Clin Endosc.
2020 Nov;53(6):705-716. 10.5946/ce.2019.196.
Clinical Outcomes of Percutaneous Endoscopic Gastrostomy in the Surgical Intensive Care Unit
- Affiliations
-
- 1Department of Gastroenterology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Nutritional Support Team, Asan Medical Center, Seoul, Korea
- 3Division of Trauma and Surgical Critical Care, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2511230
- DOI: http://doi.org/10.5946/ce.2019.196
Abstract
- Background/Aims
Percutaneous endoscopic gastrostomy (PEG) is usually performed on patients with chronic underlying diseases in the general ward (GW). This study evaluated the clinical outcomes of PEG performed on patients in the surgical intensive care unit (SICU) compared with those of PEG performed in the GW.
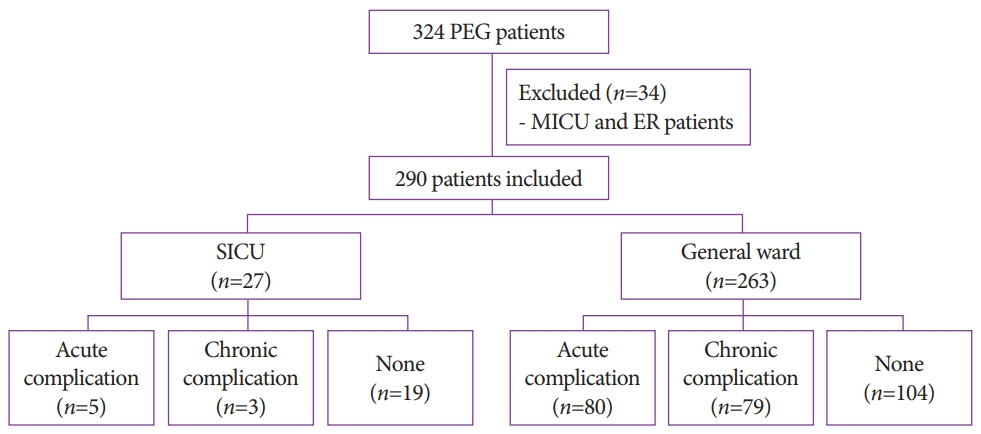
Methods
The medical records of 27 patients in the SICU and 263 in the GW, who underwent PEG between January 2013 and July 2017, were retrospectively reviewed.
Results
The median age of the 27 SICU patients was 66 years, and their median body mass index was 21.1 kg/m2. In the SICU group, the median baseline Sequential Organ Failure Assessment (SOFA) score was 4, and the median Acute Physiology and Chronic Health Evaluation II (APACHE II) score was 16. The median interval between surgery and PEG in SICU patients was 30 days, with a PEG failure rate of 3.7%. Acute complications in SICU patients included bleeding (7.4%) and ileus (11.1%), while chronic complications included aspiration pneumonia (7.4%) and tube obstruction (3.7%). The rates of acute and chronic complications did not differ significantly between the SICU and GW groups. The 30-day mortality rate was 14.8% in SICU patients and 5.3% in GW patients (p=0.073).
Conclusions
PEG is a safe and feasible method of enteral feeding for critically ill patients who require ICU care after surgery.
Keyword
Figure
Reference
-
1. Rahnemai-Azar AA, Rahnemaiazar AA, Naghshizadian R, Kurtz A, Farkas DT. Percutaneous endoscopic gastrostomy: indications, technique, complications and management. World J Gastroenterol. 2014; 20:7739–7751.
Article2. Löser C, Aschl G, Hébuterne X, et al. ESPEN guidelines on artificial enteral nutrition--percutaneous endoscopic gastrostomy (PEG). Clin Nutr. 2005; 24:848–861.3. Zippi M, Fiorani S, De Felici I, et al. Percutaneous endoscopic gastrostomy (PEG) in critically ill patients performed at bed in intensive care unit: report of our experience. Clin Ter. 2009; 160:359–362.4. Ferraro F, Gravina AG, d’Elia A, et al. Percutaneous endoscopic gastrostomy for critically ill patients in a general intensive care unit. Acta Gastroenterol Belg. 2013; 76:306–310.5. Koc D, Gercek A, Gencosmanoglu R, Tozun N. Percutaneous endoscopic gastrostomy in the neurosurgical intensive care unit: complications and outcome. JPEN J Parenter Enteral Nutr. 2007; 31:517–520.
Article6. Eleftheriadis E, Kotzampassi K. Percutaneous endoscopic gastrostomy after abdominal surgery. Surg Endosc. 2001; 15:213–216.
Article7. Guzzo JL, Bochicchio GV, Haan J, Bochicchio K, Kole K, Scalea TM. Percutaneous endoscopic gastrostomy in ICU patients with previous laparotomy. Am Surg. 2005; 71:420–423.
Article8. Pih GY, Na HK, Ahn JY, et al. Risk factors for complications and mortality of percutaneous endoscopic gastrostomy insertion. BMC Gastroenterol. 2018; 18:101.
Article9. Andersen HK, Lewis SJ, Thomas S. Early enteral nutrition within 24h of colorectal surgery versus later commencement of feeding for postoperative complications. Cochrane Database Syst Rev. 2006; (4):CD004080.
Article10. Herbert G, Perry R, Andersen HK, et al. Early enteral nutrition within 24 hours of lower gastrointestinal surgery versus later commencement for length of hospital stay and postoperative complications. Cochrane Database Syst Rev. 2019; 7:CD004080.
Article11. Lewis SJ, Andersen HK, Thomas S. Early enteral nutrition within 24 h of intestinal surgery versus later commencement of feeding: a systematic review and meta-analysis. J Gastrointest Surg. 2009; 13:569–575.12. Heyland DK. Nutritional support in the critically ill patients. A critical review of the evidence. Crit Care Clin. 1998; 14:423–440.13. Mazzola P, Bellelli G, Perego S, et al. The sequential organ failure assessment score predicts 30-day mortality in a geriatric acute care setting. J Gerontol A Biol Sci Med Sci. 2013; 68:1291–1295.
Article14. Safari S, Shojaee M, Rahmati F, et al. Accuracy of SOFA score in prediction of 30-day outcome of critically ill patients. Turk J Emerg Med. 2016; 16:146–150.
Article15. Jentzer JC, Bennett C, Wiley BM, et al. Predictive value of the sequential organ failure assessment score for mortality in a contemporary cardiac intensive care unitpopulation. J Am Heart Assoc. 2018; 7:e008169.
Article16. Grmec S, Gasparovic V. Comparison of APACHE II, MEES and Glasgow Coma Scale in patients with nontraumatic coma for prediction of mortality. Acute Physiology and Chronic Health Evaluation. Mainz Emergency Evaluation System. Crit Care. 2001; 5:19–23.17. Wang IK, Wang ST, Chang HY, et al. Prognostic value of acute physiology and chronic health evaluation II and organ system failure in patients with acute renal failure requiring dialysis. Ren Fail. 2005; 27:663–669.
Article18. Huang J, Xuan D, Li X, Ma L, Zhou Y, Zou H. The value of APACHE II in predicting mortality after paraquat poisoning in Chinese and Korean population: a systematic review and meta-analysis. Medicine (Baltimore). 2017; 96:e6838.19. To KB, Napolitano LM. Common complications in the critically ill patient. Surg Clin North Am. 2012; 92:1519–1557.
Article20. Sawyer RG, Leon CA. Common complications in the surgical intensive care unit. Crit Care Med. 2010; 38(9 Suppl):S483–S493.
Article21. Lockett MA, Templeton ML, Byrne TK, Norcross ED. Percutaneous endoscopic gastrostomy complications in a tertiary-care center. Am Surg. 2002; 68:117–120.22. Ahmad I, Mouncher A, Abdoolah A, et al. Antibiotic prophylaxis for percutaneous endoscopic gastrostomy--a prospective, randomised, double- blind trial. Aliment Pharmacol Ther. 2003; 18:209–215.23. Bragg D, El-Sharkawy AM, Psaltis E, Maxwell-Armstrong CA, Lobo DN. Postoperative ileus: recent developments in pathophysiology and management. Clin Nutr. 2015; 34:367–376.
Article24. Boelens PG, Heesakkers FF, Luyer MD, et al. Reduction of postoperative ileus by early enteral nutrition in patients undergoing major rectal surgery: prospective, randomized, controlled trial. Ann Surg. 2014; 259:649–655.25. Foutch PG, Talbert GA, Waring JP, Sanowski RA. Percutaneous endoscopic gastrostomy in patients with prior abdominal surgery: virtues of the safe tract. Am J Gastroenterol. 1988; 83:147–150.26. Townsend MC, Flancbaum L, Cloutier CT, Arnold MW. Early postlaparotomy percutaneous endoscopic gastrostomy. Surg Gynecol Obstet. 1992; 174:46–48.27. Stellato TA, Gauderer MW, Ponsky JL. Percutaneous endoscopic gastrostomy following previous abdominal surgery. Ann Surg. 1984; 200:46–50.
Article28. Yamazaki T, Sakai Y, Hatakeyama K, Hoshiyama Y. Colocutaneous fistula after percutaneous endoscopic gastrostomy in a remnant stomach. Surg Endosc. 1999; 13:280–282.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous Endoscopic Gastrostomy Through the Sinus Tract of a Surgical Gastrostomy
- Long Term Efficacy of Percutaneous Endoscopic Gastrostomy
- Updates on Percutaneous Radiologic Gastrostomy/Gastrojejunostomy and Jejunostomy
- A Case of Percutaneous Endoscopic Gastrostomy in a Patient with Liver Cirrhosis Accompanied by Both Esophageal and Gastric Varices
- A Case of Buried Bumper Syndrome; A case report