J Korean Soc Matern Child Health.
2021 Jul;25(3):204-210. 10.21896/jksmch.2021.25.3.204.
Congenital Syphilis in Neonate: A Single Center Study for 10 Years
- Affiliations
-
- 1Department of Pediatrics, Pusan National University School of Medicine, Yangsan, Korea
- KMID: 2518924
- DOI: http://doi.org/10.21896/jksmch.2021.25.3.204
Abstract
- Purpose
Syphilis infections are becoming more prevalent in the Republic of Korea, and inadequately treated syphilis can lead to congenital syphilis (CS) in newborns. This study aimed to analyze the clinical manifestations of syphilis in mothers and newborns and to make suggestions to improve disease prognosis.
Methods
This single-center study was performed between August 2009 and August 2019 and included 29 newborns with CS. We retrospectively evaluated the clinical features, rapid plasma reagin (RPR) card test, fluorescent treponemal antibody absorption test (FTA-ABS), morbidity, and treatment regimen of all the syphilis-affected mothers and their newborns.
Results
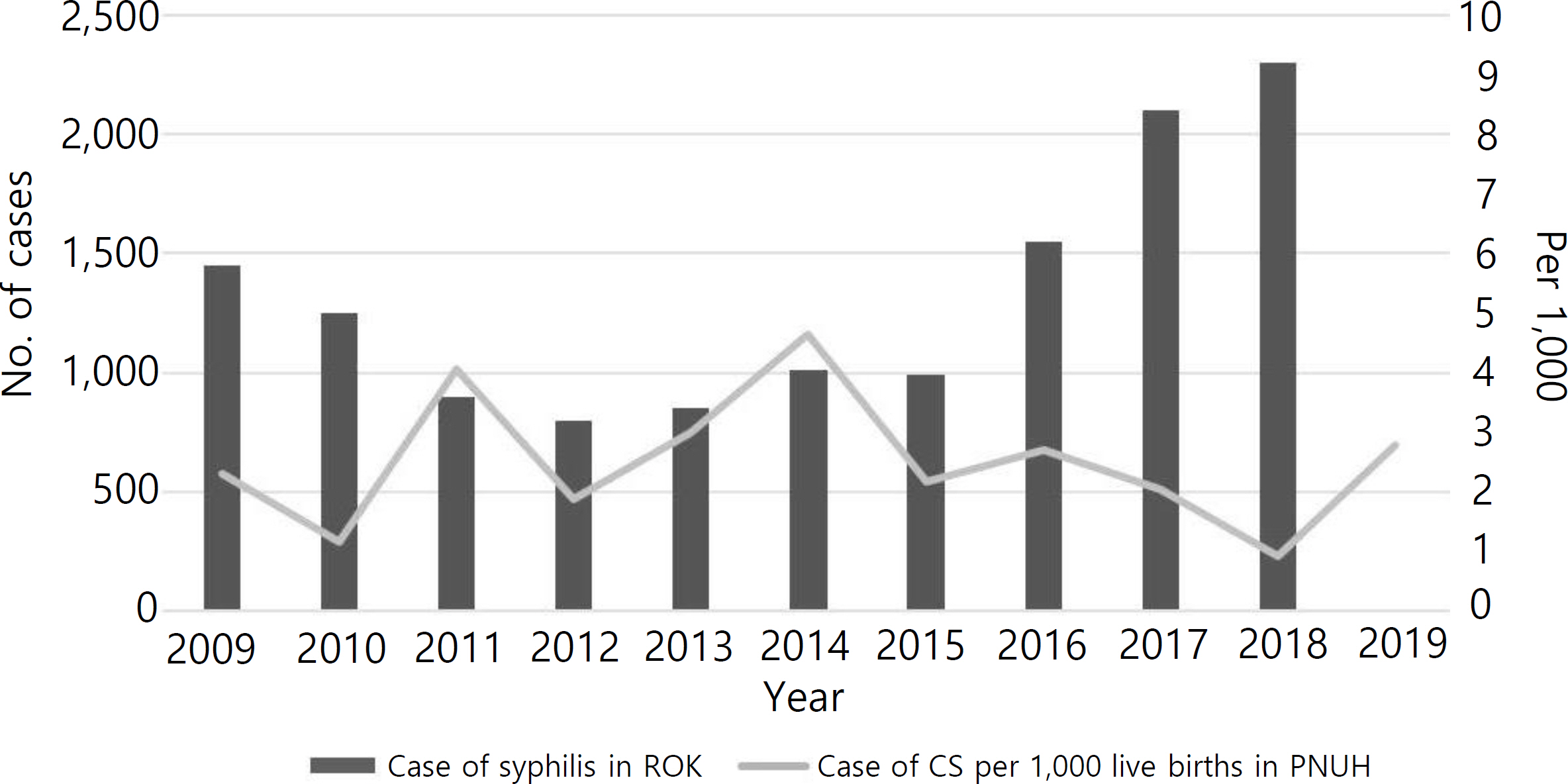
At the time of delivery, mean maternal age was 29.0±6.1 years old, and newborn gestational age was 38.0 weeks. In cases when syphilis was confirmed during the second and third trimesters of pregnancy, the newborn with CS had morbidity (p=0.004). The mean RPR titer was related to morbidity (p= 0.036). Positive results of FTA-ABS IgM (p<0.001) and pleocytosis in the cerebrospinal fluid (CSF) (p= 0.020) also increase morbidity. The most common symptoms were desquamation and skin rash, followed by hepatomegaly, neurodevelopmental disability, and bone abnormalities. The highest number of CS cases per 1,000 live births in this hospital was in 2014.
Conclusion
CS is a preventable and treatable disease if physicians detect symptoms and provide appropriate treatment through RPR examinations during every trimester. General practitioners should be widely trained on various aspects including early detection, formal treatment, and regular follow-up. Additionally, medical services should be provided for the entire childbearing population regardless of the socioeconomic status.
Figure
Reference
-
Arnold SR., Ford–Jones EL. Congenital syphilis: a guide to diagnosis and management. Paediatr Child Health. 2000. 5:463–9.
ArticleCenters for Disease Control and Prevention (CDC). Congenital syphilis – United States, 2003–2008. MMWR Morb Mortal Wkly Rep. 2010. 59:413–7.Cooper JM., Sánchez PJ. Congenital syphilis. Semin Perinatol. 2018. 42:176–84.
ArticleDivision of Tuberculosis and HIV/AIDS Prevention and Control. Management guidelines of sexually transmitted disease. Cheongju (Korea): Korea Centers for Disease Control and Prevention;2019.Kamb ML., Newman LM., Riley PL., Mark J., Hawkes SJ., Malik T, et al. A road map for the global elimination of congenital syphilis. Obstet Gynecol Int. 2010. 2010:312798.
ArticleKang SH., Lee JH., Choi SH., Lee J., Yoon HS., Cha SH, et al. Recent change in congenital syphilis in Korea: Retrospective 10 year study. Pediatr Int. 2015. 57:1112–5.Kim JK., Choi SR., Lee HJ., Kim DH., Yoon MS., Jo HS. Congenital syphilis presenting with a generalized bullous and pustular eruption in a premature newborn. Ann Dermatol. 2011. 23(Suppl 1):S127–30.
ArticleKimball A., Torrone E., Miele K., Bachmann L., Thorpe P., Weinstock H, et al. Missed opportunities for prevention of congenital syphilis – United States, 2018. MMWR Morb Mortal Wkly Rep. 2020. 69:661–5.
ArticleLago EG., Vaccari A., Fiori RM. Clinical features and follow–up of congenital syphilis. Sex Transm Dis. 2013. 40:85–94.
ArticleLim J., Yoon SJ., Shin JE., Han JH., Lee SM., Eun HS, et al. Outcomes of infants born to pregnant women with syphilis: a nationwide study in Korea. BMC Pediatr. 2021. 21:47.
ArticleOloya S., Lyczkowski D., Orikiriza P., Irama M., Boum Y., Migisha R, et al. Prevalence, associated factors and clinical features of congenital syphilis among newborns in Mbarara hospital, Uganda. BMC Pregnancy Childbirth. 2020. 20:385.
ArticlePark CY., Cho H. Prevention and management of perinatal major infectious diseases. J Korean Soc Matern Child Health. 2020. 24:133–43.
ArticlePlotzker RE., Murphy RD., Stoltey JE. Congenital syphilis prevention: strategies, evidence, and future directions. Sex Transm Dis. 2018. 45(9S Suppl 1):S29–37.
ArticleRac MW., Bryant SN., McIntire DD., Cantey JB., Twickler DM., Wendel GD Jr, et al. Progression of ultrasound findings of fetal syphilis after maternal treatment. Am J Obstet Gynecol. 2014. 211:426.e1–6.
ArticleRac MW., Revell PA., Eppes CS. Syphilis during pregnancy: a preventable threat to maternal–fetal health. Am J Obstet Gynecol. 2017. 216:352–63.
ArticleRadolf JD., Deka RK., Anand A., Šmajs D., Norgard MV., Yang XF. Treponema pallidum, the syphilis spirochete: making a living as a stealth pathogen. Nat Rev Microbiol. 2016. 14:744–59.
ArticleRothschild BM. History of syphilis. Clin Infect Dis. 2005. 40:1454–63.
ArticleRowe CR., Newberry DM., Jnah AJ. Congenital syphilis: a discussion of epidemiology, diagnosis, management, and nurses' role in early identification and treatment. Adv Neonatal Care. 2018. 18:438–45.Schmid G. Economic and programmatic aspects of congenital syphilis prevention. Bull World Health Organ. 2004. 82:402–9.Serafim AS., Moretti GP., Serafim GS., Niero CV., da Rosa MI., Pires MM, et al. Incidence of congenital syphilis in the South Region of Brazil. Rev Soc Bras Med Trop. 2014. 47:170–8.
ArticleWoods CR. Syphilis in children: congenital and acquired. Semin Pediatr Infect Dis. 2005. 16:245–57.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acquired Secondary Syphilis in Early Childhood
- Congenital Syphilis: Hematologic Findings of Early Congenital Syphilis
- Clinical Observation on 29 Cases of Congenital Syphilis
- A Case of Non-immune Hydrops Fetalis due to Congenital Syphilis
- Early congenital syphilis presenting with skin eruption alone: a case report