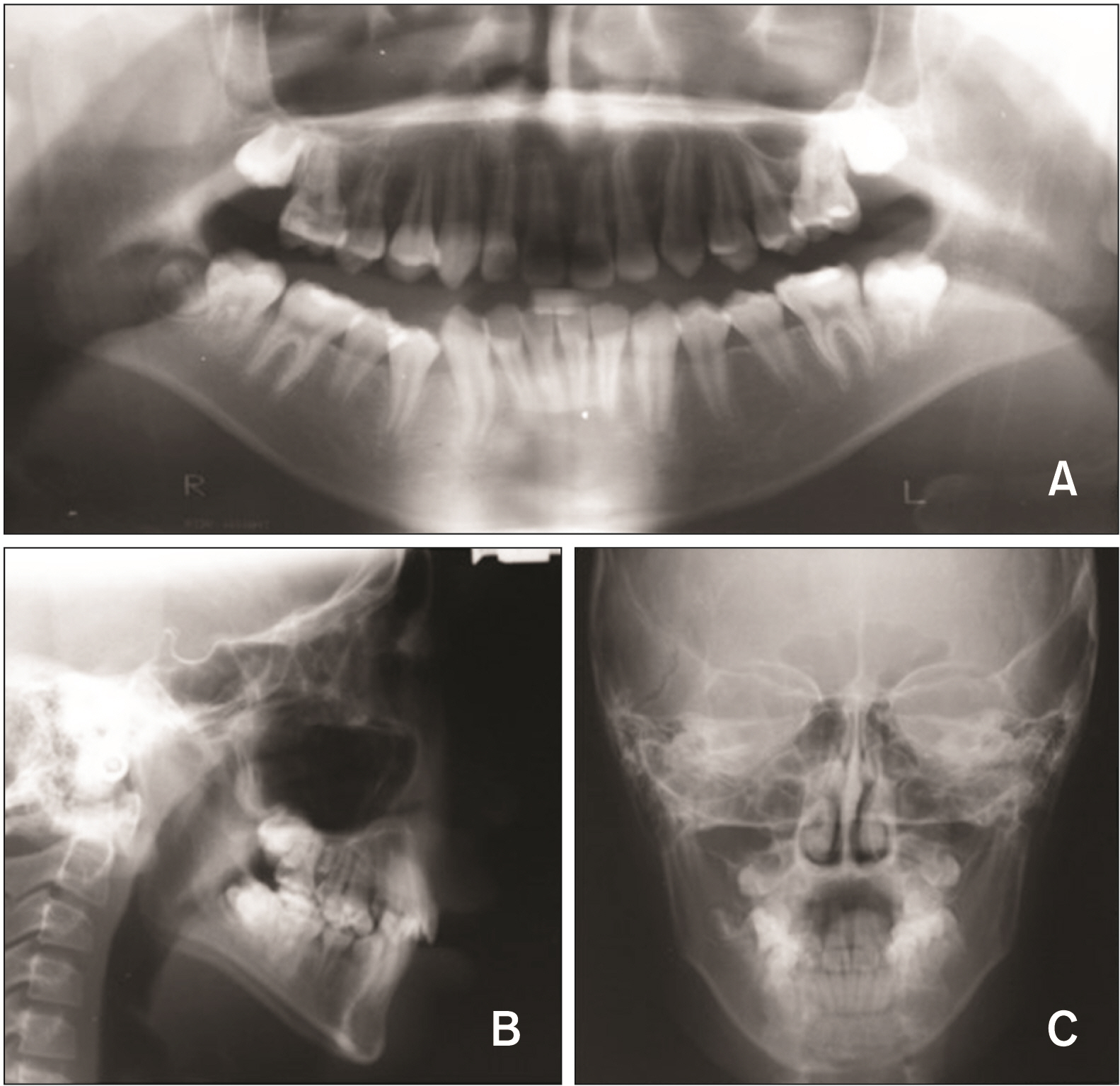
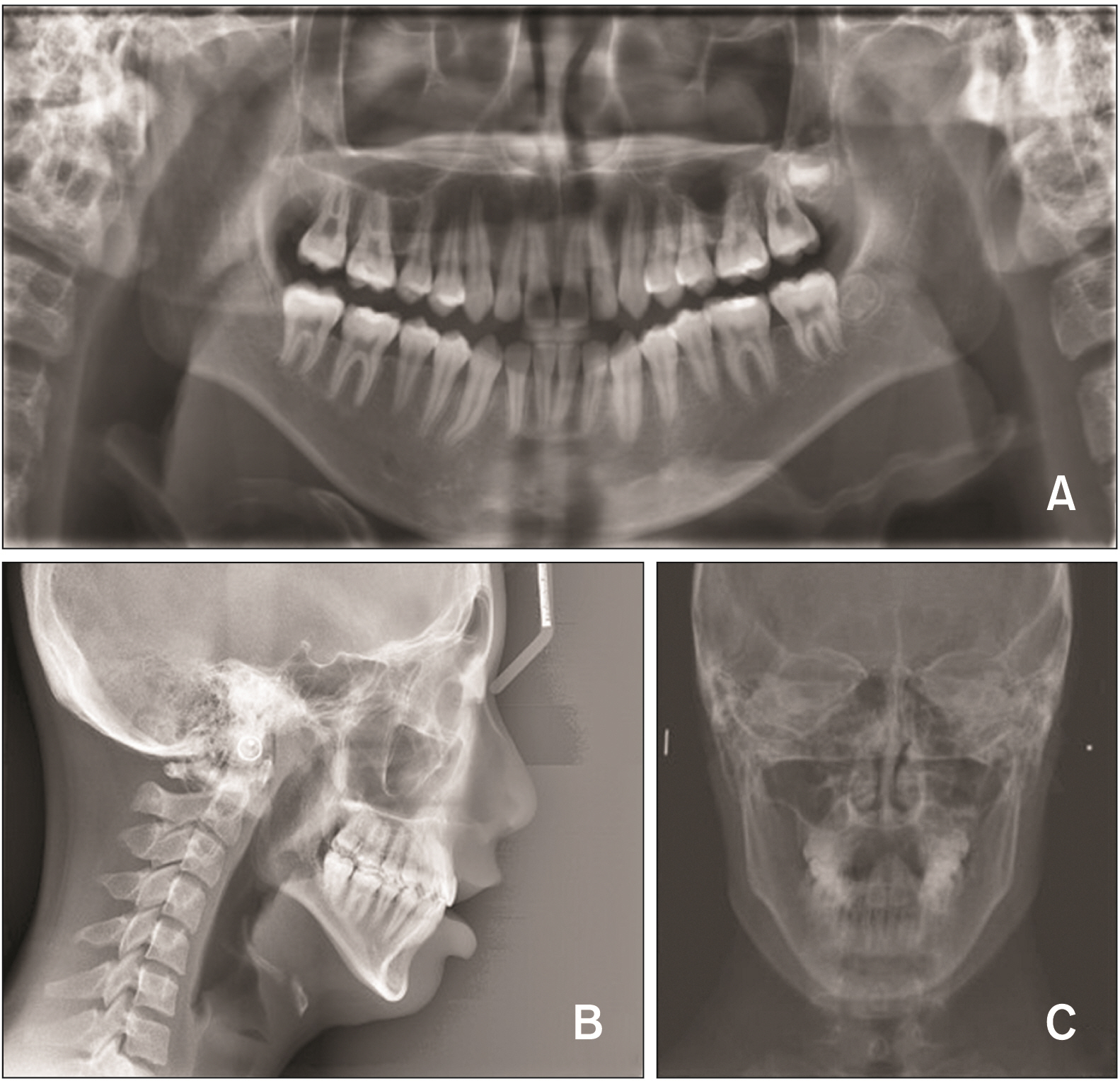
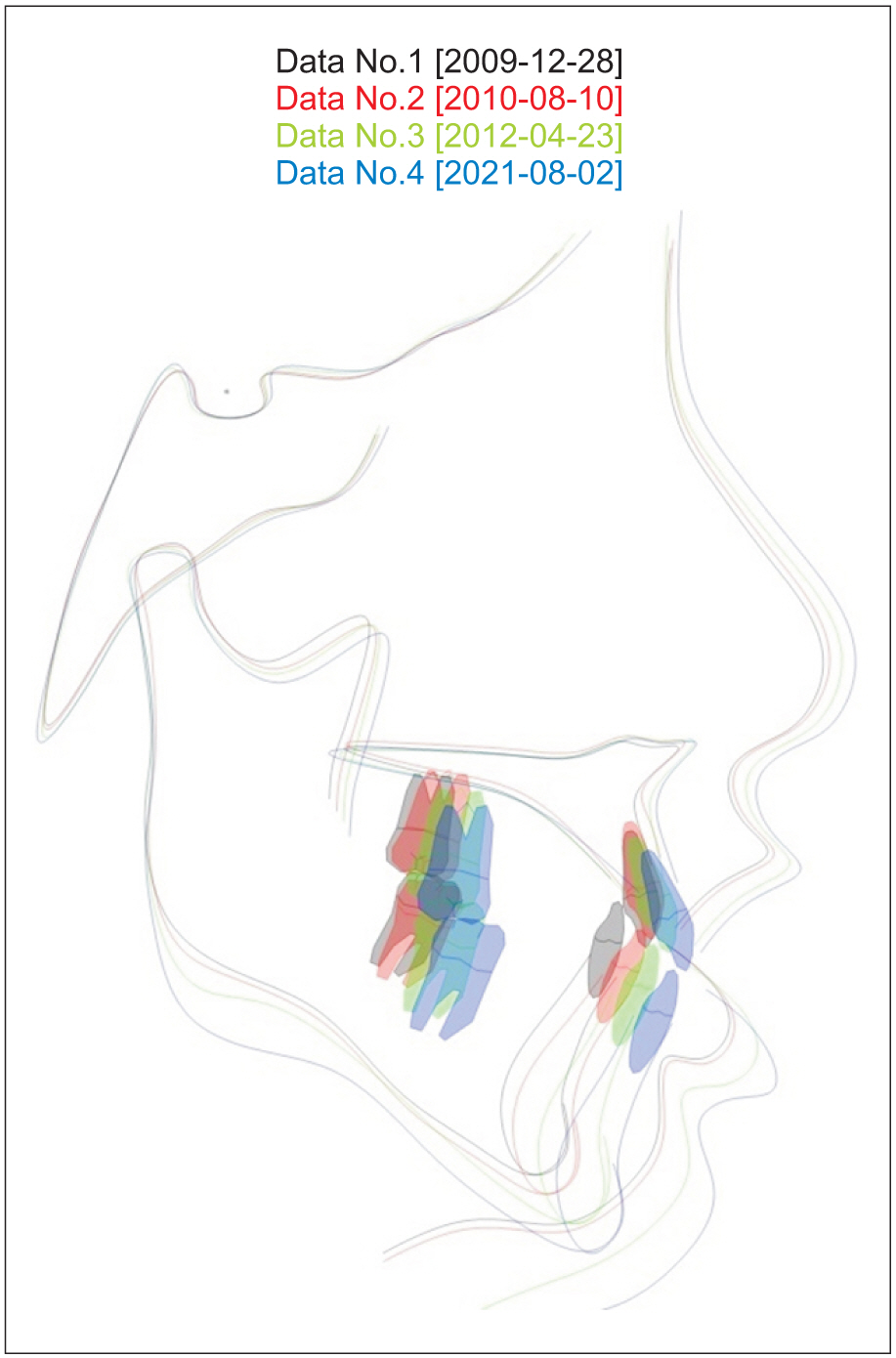
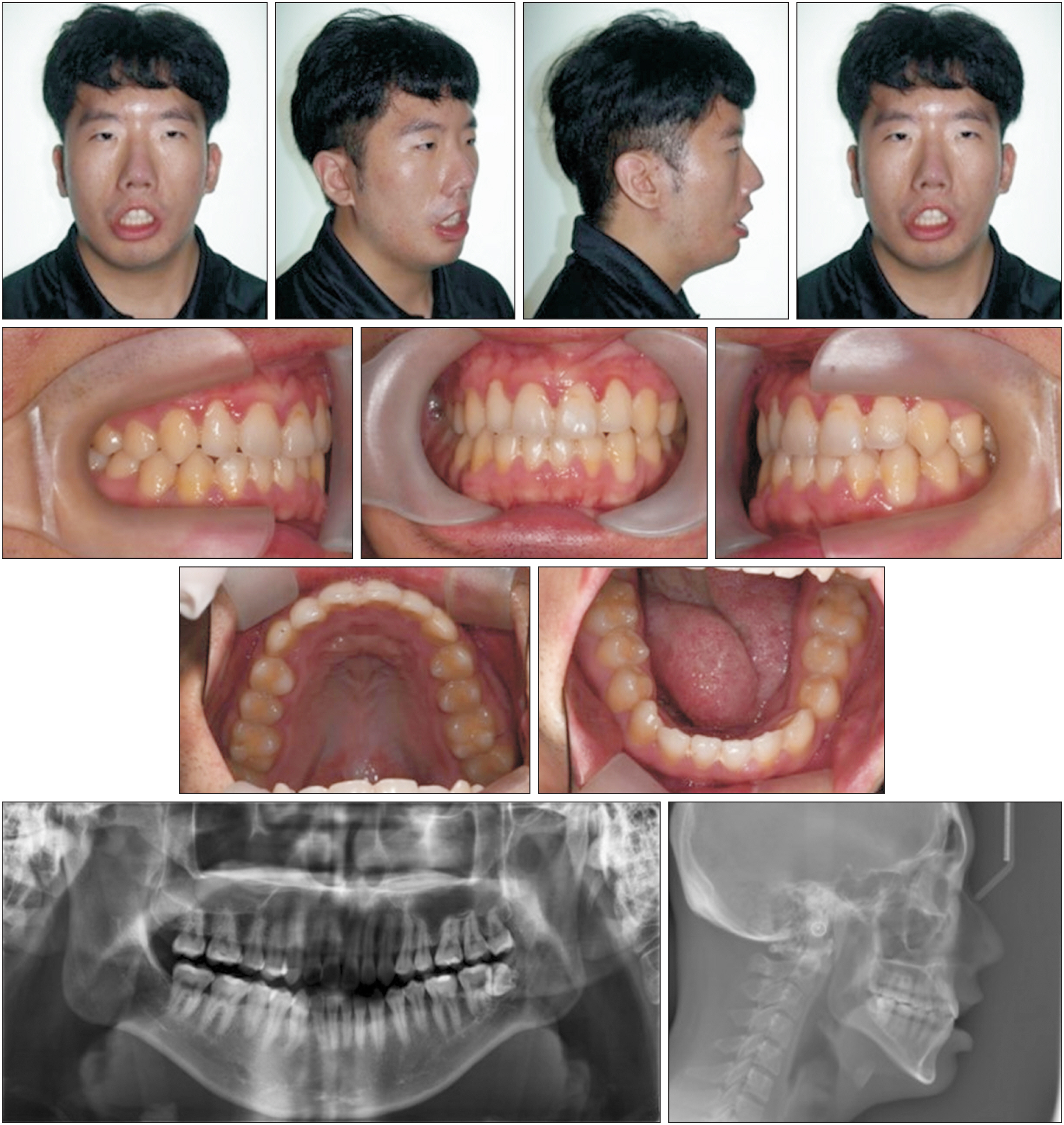
- Moebius syndrome (MBS) is a congenital neurologic disorder that causes cranio-facial abnormalities. It involves paralysis of the VI and VII cranial nerves and causes bilateral or unilateral facial paralysis, eye movement disorder, and deformation of the upper and lower limbs. The orofacial dysfunctions include microstomia, micrognathia, hypotonic mimetic and lip muscles, dental enamel hypoplasia, tongue deformity, open bite or deep overbite, maxillary hypoplasia, high arched palate, mandibular hyperplasia or features indicating mandibular hypoplasia. This case report presents a 7-year-old male patient who was diagnosed with MBS at the age 2 years. The patient displayed typical clinical symptoms and was diagnosed with Class II malocclusion with a large overjet/ overbite, tongue deformity and motion limitation, and lip closure incompetency. Treatment was initiated using a removable appliance for left scissor bite correction. After permanent tooth eruption, fixed appliance treatment was performed for correction of the arch width discrepancy and deep overbite. A self-ligation system and wide-width arch form wire were used during the treatment to expand the arch width. After 30 months of phase II treatment, the alignment of the dental arch and stable molar occlusion was achieved. Function and occlusion remained stable with a Class I canine and molar relationship, and a normal overjet/overbite was maintained after 9.4 years of retainer use. In MBS patients, it is important to achieve an accurate early diagnosis, and implement a multidisciplinary treatment approach and long-term retention and follow-up.
Figure
Reference
-
1. Miller G. 2007; Neurological disorders. The mystery of the missing smile. Science. 316:826–7. DOI: 10.1126/science.316.5826.826. PMID: 17495152. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=34248587773&origin=inward.2. Möbius PJ. 2008; About congenital bilateral abducens and facialis palsy (1888). Strabismus. 16:39–44. DOI: 10.1080/09273970801946737. PMID: 18306122. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=39849105850&origin=inward.3. Verzijl HT, van der Zwaag B, Cruysberg JR, Padberg GW. 2003; Möbius syndrome redefined: a syndrome of rhombencephalic maldevelopment. Neurology. 61:327–33. DOI: 10.1212/01.WNL.0000076484.91275.CD. PMID: 12913192. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0042125052&origin=inward.4. Abramson DL, Cohen MM Jr, Mulliken JB. 1998; Möbius syndrome: classification and grading system. Plast Reconstr Surg. 102:961–7. DOI: 10.1097/00006534-199809020-00004. PMID: 9734409.5. Kumar D. 1990; Moebius syndrome. J Med Genet. 27:122–6. DOI: 10.1136/jmg.27.2.122. PMID: 2319579. PMCID: PMC1016933. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0025122294&origin=inward.6. Sjögreen L, Andersson-Norinder J, Jacobsson C. 2001; Development of speech, feeding, eating, and facial expression in Möbius sequence. Int J Pediatr Otorhinolaryngol. 60:197–204. DOI: 10.1016/S0165-5876(01)00532-8. PMID: 11551610. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=17944366918&origin=inward.7. Temtamy SA. 1985; The genetics of hand malformations. Cong Anom. 25:73–92. DOI: 10.1111/j.1741-4520.1985.tb00636.x. PMID: 215242. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0021915685&origin=inward.8. Gathwala G, Singh J, Dalal P, Garg A. 2011; Hypoglossia-hypodactyly syndrome in a newborn. J Craniomaxillofac Surg. 39:99–101. DOI: 10.1016/j.jcms.2010.06.007. PMID: 20673638. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=79952007507&origin=inward.9. Picciolini O, Porro M, Cattaneo E, Castelletti S, Masera G, Mosca F, et al. 2016; Moebius syndrome: clinical features, diagnosis, management and early intervention. Ital J Pediatr. 42:56. DOI: 10.1186/s13052-016-0256-5. PMID: 27260152. PMCID: PMC4893276. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84971665274&origin=inward.10. Rizos M, Negrón RJ, Serman N. 1998; Möbius syndrome with dental involvement: a case report and literature review. Cleft Palate Craniofac J. 35:262–8. DOI: 10.1597/1545-1569_1998_035_0262_mbswdi_2.3.co_2. PMID: 9603562.11. Guijarro-Martínez R, Hernández-Alfaro F. 2012; Management of maxillofacial hard and soft tissue discrepancy in Möbius sequence: clinical report and review of the literature. J Craniomaxillofac Surg. 40:11–6. DOI: 10.1016/j.jcms.2010.12.006. PMID: 21353788. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=83555172411&origin=inward.12. Gugino CF, Dus I. 1998; Unlocking orthodontic malocclusions: an interplay between form and function. Semin Orthod. 4:246–55. DOI: 10.1016/S1073-8746(98)80030-3. PMID: 10219180. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0032240941&origin=inward.13. Bianchi B, Ferri A, Brevi B, Di Blasio A, Copelli C, Di Blasio C, et al. 2013; Orthognathic surgery for the complete rehabilitation of Moebius patients: principles, timing and our experience. J Craniomaxillofac Surg. 41:e1–4. DOI: 10.1016/j.jcms.2012.07.002. PMID: 22878220. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84872007823&origin=inward.14. Magnifico M, Cassi D, Kasa I, Di Blasio M, Di Blasio A, Gandolfini M. 2017; Pre- and postsurgical orthodontics in patients with Moebius syndrome. Case Rep Dent. 2017:1484065. DOI: 10.1155/2017/1484065. PMID: 28409036. PMCID: PMC5376922. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85017179409&origin=inward.15. Cudzilo D, Matthews-Brzozowska T. 2019; Moebius syndrome: the challenge of dental management. Eur J Paediatr Dent. 20:143–6. DOI: 10.23804/ejpd.2019.20.02.12. PMID: 31246092. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85068866559&origin=inward.16. Magalhães M, Araújo L, Chiaradia C, Fraige A, Zamunaro M, Mantesso A. 2006; Early dental management of patients with Mobius syndrome. Oral Dis. 12:533–6. DOI: 10.1111/j.1601-0825.2006.01231.x. PMID: 17054764. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=33750327359&origin=inward.17. Bergersen EO. 1988; A longitudinal study of anterior vertical overbite from eight to twenty years of age. Angle Orthod. 58:237–56. DOI: 10.1043/0003-3219(1988)058<0237:ALSOAV>2.0.CO;2. PMID: 3189955.18. Sonnesen L, Svensson P. 2008; Temporomandibular disorders and psychological status in adult patients with a deep bite. Eur J Orthod. 30:621–9. DOI: 10.1093/ejo/cjn044. PMID: 18684706. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=60049086160&origin=inward.19. Pandis N, Polychronopoulou A, Eliades T. 2007; Self-ligating vs conventional brackets in the treatment of mandibular crowding: a prospective clinical trial of treatment duration and dental effects. Am J Orthod Dentofacial Orthop. 132:208–15. DOI: 10.1016/j.ajodo.2006.01.030. PMID: 17693371. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=34547666826&origin=inward.20. Woods MG. 2008; Sagittal mandibular changes with overbite correction in subjects with different mandibular growth directions: late mixed-dentition treatment effects. Am J Orthod Dentofacial Orthop. 133:388–94. DOI: 10.1016/j.ajodo.2006.03.037. PMID: 18331938. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=40449092421&origin=inward.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comprehensive Orthodontic Treatment in a Middle-Aged Patient with Missing Maxillary Left First Premolar: A Case Report
- Report on a case treated with lingual multibracket appliance
- An esthetic appliance for the management of crown-root fracture: a case report
- Orthodontic Traction of the Permanent Molar Using Skeletal Anchorage: A Case Report
- An orthodontic approach for Class III malocclusion in a pediatric cancer patient: A case report