J Korean Assoc Oral Maxillofac Surg.
2020 Oct;46(5):321-327. 10.5125/jkaoms.2020.46.5.321.
An in vivo electromyographic evaluation of pain relief using different therapies in masticatory myalgia patients
- Affiliations
-
- 1Department of Prosthodontics, Nitte (Deemed to be University), AB Shetty Memorial Institute of Dental Sciences (ABSMIDS), Mangalore, India
- 2Nitte Institute of Physiotherapy (NIPT), Nitte (Deemed to be University), Mangalore, India
- KMID: 2508256
- DOI: http://doi.org/10.5125/jkaoms.2020.46.5.321
Abstract
Objectives
This study is aimed to evaluate and compare the effect of moist heat fomentation therapy with ultrasound therapy in patients with the masticatory myalgia.
Materials and Methods
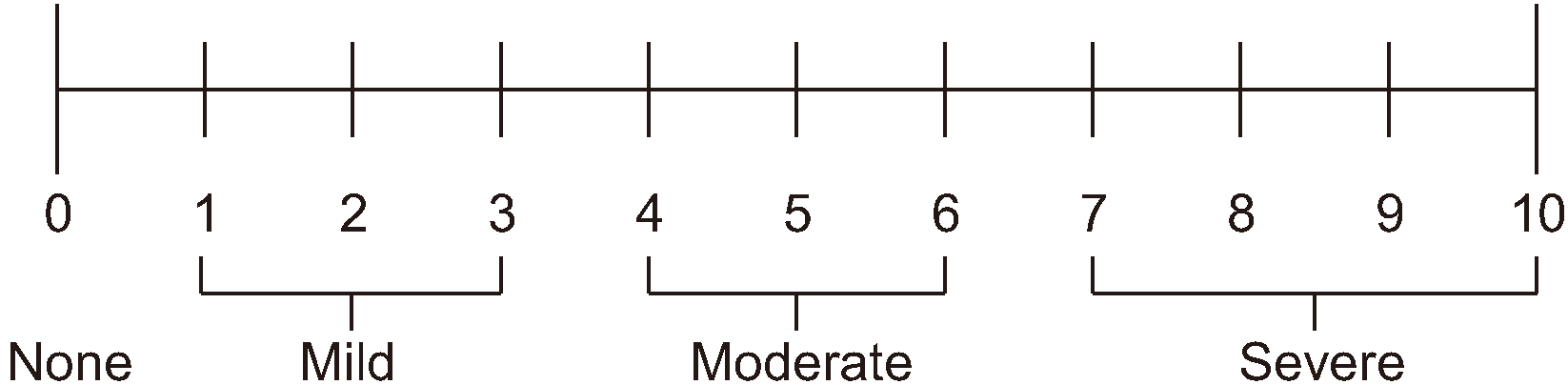
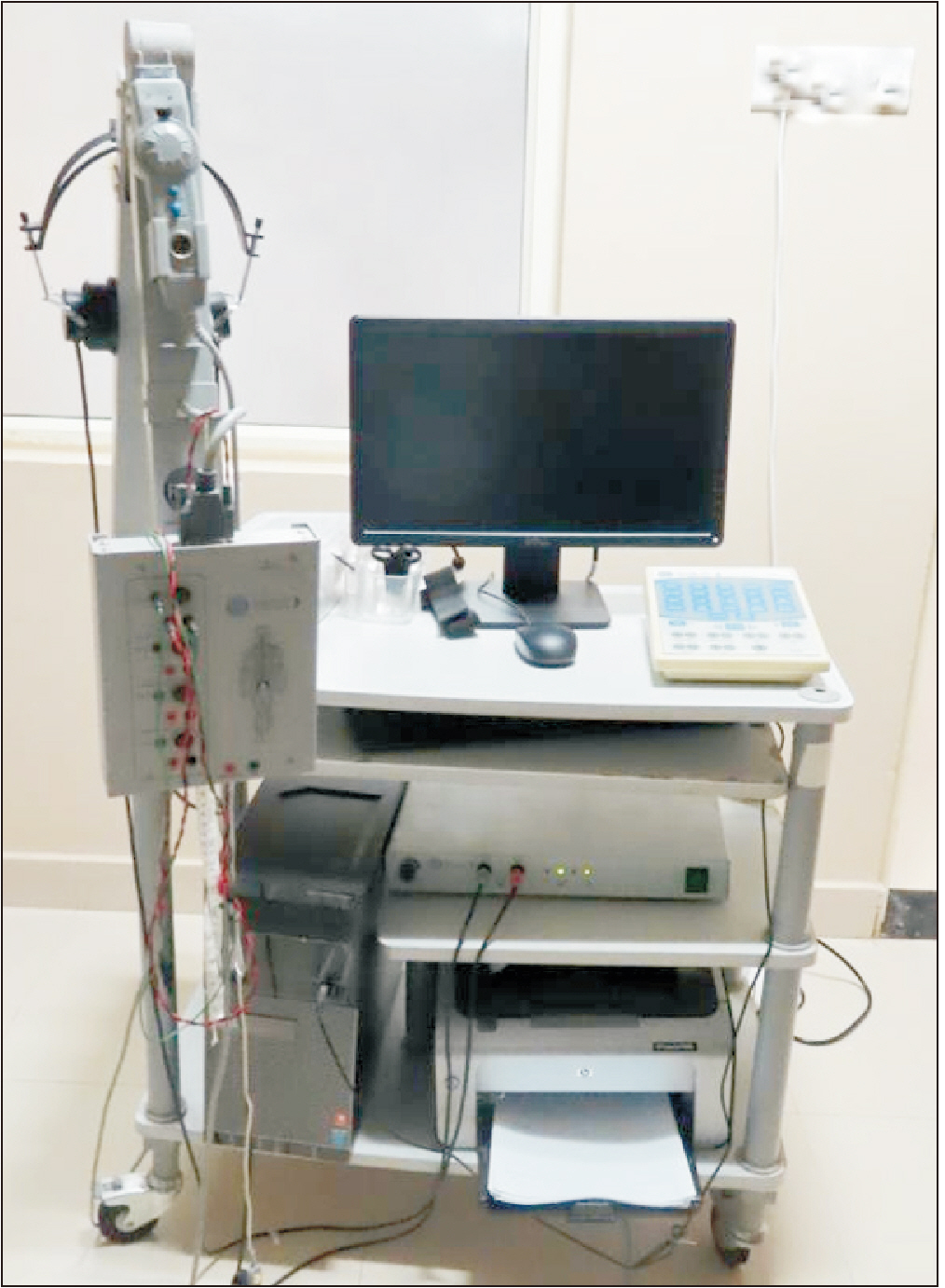
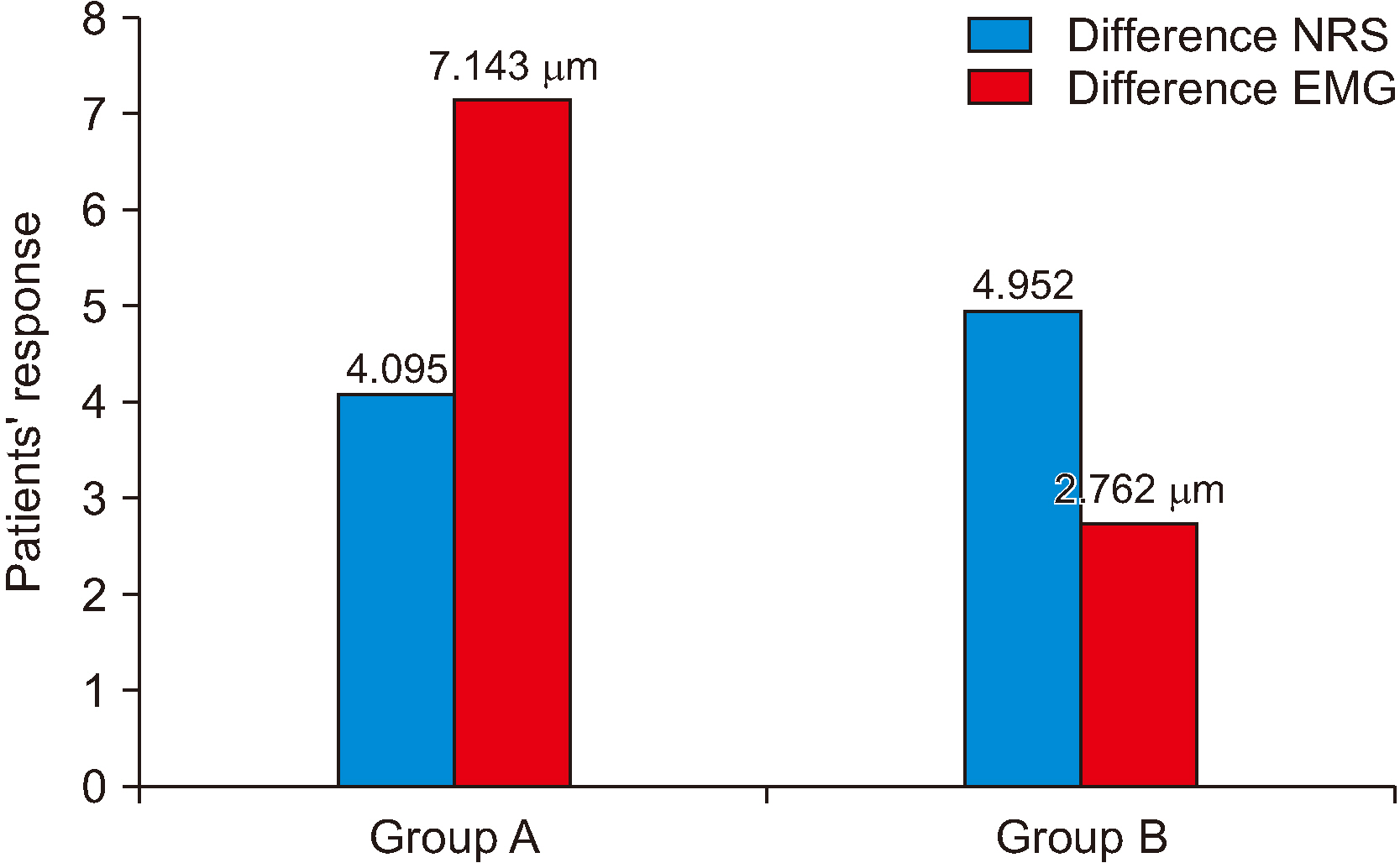
The study was conducted on 42 patients with masticatory myalgia, dividing them into two groups; Group A (21 patients), received moist heat therapy and Group B (21 patients), received ultrasound therapy for seven effective days. Prior and after the treatment the numeric rating scale (NRS) and the electromyography (EMG) scores were recorded and compared. The observations were analyzed clinically and statistical support was taken to assess the NRS and EMG data.
Results
Irrespective of the groups, patients testified a significant reduction in pain after the treatment. From the EMG readings; even though the standard deviation for each group was varied considerably, EMG recorded an improved muscle activity. Statistical analysis was used to assess and identify the best treatment methodology between the two modalities.
Conclusion
From the statistical analysis, it is concluded that, though both the therapies had significantly reduced the symptomatic response, it is moist heat fomentation that improved muscle activity both statistically and clinically in comparison to ultrasound.
Figure
Reference
-
References
1. Okeson JP. 2013. Management of temporomandibular disorders and occlusion. 7th ed. Elsevier;Louis:2. Chethan H, Ganaraj S, Krishna Prasad D. 2015; To evaluate the effect of moist heat fomentation therapy in relieving symptoms of pain related temporomandibular muscle pain disorder. Int J Curr Res. 7:17393–6.3. McNeill C. 1997; Management of temporomandibular disorders: concepts and controversies. J Prosthet Dent. 77:510–22. https://doi.org/10.1016/s0022-3913(97)70145-8 . DOI: 10.1016/S0022-3913(97)70145-8.
Article4. Mohl ND, Lund JP, Widmer CG, McCall WD Jr Jr. 1990; Devices for the diagnosis and treatment of temporomandibular disorders. Part II: electromyography and sonography. J Prosthet Dent. 63:332–6. https://doi.org/10.1016/0022-3913(90)90207-s . DOI: 10.1016/0022-3913(90)90207-S.
Article5. Klasser GD, Okeson JP. 2006; The clinical usefulness of surface electromyography in the diagnosis and treatment of temporomandibular disorders. J Am Dent Assoc. 137:763–71. https://doi.org/10.14219/jada.archive.2006.0288 . DOI: 10.14219/jada.archive.2006.0288. PMID: 16803805.
Article6. Carrara SV, Conti PCR, Barbosa JS. 2010; Statement of the 1st consensus on temporomandibular disorders and orofacial pain. Dent Press J Orthod. 15:114–20. DOI: 10.1590/S2176-94512010000300014.7. Gray RJM, Quayle AA, Hall CA, Schofield MA. 1995; Temporomandibular pain dysfunction: can electrotherapy help? Physiotherapy. 81:47–51. https://doi.org/10.1016/S0031-9406(05)67036-8 . DOI: 10.1016/S0031-9406(05)67036-8.
Article8. Abouelhuda AM, Khalifa AK, Kim YK, Hegazy SA. 2018; Non-invasive different modalities of treatment for temporomandibular disorders: review of literature. J Korean Assoc Oral Maxillofac Surg. 44:43–51. https://doi.org/10.5125/jkaoms.2018.44.2.43 . DOI: 10.5125/jkaoms.2018.44.2.43. PMID: 29732308. PMCID: PMC5932270.
Article9. Miller DL, Smith NB, Bailey MR, Czarnota GJ, Hynynen K, Makin IR. Bioeffects Committee of the American Institute of Ultrasound in Medicine. 2012; Overview of therapeutic ultrasound applications and safety considerations. J Ultrasound Med. 31:623–34. https://doi.org/10.7863/jum.2012.31.4.623 . DOI: 10.7863/jum.2012.31.4.623. PMID: 22441920. PMCID: PMC3810427.
Article10. Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet JP, et al. International RDC/TMD Consortium Network, International association for Dental Research; Orofacial Pain Special Interest Group, International Association for the Study of Pain. 2014; Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. J Oral Facial Pain Headache. 28:6–27. https://doi.org/10.11607/jop.1151 . DOI: 10.11607/jop.1151. PMID: 24482784. PMCID: PMC4478082.
Article11. Breivik H, Borchgrevink PC, Allen SM, Rosseland LA, Romundstad L, Hals EK, et al. 2008; Assessment of pain. Br J Anaesth. 101:17–24. https://doi.org/10.1093/bja/aen103 . DOI: 10.1093/bja/aen103. PMID: 18487245.
Article12. Poindexter RH, Wright EF, Murchison DF. 2002; Comparison of moist and dry heat penetration through orofacial tissues. Cranio. 20:28–33. https://doi.org/10.1080/08869634.2002.11746187 . DOI: 10.1080/08869634.2002.11746187. PMID: 11831341.
Article13. Erickson RI. 1964; Ultrasound-a useful adjunct in temporomandibular joint therapy. Oral Surg Oral Med Oral Pathol. 18:176–9. https://doi.org/10.1016/0030-4220(64)90422-0 . DOI: 10.1016/0030-4220(64)90422-0.
Article14. Möller E, Sheikholeslam A, Lous I. 1984; Response of elevator activity during mastication to treatment of functional disorders. Scand J Dent Res. 92:64–83. https://doi.org/10.1111/j.1600-0722.1984.tb00861.x . DOI: 10.1111/j.1600-0722.1984.tb00861.x. PMID: 6585914.
Article15. Sheikholeslam A, Möller E, Lous I. 1982; Postural and maximal activity in elevators of mandible before and after treatment of functional disorders. Scand J Dent Res. 90:37–46. https://doi.org/10.1111/j.1600-0722.1982.tb01522.x . DOI: 10.1111/j.1600-0722.1982.tb01522.x. PMID: 6952545.
Article16. Yemm R. 1985; A neurophysiological approach to the pathology and aetiology of temporomandibular dysfunction. J Oral Rehabil. 12:343–53. https://doi.org/10.1111/j.1365-2842.1985.tb01289.x . DOI: 10.1111/j.1365-2842.1985.tb01289.x. PMID: 3862796.
Article17. Ries LG, Alves MC, Bérzin F. 2008; Asymmetric activation of temporalis, masseter, and sternocleidomastoid muscles in temporomandibular disorder patients. Cranio. 26:59–64. https://doi.org/10.1179/crn.2008.008 . DOI: 10.1179/crn.2008.008. PMID: 18290526.
Article18. Suvinen TI, Kemppainen P. 2007; Review of clinical EMG studies related to muscle and occlusal factors in healthy and TMD subjects. J Oral Rehabil. 34:631–44. https://doi.org/10.1111/j.1365-2842.2007.01769.x . DOI: 10.1111/j.1365-2842.2007.01769.x. PMID: 17716262.
Article19. Cooper BC, Cooper DL, Lucente FE. 1991; Electromyography of masticatory muscles in craniomandibular disorders. Laryngoscope. 101:150–7. https://doi.org/10.1288/00005537-199102000-00009 . DOI: 10.1288/00005537-199102000-00009. PMID: 1992265.
Article20. Santana-Mora U, Cudeiro J, Mora-Bermúdez MJ, Rilo-Pousa B, Ferreira-Pinho JC, Otero-Cepeda JL, et al. 2009; Changes in EMG activity during clenching in chronic pain patients with unilateral temporomandibular disorders. J Electromyogr Kinesiol. 19:e543–9. https://doi.org/10.1016/j.jelekin.2008.10.002 . DOI: 10.1016/j.jelekin.2008.10.002. PMID: 19041265.
Article21. Gervais RO, Fitzsimmons GW, Thomas NR. 1989; Masseter and temporalis electromyographic activity in asymptomatic, subclinical, and temporomandibular joint dysfunction patients. Cranio. 7:52–7. https://doi.org/10.1080/08869634.1989.11678268 . DOI: 10.1080/08869634.1989.11678268. PMID: 2611899.
Article22. Esposito CJ, Veal SJ, Farman AG. 1984; Alleviation of myofascial pain with ultrasonic therapy. J Prosthet Dent. 51:106–8. https://doi.org/10.1016/s0022-3913(84)80115-8 . DOI: 10.1016/S0022-3913(84)80115-8.
Article23. van der Windt van der Windt, van der Heijden GJ, van den Berg SG, ter Riet G, de Winter AF, Bouter LM. 1999; Ultrasound therapy for musculoskeletal disorders: a systematic review. Pain. 81:257–71. https://doi.org/10.1016/s0304-3959(99)00016-0 . DOI: 10.1016/S0304-3959(99)00016-0.
Article24. Funk D, Swank AM, Adams KJ, Treolo D. 2001; Efficacy of moist heat pack application over static stretching on hamstring flexibility. J Strength Cond Res. 15:123–6. DOI: 10.1519/00124278-200102000-00021. PMID: 11708695.
Article25. Petrofsky J, Bains G, Prowse M, Gunda S, Berk L, Raju C, et al. 2009; Dry heat, moist heat and body fat: are heating modalities really effective in people who are overweight? J Med Eng Technol. 33:361–9. https://doi.org/10.1080/03091900802355508 . DOI: 10.1080/03091900802355508. PMID: 19499453.
Article26. Petrofsky J, Bains G, Prowse M, Gunda S, Berk L, Raju C, et al. 2009; Does skin moisture influence the blood flow response to local heat? A re-evaluation of the Pennes model. J Med Eng Technol. 33:532–7. https://doi.org/10.1080/03091900902952683 . DOI: 10.1080/03091900902952683. PMID: 19484652.
Article27. Gam AN, Johannsen F. 1995; Ultrasound therapy in musculoskeletal disorders: a meta-analysis. Pain. 63:85–91. https://doi.org/10.1016/0304-3959(95)00018-n . DOI: 10.1016/0304-3959(95)00018-N.
Article28. Fouda AAEH. 2014; Ultrasonic therapy as an adjunct treatment of temporomandibular joint dysfunction. J Oral Maxillofac Surg. 117:232–37.29. Young SR, Dyson M. 1990; Effect of therapeutic ultrasound on the healing of full-thickness excised skin lesions. Ultrasonics. 28:175–80. https://doi.org/10.1016/0041-624x(90)90082-y . DOI: 10.1016/0041-624X(90)90082-Y.
Article30. El-Batouty MF, el-Gindy M, el-Shawaf I, Bassioni N, el-Ghaweet A, el-Emam A. 1986; Comparative evaluation of the effects of ultrasonic and ultraviolet irradiation on tissue regeneration. Scand J Rheumatol. 15:381–6. https://doi.org/10.3109/03009748609098208 . DOI: 10.3109/03009748609098208. PMID: 3823796.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Masticatory muscle tenderness in burning mouth syndrome: A case control study
- Effects of soft occlusal appliance therapy for patients with masticatory muscle pain
- Comparative Electromyographic Analysis Of Masticatory Muscles Between Bilateral And Unilateral Masticators
- Association between Temporomandibular Disorder and Masticatory Muscle Weakness: A Case report
- A study on the bite force and the electromyographic activity of masticatory muscle in deepbite