Ann Surg Treat Res.
2022 Jun;102(6):295-305. 10.4174/astr.2022.102.6.295.
Surgical safety in the COVID-19 era: present and future considerations
- Affiliations
-
- 1Division of Colon and Rectal Surgery, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2530383
- DOI: http://doi.org/10.4174/astr.2022.102.6.295
Abstract
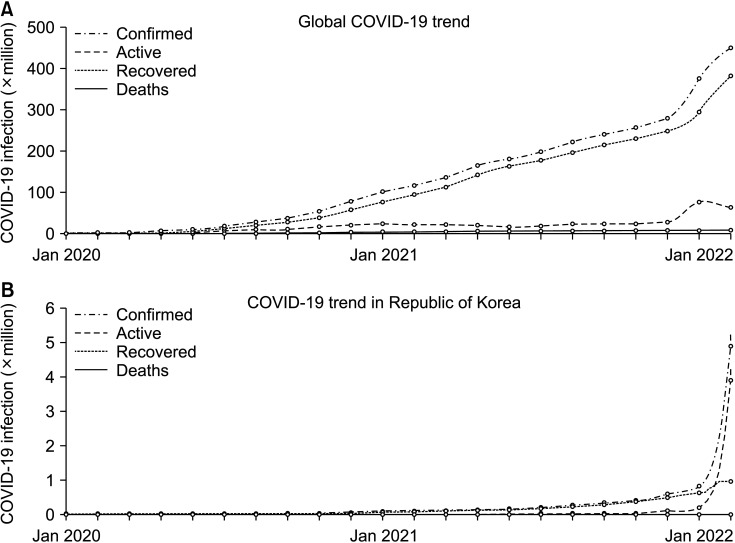
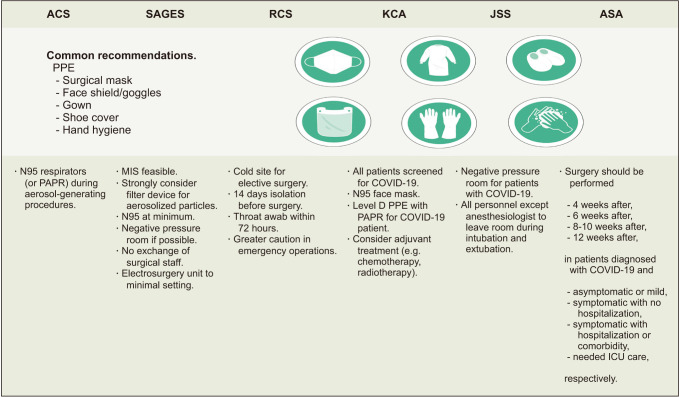
- The impacts of coronavirus disease 2019 (COVID-19) have been globally paradigm shifting in all aspects. Surgeons have experienced unprecedented changes regarding operation schedules, preparations before surgery, and the precautions needed both during and after surgery. Many medical centers simultaneously reported a decrease in their numbers of surgeries, whether they were elective or emergent, or for cancerous or benign resections. However, accumulated surgical outcomes from the last 2 years of experience presented postoperative morbidity and mortality data that were comparable to the pre-pandemic era, whether in elective or urgent settings. Although COVID-19 showed a significant association with postoperative morbidity and mortality, the majority of noninfected patients could be treated successfully with stringent mitigation protocols. Initially recommended to be avoided at the start of the pandemic, minimally invasive surgery seems to be safe and feasible according to reported surgical outcomes. Numerous sets of guidelines have now been produced from medical societies and adhering to the basic precautions has been found to be practicable. It is crucial that health care systems and surgical staff remain vigilant and attentive to the ever-changing situation in this pandemic in order to provide optimal medical support to their patients.
Keyword
Figure
Reference
-
1. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020; 382:727–733. PMID: 31978945.
Article2. Coronaviridae Study Group of the International Committee on Taxonomy of Viruses. The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020; 5:536–544. PMID: 32123347.3. World Health Organization (WHO). WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020 [Internet]. Geneva: WHO;2020. cited 2022 Apr 11. Available from: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.4. Johns Hopkins University & Medicine. COVID-19 dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU) [Internet]. Baltimore, MD: Johns Hopkins University & Medicine;c2022. cited 2022 Apr 11. Available from: https://coronavirus.jhu.edu/map.html.5. Berber E, Sumbria D, Çanakoğlu N. Meta-analysis and comprehensive study of coronavirus outbreaks: SARS, MERS and COVID-19. J Infect Public Health. 2021; 14:1051–1064. PMID: 34174535.
Article6. COVIDSurg Collaborative. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020; 107:1440–1449. PMID: 32395848.7. Dobbs TD, Gibson JA, Fowler AJ, Abbott TE, Shahid T, Torabi F, et al. Surgical activity in England and Wales during the COVID-19 pandemic: a nationwide observational cohort study. Br J Anaesth. 2021; 127:196–204. PMID: 34148732.
Article8. Choi JY, Park IJ, Lee HG, Cho E, Kim YI, Kim CW, et al. Impact of the COVID-19 pandemic on surgical treatment patterns for colorectal cancer in a tertiary medical facility in Korea. Cancers (Basel). 2021; 13:2221. PMID: 34066390.
Article9. Prasad NK, Englum BR, Turner DJ, Lake R, Siddiqui T, Mayorga-Carlin M, et al. A nation-wide review of elective surgery and COVID-surge capacity. J Surg Res. 2021; 267:211–216. PMID: 34157490.
Article10. Chang EI, Liu JJ. Flattening the curve in oncologic surgery: impact of COVID-19 on surgery at tertiary care cancer center. J Surg Oncol. 2020; 06. 02. DOI: 10.1002/jso.26056. [Epub].
Article11. Mattingly AS, Rose L, Eddington HS, Trickey AW, Cullen MR, Morris AM, et al. Trends in US surgical procedures and health care system response to policies curtailing elective surgical operations during the COVID-19 pandemic. JAMA Netw Open. 2021; 4:e2138038. PMID: 34878546.
Article12. Meredith JW, High KP, Freischlag JA. Preserving elective surgeries in the COVID-19 pandemic and the future. JAMA. 2020; 324:1725–1726. PMID: 33031523.
Article13. Sá AF, Lourenço SF, Teixeira RD, Barros F, Costa A, Lemos P. Urgent/emergency surgery during COVID-19 state of emergency in Portugal: a retrospective and observational study. Braz J Anesthesiol. 2021; 71:123–128. PMID: 33623174.
Article14. Hübner M, Zingg T, Martin D, Eckert P, Demartines N. Surgery for non-COVID-19 patients during the pandemic. PLoS One. 2020; 15:e0241331. PMID: 33095834.
Article15. Tebala GD, Milani MS, Bignell M, Bond-Smith G, Lewis C, Cirocchi R, et al. Emergency surgery admissions and the COVID-19 pandemic: did the first wave really change our practice?: results of an ACOI/WSES international retrospective cohort audit on 6263 patients. World J Emerg Surg. 2022; 17:8. PMID: 35090519.16. Cano-Valderrama O, Morales X, Ferrigni CJ, Martín-Antona E, Turrado V, García A, et al. Acute care surgery during the COVID-19 pandemic in Spain: changes in volume, causes and complications: a multicentre retrospective cohort study. Int J Surg. 2020; 80:157–161. PMID: 32679205.
Article17. Challine A, Dousset B, de’Angelis N, Lefèvre JH, Parc Y, Katsahian S, et al. Impact of coronavirus disease 2019 (COVID-19) lockdown on in-hospital mortality and surgical activity in elective digestive resections: a nationwide cohort analysis. Surgery. 2021; 170:1644–1649. PMID: 33597086.
Article18. Tschann P, Girotti PN, Lechner D, Adler S, Feurstein B, Szeverinski P, et al. How does the COVID-19 pandemic influence surgical case load and histological outcome for colorectal cancer?: a single-centre experience. J Gastrointest Surg. 2021; 25:2957–2960. PMID: 33852126.
Article19. Cui J, Li Z, An Q, Xiao G. Impact of the COVID-19 pandemic on elective surgery for colorectal cancer. J Gastrointest Cancer. 2021; 03. 17. DOI: 10.1007/s12029-021-00621-1. [Epub].
Article20. Fu SJ, George EL, Maggio PM, Hawn M, Nazerali R. The consequences of delaying elective surgery: surgical perspective. Ann Surg. 2020; 272:e79–e80. PMID: 32675504.
Article21. COVIDSurg Collaborative. Global guidance for surgical care during the COVID-19 pandemic. Br J Surg. 2020; 107:1097–1103. PMID: 32293715.22. Cai M, Wang G, Zhang L, Gao J, Xia Z, Zhang P, et al. Performing abdominal surgery during the COVID-19 epidemic in Wuhan, China: a single-centred, retrospective, observational study. Br J Surg. 2020; 107:e183–e185. PMID: 32339259.
Article23. Zhao N, Wu L, Cheng Y, Zheng H, Hu P, Hu C, et al. The effect of emergency surgery on acute abdomen patients with COVID-19 pneumonia: a retrospective observational study. Aging (Albany NY). 2020; 12:15771–15783. PMID: 32805726.
Article24. Seretis C, Archer L, Lalou L, Yahia S, Katz C, Parwaiz I, et al. Minimal impact of COVID-19 outbreak on the postoperative morbidity and mortality following emergency general surgery procedures: results from a 3-month observational period. Med Glas (Zenica). 2020; 17:275–278. PMID: 32662615.25. Bozkurt H, Gür HÜ, Akıncı M, Aslan H, Karakullukçu Ç, Yıldırım D. Evaluation of patients undergoing emergency surgery in a COVID-19 pandemic hospital: a cross-sectional study. Sao Paulo Med J. 2020; 138:305–309. PMID: 32638937.
Article26. Knisely A, Zhou ZN, Wu J, Huang Y, Holcomb K, Melamed A, et al. Perioperative morbidity and mortality of patients with COVID-19 who undergo urgent and emergent surgical procedures. Ann Surg. 2021; 273:34–40. PMID: 33074900.
Article27. COVIDSurg Collaborative. Outcomes from elective colorectal cancer surgery during the SARS-CoV-2 pandemic. Colorectal Dis. 2020; 11. 15. DOI: 10.1111/codi.15431. [Epub].28. Shrikhande SV, Pai PS, Bhandare MS, Bakshi G, Chaukar DA, Chaturvedi P, et al. Outcomes of elective major cancer surgery during COVID 19 at Tata Memorial Centre: implications for cancer care policy. Ann Surg. 2020; 272:e249–e252. PMID: 32520743.29. Kapoor D, Perwaiz A, Singh A, Chaudhary A. Elective gastrointestinal surgery in COVID times. Indian J Surg. 2020; 10. 22. DOI: 10.1007/s12262-020-02642-9. [Epub].30. Singhal R, Tahrani AA, Ludwig C, Mahawar K. GENEVA collaborators. Global 30-day outcomes after bariatric surgery during the COVID-19 pandemic (GENEVA): an international cohort study. Lancet Diabetes Endocrinol. 2021; 9:7–9. PMID: 33253631.31. Maggi U, De Carlis L, Yiu D, Colledan M, Regalia E, Rossi G, et al. The impact of the COVID-19 outbreak on liver transplantation programs in Northern Italy. Am J Transplant. 2020; 20:1840–1848. PMID: 32330351.
Article32. Varghese J, Malleeswaran S, Patcha RV, Appusamy E, Karnan P, Kapoor D, et al. A multicentric experience on living donor liver transplantation in coronavirus disease 2019 hotspots in India. Liver Transpl. 2021; 27:1334–1338. PMID: 33253477.
Article33. Li YX, He CZ, Liu YC, Zhao PY, Xu XL, Wang YF, et al. The impact of COVID-19 on gastric cancer surgery: a single-center retrospective study. BMC Surg. 2020; 20:222. PMID: 33008379.
Article34. Sparwasser P, Brandt MP, Haack M, Dotzauer R, Boehm K, Gheith MK, et al. Robotic surgery can be safely performed for patients and healthcare workers during COVID-19 pandemic. Int J Med Robot. 2021; 17:e2291. PMID: 34050598.
Article35. Glasbey JC, Nepogodiev D, Simoes JF, Omar O, Li E, Venn ML, et al. Elective cancer surgery in COVID-19-free surgical pathways dur ing the SARS-CoV-2 pandemic: an international, multicenter, comparative cohort study. J Clin Oncol. 2021; 39:66–78. PMID: 33021869.36. Deng JZ, Chan JS, Potter AL, Chen YW, Sandhu HS, Panda N, et al. The risk of postoperative complications after major elective surgery in active or resolved COVID-19 in the United States. Ann Surg. 2022; 275:242–246. PMID: 34793348.
Article37. Oh CK, Huh JW, Lee YJ, Choi MS, Pyo DH, Lee SC, et al. Long-term oncologic outcome of postoperative complications after colorectal cancer surgery. Ann Coloproctol. 2020; 36:273–280. PMID: 32054256.
Article38. Chaouch MA, Kellil T, Jeddi C, Saidani A, Chebbi F, Zouari K. How to prevent anastomotic leak in colorectal surgery?: a systematic review. Ann Coloproctol. 2020; 36:213–222. PMID: 32919437.
Article39. GlobalSurg Collaborative. COVIDSurg Collaborative. Timing of surgery following SARS-CoV-2 infection: an international prospective cohort study. Anaesthesia. 2021; 76:748–758. PMID: 33690889.40. Kovoor JG, Scott NA, Tivey DR, Babidge WJ, Scott DA, Beavis VS, et al. Proposed delay for safe surgery after COVID-19. ANZ J Surg. 2021; 91:495–506. PMID: 33656269.
Article41. Tebala GD, Mingoli A, Natili A, Khan AQ, Brachini G. Surgical risk and pathological results of emergency resection in the treatment of acutely obstructing colorectal cancers: a retrospective cohort study. Ann Coloproctol. 2021; 37:21–28. PMID: 32178504.
Article42. Grass F, Behm KT, Duchalais E, Crippa J, Spears GM, Harmsen WS, et al. Impact of delay to surgery on survival in stage I-III colon cancer. Eur J Surg Oncol. 2020; 46:455–461. PMID: 31806516.
Article43. Kaltenmeier C, Shen C, Medich DS, Geller DA, Bartlett DL, Tsung A, et al. Time to surgery and colon cancer survival in the United States. Ann Surg. 2021; 274:1025–1031. PMID: 31850985.
Article44. Shin DW, Cho J, Kim SY, Guallar E, Hwang SS, Cho B, et al. Delay to curative surgery greater than 12 weeks is associated with increased mortality in patients with colorectal and breast cancer but not lung or thyroid cancer. Ann Surg Oncol. 2013; 20:2468–2476. PMID: 23529782.
Article45. Whittaker TM, Abdelrazek ME, Fitzpatrick AJ, Froud JL, Kelly JR, Williamson JS, et al. Delay to elective colorectal cancer surgery and implications for survival: a systematic review and meta-analysis. Colorectal Dis. 2021; 23:1699–1711. PMID: 33714235.
Article46. Klein CA. Cancer progression and the invisible phase of metastatic colonization. Nat Rev Cancer. 2020; 20:681–694. PMID: 33024261.
Article47. Marchegiani G, Andrianello S, Perri G, Secchettin E, Maggino L, Malleo G, et al. Does the surgical waiting list affect pathological and survival outcome in resectable pancreatic ductal adenocarcinoma? HPB (Oxford). 2018; 20:411–417. PMID: 29191689.
Article48. Sanjeevi S, Ivanics T, Lundell L, Kartalis N, Andrén-Sandberg Å, Blomberg J, et al. Impact of delay between imaging and treatment in patients with potentially curable pancreatic cancer. Br J Surg. 2016; 103:267–275. PMID: 26572509.
Article49. American College of Surgeons (ACS). COVID-19: elective case triage guidelines for surgical care [Internet]. Chicago, IL: ACS;c1996-2022. cited 2022 Apr 11. Available from: https://www.facs.org/for-medical-professionals/covid-19/clinical-guidance/elective-case/.50. Society of Surgical Oncology (SSO). COVID-19 resources. Rosemont, IL: SOS;2020. cited 2022 Apr 11. Available from: https://www.surgonc.org/resources/covid-19-resources/.51. Manlubatan SI, Lopez MP, Onglao MA, Monroy Iii HJ. Modifications to treatment plan of rectal cancer in response to COVID-19 at the Philippine General Hospital. Ann Coloproctol. 2021; 37:225–231. PMID: 34364319.
Article52. Park SH, Shin JK, Lee WY, Yun SH, Cho YB, Huh JW, et al. Clinical outcomes of neoadjuvant chemotherapy in colorectal cancer patients with synchronous resectable liver metastasis: a propensity score matching analysis. Ann Coloproctol. 2021; 37:244–252. PMID: 34182620.
Article53. Park EJ. Shifting treatment strategies to prevent early relapse of locally advanced rectal cancer after preoperative chemoradiotherapy. Ann Coloproctol. 2020; 36:357–358. PMID: 33486905.
Article54. Liang W, Guan W, Chen R, Wang W, Li J, Xu K, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020; 21:335–337. PMID: 32066541.
Article55. Zhang L, Zhu F, Xie L, Wang C, Wang J, Chen R, et al. Clinical characteristics of COVID-19-infected cancer patients: a retrospective case study in three hospitals within Wuhan, China. Ann Oncol. 2020; 31:894–901. PMID: 32224151.
Article56. Lee JB, Jung M, Kim JH, Kim BH, Kim Y, Kim YS, et al. Guidelines for cancer care during the COVID-19 pandemic in South Korea. Cancer Res Treat. 2021; 53:323–329. PMID: 33721486.
Article57. Rottoli M, Pellino G, Spinelli A, Flacco ME, Manzoli L, Morino M, et al. Impact of COVID-19 on the oncological outcomes of colorectal cancer surgery in northern Italy in 2019 and 2020: multicentre comparative cohort study. BJS Open. 2022; 6:zrab139. PMID: 35143629.58. Kuryba A, Boyle JM, Blake HA, Aggarwal A, van der Meulen J, Braun M, et al. Surgical treatment and outcomes of colorectal cancer patients during the COVID-19 pandemic: a national population-based study in England. Ann Surg Open. 2021; 2:e071. PMID: 34240077.
Article59. Ghosh S, Nevins EJ, Hicks GJ, Carney K, Emmett C, Mills SJ. Colorectal cancer care in the COVID-19 era: outcomes from a‘mixed site’ model. Ann R Coll Surg Engl. 2022; 104:261–268. PMID: 34846184.60. Meijer J, Elferink MA, van Hoeve JC, Buijsen J, van Erning F, Nagtegaal ID, et al. Impact of the COVID-19 pandemic on colorectal cancer care in the Netherlands: a population-based study. Clin Colorectal Cancer. 2022; 03. 03. DOI: 10.1016/j.clcc.2022.02.005. [Epub].
Article61. Lim JH, Lee WY, Yun SH, Kim HC, Cho YB, Huh JW, et al. Has the COVID-19 pandemic caused upshifting in colorectal cancer stage? Ann Coloproctol. 2021; 37:253–258. PMID: 34376026.
Article62. Kara H, Arikan AE, Dulgeroglu O, Tutar B, Tokat F, Uras C. Has the COVID-19 pandemic affected breast cancer stage and surgical volume? Front Surg. 2022; 9:811108. PMID: 35198597.
Article63. Romics L, Doughty J, Stallard S, Mansell J, Blackhall V, Lannigan A, et al. A prospective cohort study of the safety of breast cancer surgery during COVID-19 pandemic in the West of Scotland. Breast. 2021; 55:1–6. PMID: 33285400.
Article64. Monaghesh E, Hajizadeh A. The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health. 2020; 20:1193. PMID: 32738884.
Article65. Simcock R, Thomas TV, Estes C, Filippi AR, Katz MA, Pereira IJ, et al. COVID-19: global radiation oncology’s targeted response for pandemic preparedness. Clin Transl Radiat Oncol. 2020; 22:55–68. PMID: 32274425.
Article66. Kim YJ. The future medical science and colorectal surgeons. Ann Coloproctol. 2017; 33:207–209. PMID: 29354602.
Article67. Mowbray N, Ansell J, Warren N, Wall P, Torkington J. Is surgical smoke harmful to theater staff?: a systematic review. Surg Endosc. 2013; 27:3100–3107. PMID: 23605191.
Article68. The Royal College of Surgeons of Edinburgh. Intercollegiate general surgery guidance on COVID-19 update [Internet]. Edinburgh: The Royal College of Surgeons of Edinburgh;2020. cited 2022 Apr 11. Available from: https://www.rcsed.ac.uk/news-public-affairs/news/2020/march/intercollegiate-general-surgery-guidance-on-covid-19-update.69. Hadjittofi C, Seraj SS, Uddin A, Ali ZJ, Antonas PL, Fisher RJ, et al. Laparoscopic vs open surgery during the COVID-19 pandemic: what are the risks. Ann R Coll Surg Engl. 2021; 103:354–359. PMID: 33682443.
Article70. Kameyama H, Otani T, Yamazaki T, Iwaya A, Uehara H, Harada R, et al. Comparison of surgical smoke between open surgery and laparoscopic surgery for colorectal disease in the COVID-19 era. Surg Endosc. 2022; 36:1243–1250. PMID: 33616729.
Article71. Romero-Velez G, Pereira X, Zenilman A, Camacho D. SARS-Cov-2 was not found in the peritoneal fluid of an asymptomatic pat ient undergoing laparoscopic appendectomy. Surg Laparosc Endosc Percutan Tech. 2020; 30:e43–e45. PMID: 32694404.72. Bogani G, Ditto A, De Cecco L, Lopez S, Guerrisi R, Piccioni F, et al. Transmission of SARS-CoV-2 in surgical smoke during laparoscopy: a prospective, proof-of-concept study. J Minim Invasive Gynecol. 2021; 28:1519–1525. PMID: 33373728.
Article73. Collings AT, Jeyarajah DR, Hanna NM, Dort J, Tsuda S, Nepal P, et al. SAGES 2022 guidelines regarding the use of laparoscopy in the era of COVID-19. Surg Endosc. 2022; 36:2723–2733. PMID: 35237900.
Article74. Tan WJ, Foo FJ, Sivarajah SS, Li LH, Koh FH, Chew MH. Safe colorectal surgery in the COVID-19 era: a Singapore experience. Ann Coloproctol. 2020; 36:65–69. PMID: 32429009.
Article75. American College of Surgeons (ACS). COVID 19: considerations for optimum surgeon protection before, during, and after operation [Internet]. Chicago, IL: ACS;2020. updated 2020 Apr 1. cited 2020 Apr 5. Available from: https://www.facs.org/for-medical-professionals/covid-19/clinical-guidance/surgeon-protection/.76. Pryor A. SAGES and EAES recommendations regarding surgical response to COVID-19 crisis. Los Angeles, CA: Society of American Gastrointestinal and Endoscopic Surgeons (SAGES);c2022. released 2020 Mar 30. cited 2022 Apr 11. Available from: https://www.sages.org/recommendations-surgical-response-covid-19/.77. American Society of Anesthesiologist (ASA). ASA and APSF joint statement on elective surgery and anesthesia for patients after COVID-19 infection [Internet]. Schaumburg, IL: ASA;c2022. cited 2022 Apr 11. Available from: https://www.asahq.org/about-asa/newsroom/news-releases/2020/12/asa-and-apsf-joint-statement-on-elective-surgery-and-anesthesia-for-patients-after-covid-19-infection.78. Mori M, Ikeda N, Taketomi A, Asahi Y, Takesue Y, Orimo T, et al. COVID-19: clinical issues from the Japan Surgical Society. Surg Today. 2020; 50:794–808. PMID: 32651686.
Article79. World Health Organization (WHO). Infection prevention and control during health care when coronavirus disease (COVID-19) is suspected or confirmed. Interim guidance, 29 June 2020 [Internet]. Geneva: WHO;c2022. cited 2022 Apr 11. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-IPC-2021.1.80. Centers for Disease Control and Prevention (CDC). Duration of isolation and precautions for adults with COVID-19. Atlanta, GA: CDC;2020. cited 2022 Apr 11. Available from: https://stacks.cdc.gov/view/cdc/93433/cdc_93433_DS1.pdf?.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cardiovascular Imaging Asia in the Era of the COVID-19 Outbreak
- Proposal of the Autopsy Guideline for Infectious Diseases: Preparation for the Post-COVID-19 Era
- The Role of COVID-19 Vaccination for Patients With Atherosclerotic Cardiovascular Disease in the Upcoming Endemic Era
- Proposal of the Autopsy Guideline for Infectious Diseases: Preparation for the Post-COVID-19 Era (abridged translation)
- Cardiovascular Imaging in the Era of the COVID-19 Outbreak