J Stroke.
2021 Sep;23(3):443-448. 10.5853/jos.2021.01312.
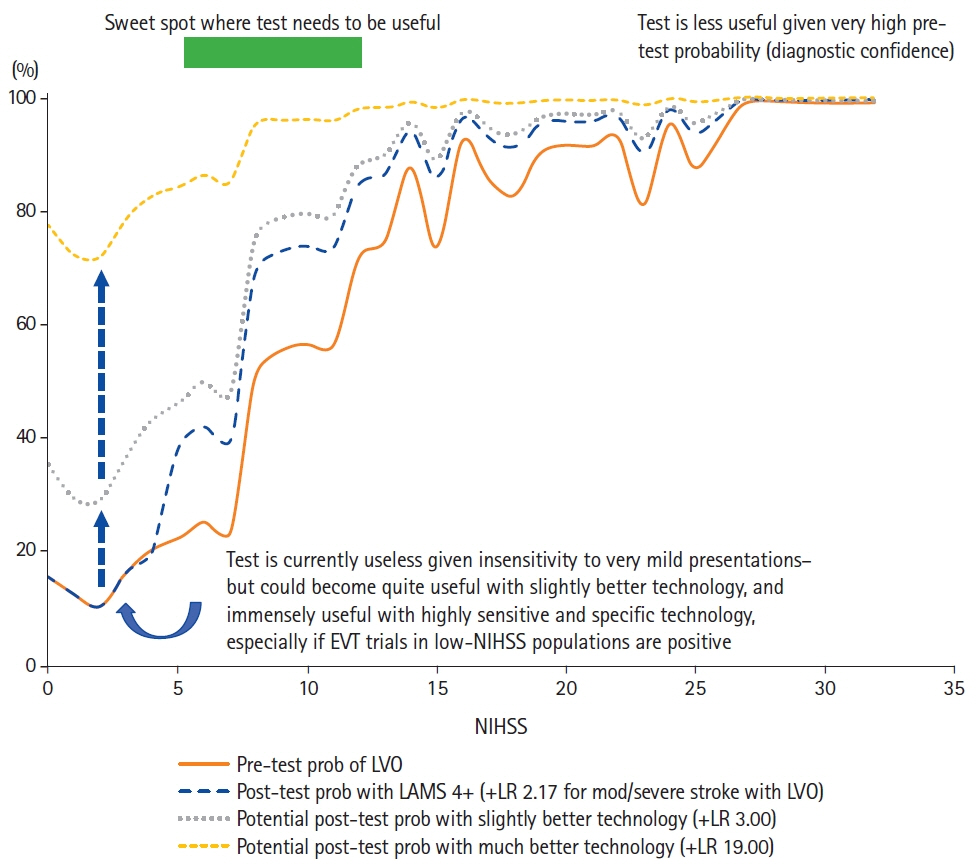
A Bayesian Framework to Optimize Performance of Pre-Hospital Stroke Triage Scales
- Affiliations
-
- 1Department of Radiology, University of Calgary Cumming School of Medicine, Calgary, AB, Canada
- 2Calgary Stroke Program, Department of Clinical Neurosciences, University of Calgary Cumming School of Medicine, Calgary, AB, Canada
- 3Hotchkiss Brain Institute, University of Calgary Cumming School of Medicine, Calgary, AB, Canada
- 4Department.of.Neuroradiology, University.Hospital.Basel,.Basel,.Switzerland…
- 5Cerebrovascular Center and Department of Neurology, Seoul National University Bundang Hospital, Seoul, Korea
- 6Departments of Neurology, Radiology, and Nuclear Medicine, Erasmus MC University Medical Center, Rotterdam, Netherlands
- 7Department of Neurology, Albert Schweitzer Hospital, Dordrecht, Netherlands
- KMID: 2520922
- DOI: http://doi.org/10.5853/jos.2021.01312
Figure
Reference
-
References
1. Saver JL, Goyal M, van der Lugt A, Menon BK, Majoie CB, Dippel DW, et al. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a metaanalysis. JAMA. 2016; 316:1279–1288.
Article2. Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet. 2014; 384:1929–1935.
Article3. Zhao H, Coote S, Pesavento L, Churilov L, Dewey HM, Davis SM, et al. Large vessel occlusion scales increase delivery to endovascular centers without excessive harm from misclassifications. Stroke. 2017; 48:568–573.
Article4. Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation. 2019; 139:e56–e528.5. Xirasagar S, Tsai MH, Heidari K, Hardin JW, Wu Y, Wronski R, et al. Why acute ischemic stroke patients in the United States use or do not use emergency medical services transport?: findings of an inpatient survey. BMC Health Serv Res. 2019; 19:929.
Article6. Adeoye O, Lindsell C, Broderick J, Alwell K, Jauch E, Moomaw CJ, et al. Emergency medical services use by stroke patients: a population-based study. Am J Emerg Med. 2009; 27:141–145.
Article7. Ganesh A, Luengo-Fernandez R, Wharton RM, Gutnikov SA, Silver LE, Mehta Z, et al. Time course of evolution of disability and cause-specific mortality after ischemic stroke: implications for trial design. J Am Heart Assoc. 2017; 6:e005788.
Article8. Reeves M, Khoury J, Alwell K, Moomaw C, Flaherty M, Woo D, et al. Distribution of National Institutes of Health stroke scale in the Cincinnati/Northern Kentucky Stroke Study. Stroke. 2013; 44:3211–3213.
Article9. Brown DL, Lisabeth LD, Garcia NM, Smith MA, Morgenstern LB. Emergency department evaluation of ischemic stroke and TIA: the BASIC Project. Neurology. 2004; 63:2250–2254.10. Wolters FJ, Paul NL, Li L, Rothwell PM; Oxford Vascular Study. Sustained impact of UK FAST-test public education on response to stroke: a population-based time-series study. Int J Stroke. 2015; 10:1108–1114.
Article11. Heldner MR, Zubler C, Mattle HP, Schroth G, Weck A, Mono ML, et al. National Institutes of Health stroke scale score and vessel occlusion in 2152 patients with acute ischemic stroke. Stroke. 2013; 44:1153–1157.
Article12. Nguyen TT, van den Wijngaard IR, Bosch J, van Belle E, van Zwet EW, Dofferhoff-Vermeulen T, et al. Comparison of prehospital scales for predicting large anterior vessel occlusion in the ambulance setting. JAMA Neurol. 2021; 78:157–164.
Article13. Smith EE, Kent DM, Bulsara KR, Leung LY, Lichtman JH, Reeves MJ, et al. Accuracy of prediction instruments for diagnosing large vessel occlusion in individuals with suspected stroke: a systematic review for the 2018 guidelines for the early management of patients with acute ischemic stroke. Stroke. 2018; 49:e111–e122.
Article14. Vidale S, Agostoni E. Prehospital stroke scales and large vessel occlusion: a systematic review. Acta Neurol Scand. 2018; 138:24–31.
Article15. Antipova D, Eadie L, Macaden A, Wilson P. Diagnostic accuracy of clinical tools for assessment of acute stroke: a systematic review. BMC Emerg Med. 2019; 19:49.
Article16. Mazya MV, Berglund A, Ahmed N, von Euler M, Holmin S, Laska AC, et al. Implementation of a prehospital stroke triage system using symptom severity and teleconsultation in the Stockholm Stroke Triage Study. JAMA Neurol. 2020; 77:691–699.
Article17. Duvekot MH, Venema E, Rozeman AD, Moudrous W, Vermeij FH, Biekart M, et al. Comparison of eight prehospital stroke scales to detect intracranial large-vessel occlusion in suspected stroke (PRESTO): a prospective observational study. Lancet Neurol. 2021; 20:213–221.18. Noorian AR, Sanossian N, Shkirkova K, Liebeskind DS, Eckstein M, Stratton SJ, et al. Los Angeles Motor Scale to identify large vessel occlusion: prehospital validation and comparison with other screens. Stroke. 2018; 49:565–572.19. Holodinsky JK, Williamson TS, Demchuk AM, Zhao H, Zhu L, Francis MJ, et al. Modeling stroke patient transport for all patients with suspected large-vessel occlusion. JAMA Neurol. 2018; 75:1477–1486.
Article20. Venema E, Lingsma HF, Chalos V, Mulder MJ, Lahr MM, van der Lugt A, et al. Personalized prehospital triage in acute ischemic stroke. Stroke. 2019; 50:313–320.
Article21. Matsuo R, Yamaguchi Y, Matsushita T, Hata J, Kiyuna F, Fukuda K, et al. Association between onset-to-door time and clinical outcomes after ischemic stroke. Stroke. 2017; 48:3049–3056.
Article22. Walsh KB. Non-invasive sensor technology for prehospital stroke diagnosis: current status and future directions. Int J Stroke. 2019; 14:592–602.
Article23. Sergot PB, Maza AJ, Derrick BJ, Smith LM, Berti LT, Wilcox MR, et al. Portable neuromonitoring device detects large vessel occlusion in suspected acute ischemic stroke. Stroke. 2021; 52:1437–1440.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of a Web-Based Korean Triage and Acuity Scale Learning Program on Triage Self-Efficacy and Triage Performance Ability for Nurses in Emergency Department
- A Nationwide Survey of Korean Emergency Department Triage Systems and Scales; A First Step Towards Reform of the Emergency Medical Service System
- Factors Influencing Triage Nurses' the Korean Triage and Acuity Scale Performance Ability
- Effects on Triage Competency Based on Nursing Task Performance and Self-Efficacy of Nurses in Regional Emergency Medical Institutions
- Clinical Assessment in Stroke Patients: Introduction of Neurologic Stroke Scales