J Liver Cancer.
2022 Mar;22(1):75-83. 10.17998/jlc.2022.03.04.
Multidisciplinary treatment with immune checkpoint inhibitors for advanced stage hepatocellular carcinoma
- Affiliations
-
- 1Division of Gastroenterology and Hepatology, Department of Internal Medicine, Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2The Catholic University Liver Research Center, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Department of Radiation Oncology, Eunpyeong St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 4Department of Radiology, Eunpyeong St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 5Department of Radiology, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2528300
- DOI: http://doi.org/10.17998/jlc.2022.03.04
Abstract
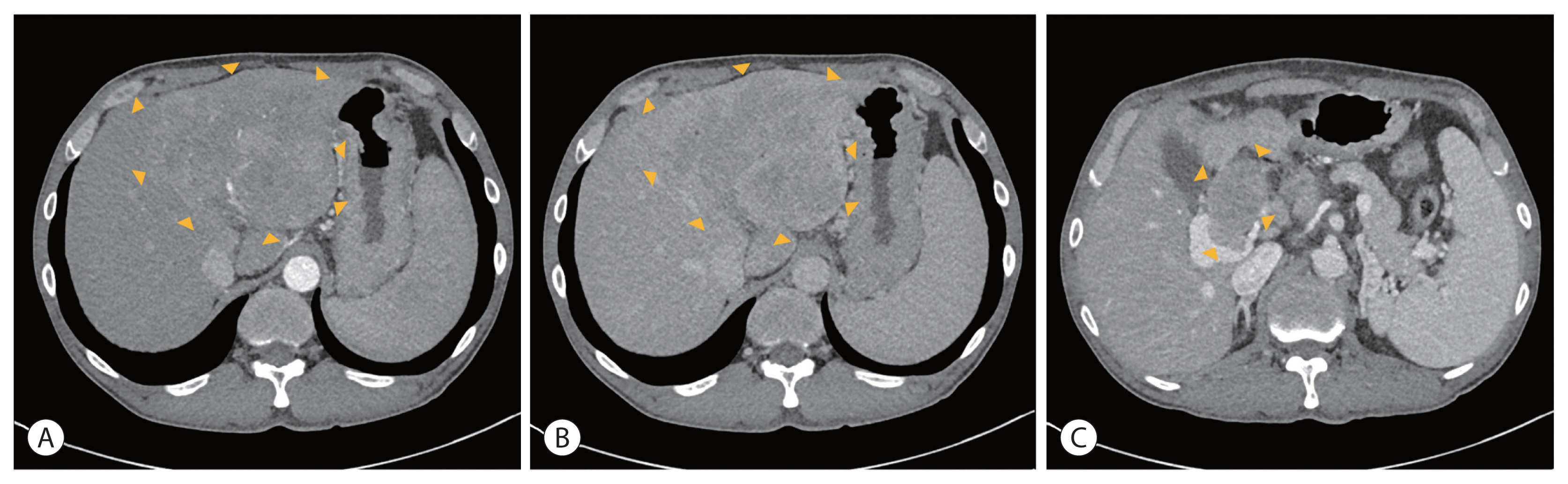
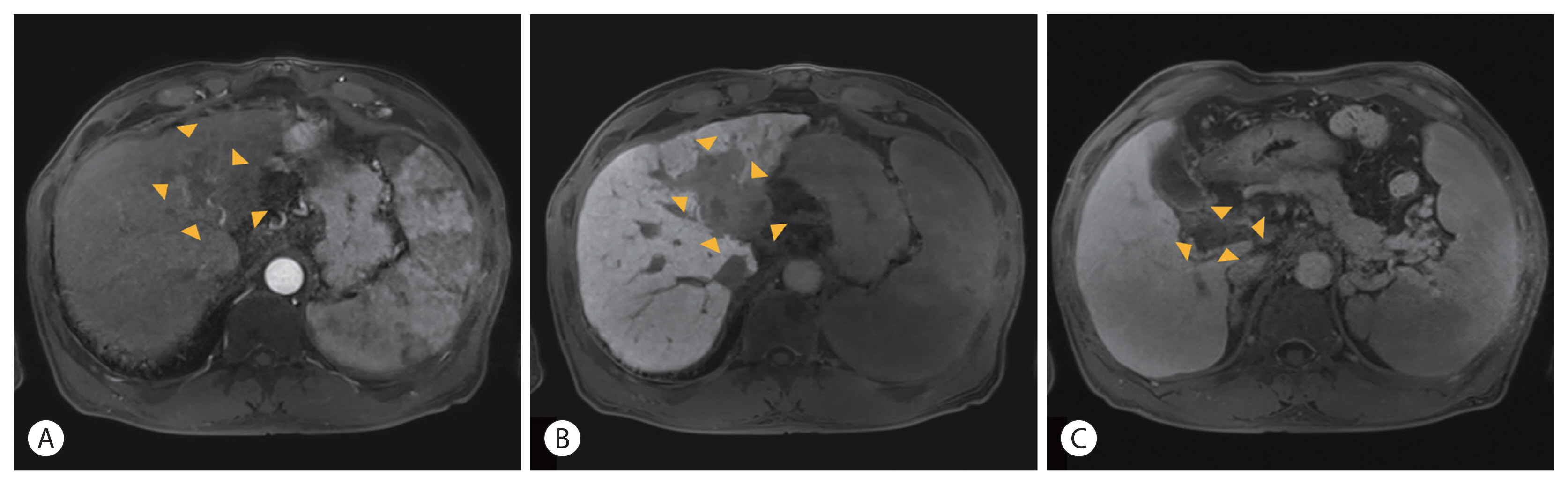
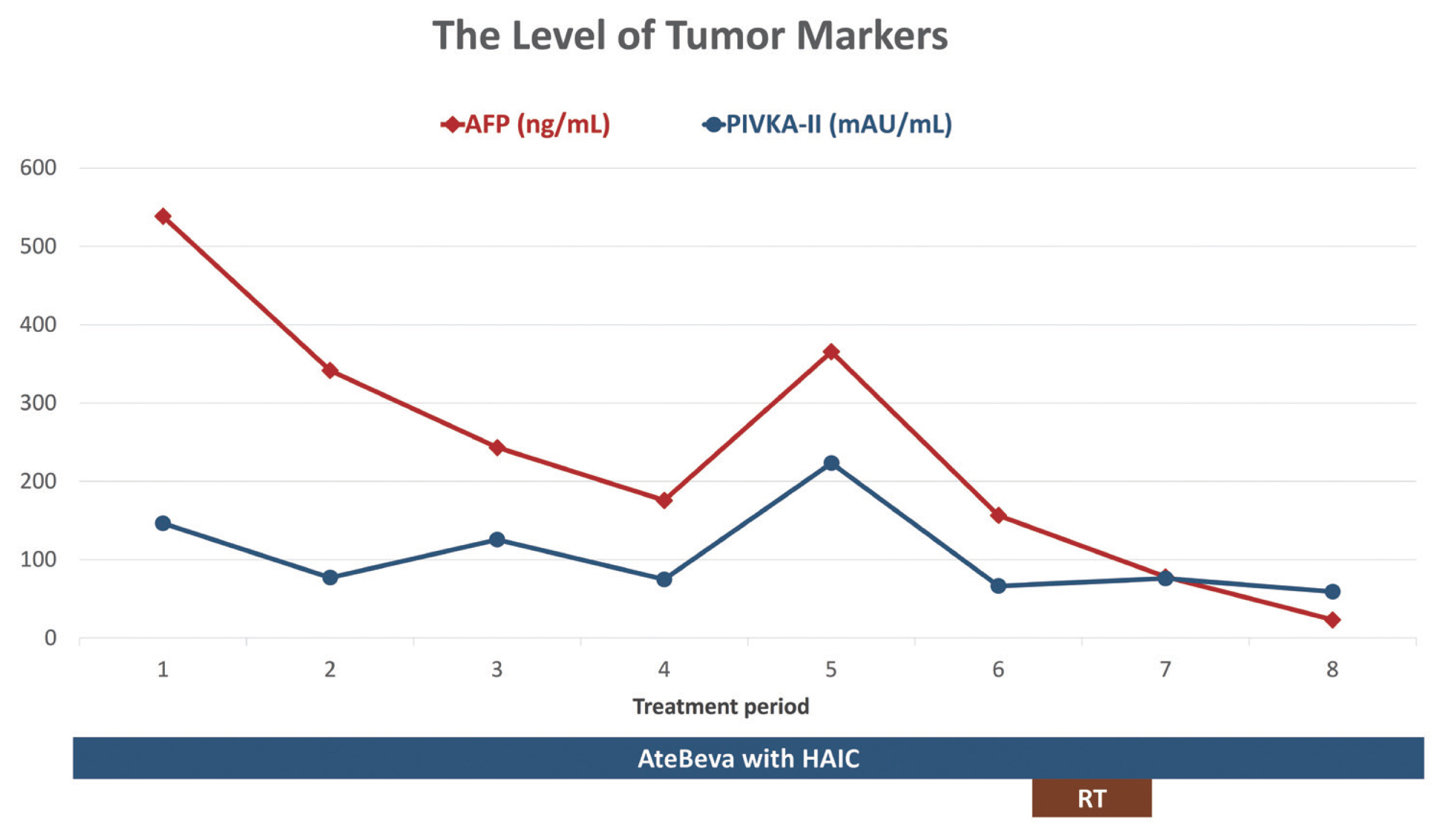
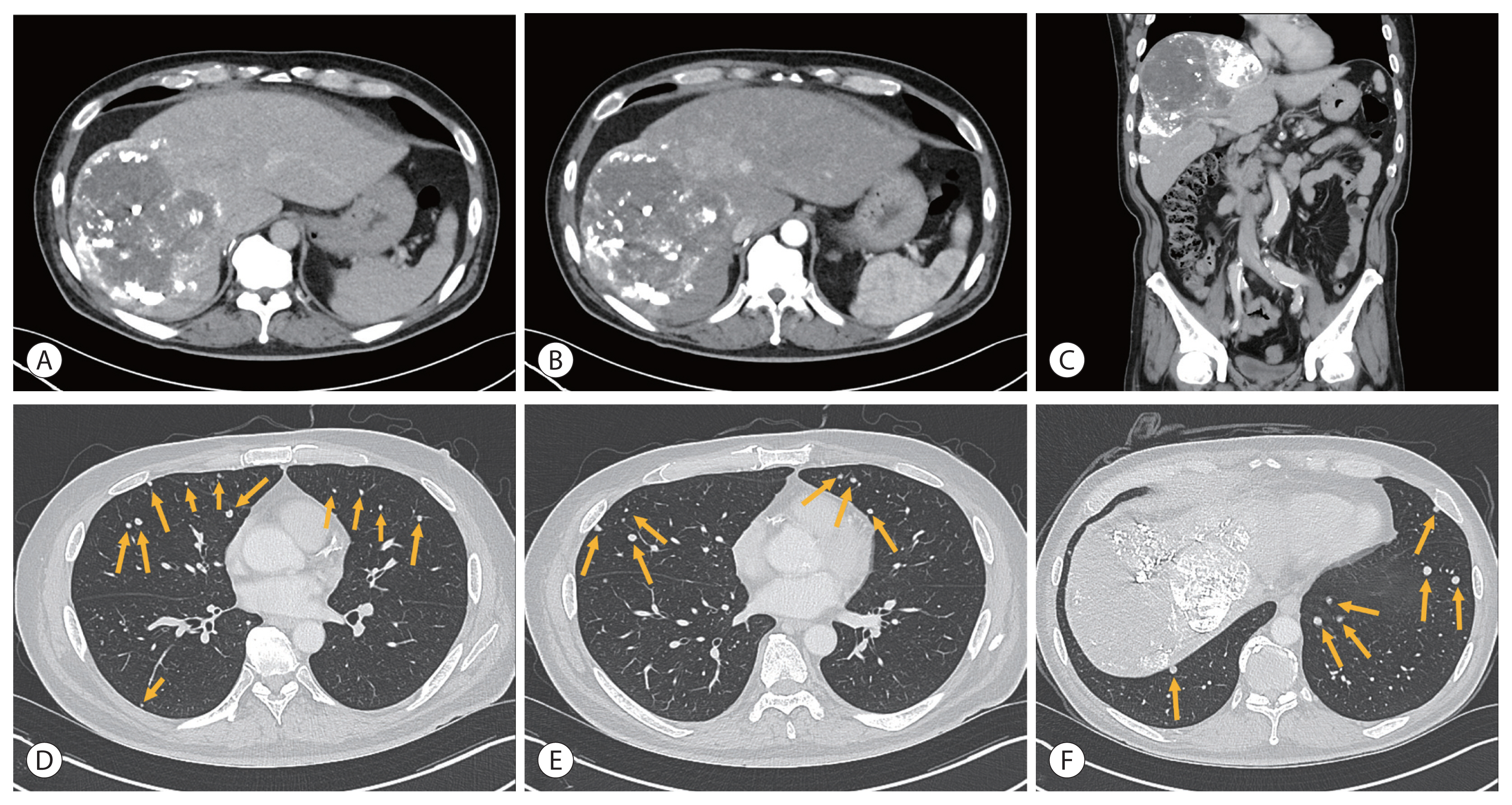
- Hepatocellular carcinoma (HCC) is a cytotoxic chemotherapy-resistant tumor and most HCCs arise in a background of liver cirrhosis of various causes. Although the IMBrave150 trial showed remarkable advancements in the treatment of unresectable HCC with atezolizumab plus bevacizumab (AteBeva), therapeutic outcomes were unsatisfactory in more than half of the patients. Accordingly, many ongoing trials combine conventional modalities with new drugs such as immune checkpoint inhibitors for better treatment outcomes, and they are expected to benefit patients with limited responses to conventional treatment. Here, two patients with advanced stage HCC with preserved liver function and good performance status showed partial response after treatment with combination or sequential therapy of AteBeva, hepatic arterial infusion chemotherapy, radiation therapy, and transarterial chemoembolization. These findings indicate the efficacy of multidisciplinary treatment against advanced HCC. Additional studies are required to establish optimal treatment strategies.
Keyword
Figure
Cited by 2 articles
-
Is multidisciplinary treatment effective for hepatocellular carcinoma with portal vein tumor thrombus?
Won Hyeok Choe
J Liver Cancer. 2022;22(1):1-3. doi: 10.17998/jlc.2022.03.15.Complications of immunotherapy in advanced hepatocellular carcinoma
Young-Gi Song, Jeong-Ju Yoo, Sang Gyune Kim, Young Seok Kim
J Liver Cancer. 2024;24(1):9-16. doi: 10.17998/jlc.2023.11.21.
Reference
-
References
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021; 71:209–249.
Article2. Liu PH, Huo TI, Miksad RA. Hepatocellular carcinoma with portal vein tumor involvement: best management strategies. Semin Liver Dis. 2018; 38:242–251.
Article3. Lurje I, Czigany Z, Bednarsch J, Roderburg C, Isfort P, Neumann UP, et al. Treatment strategies for hepatocellular carcinoma—a multidisciplinary approach. Int J Mol Sci. 2019; 20:1465.
Article4. Yang Z, Abdrakhimov B, Wang S, Xie QF, Zheng SS. Multidisciplinary treatment of advanced hepatocellular carcinoma. Case Rep Gastroenterol. 2020; 14:98–102.5. Pinter M, Jain RK, Duda DG. The current landscape of immune checkpoint blockade in hepatocellular carcinoma: a review. JAMA Oncol. 2021; 7:113–123.
Article6. Sung PS, Choi MH, Yang H, Lee SK, Chun HJ, Jang JW, et al. Diffusion-weighted magnetic resonance imaging in hepatocellular carcinoma as a predictor of a response to cisplatin-based hepatic arterial infusion chemotherapy. Front Oncol. 2020; 10:600233.
Article7. Cheng AL, Hsu C, Chan SL, Choo SP, Kudo M. Challenges of combination therapy with immune checkpoint inhibitors for hepatocellular carcinoma. J Hepatol. 2020; 72:307–319.
Article8. Doycheva I, Thuluvath PJ. Systemic therapy for advanced hepatocellular carcinoma: an update of a rapidly evolving field. J Clin Exp Hepatol. 2019; 9:588–596.
Article9. Lee YH, Tai D, Yip C, Choo SP, Chew V. Combinational immunotherapy for hepatocellular carcinoma: radiotherapy, immune checkpoint blockade and beyond. Front Immunol. 2020; 11:568759.
Article10. Liu BJ, Gao S, Zhu X, Guo JH, Kou FX, Liu SX, et al. Real-world study of hepatic artery infusion chemotherapy combined with anti-PD-1 immunotherapy and tyrosine kinase inhibitors for advanced hepatocellular carcinoma. Immunotherapy. 2021; 13:1395–1405.
Article11. Mei J, Li SH, Li QJ, Sun XQ, Lu LH, Lin WP, et al. Anti-PD-1 immunotherapy improves the efficacy of hepatic artery infusion chemotherapy in advanced hepatocellular carcinoma. J Hepatocell Carcinoma. 2021; 8:167–176.
Article12. Sung PS, Yang K, Bae SH, Oh JS, Chun HJ, Nam HC, et al. Reduction of intrahepatic tumour by hepatic arterial infusion chemotherapy prolongs survival in hepatocellular carcinoma. Anticancer Res. 2019; 39:3909–3916.
Article13. Lin CC, Hung CF, Chen WT, Lin SM. Hepatic arterial infusion chemotherapy for advanced hepatocellular carcinoma with portal vein thrombosis: impact of early response to 4 weeks of treatment. Liver Cancer. 2015; 4:228–240.
Article14. Korean Liver Cancer Association; National Cancer Center. 2018 Korean Liver Cancer Association-National Cancer Center Korea practice guidelines for the management of hepatocellular carcinoma. Gut Liver. 2019; 13:227–299.15. Reig M, Forner A, Rimola J, Ferrer-Fàbrega J, Burrel M, Garcia-Criado Á, et al. BCLC strategy for prognosis prediction and treatment recommendation: the 2022 update. J Hepatol. 2022; 76:681–693.
Article16. Jung SM, Jang JW, You CR, Yoo SH, Kwon JH, Bae SH, et al. Role of intrahepatic tumor control in the prognosis of patients with hepatocellular carcinoma and extrahepatic metastases. J Gastroenterol Hepatol. 2012; 27:684–689.
Article17. Uchino K, Tateishi R, Shiina S, Kanda M, Masuzaki R, Kondo Y, et al. Hepatocellular carcinoma with extrahepatic metastasis: clinical features and prognostic factors. Cancer. 2011; 117:4475–4483.
Article18. Gao S, Zhang PJ, Guo JH, Chen H, Xu HF, Liu P, et al. Chemoembolization alone vs combined chemoembolization and hepatic arterial infusion chemotherapy in inoperable hepatocellular carcinoma patients. World J Gastroenterol. 2015; 21:10443–10452.
Article19. Yoo C, Kim JH, Ryu MH, Park SR, Lee D, Kim KM, et al. Clinical outcomes with multikinase inhibitors after progression on first-line atezolizumab plus bevacizumab in patients with advanced hepatocellular carcinoma: a multinational multicenter retrospective study. Liver Cancer. 2021; 10:107–114.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A multidisciplinary approach with immunotherapies for advanced hepatocellular carcinoma
- Advances in immune checkpoint inhibitors for hepatocellular carcinoma
- Treatment of advanced urogenital cancers with immune checkpoint inhibitors
- Gastrointestinal cancer treatment with immune checkpoint inhibitors
- Infiltrative hepatocellular carcinoma with multiple lung metastasis completely cured using nivolumab: a case report