Radiation Dose Reduction without Compromise to Image Quality by Alterations of Filtration and Focal Spot Size in Cerebral Angiography
- Affiliations
-
- 1Department of Radiology, Yonsei University College of Medicine, Seoul 03722, Korea. djkimmd@yuhs.ac
- KMID: 2427241
- DOI: http://doi.org/10.3348/kjr.2017.18.4.722
Abstract
OBJECTIVE
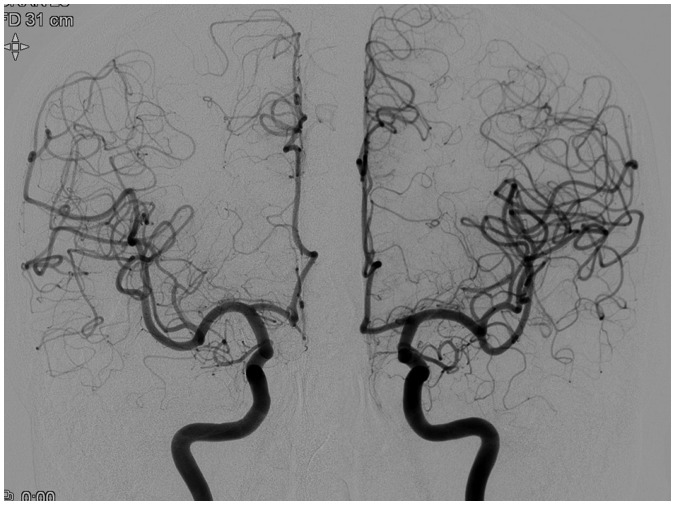
Different angiographic protocols may influence the radiation dose and image quality. In this study, we aimed to investigate the effects of filtration and focal spot size on radiation dose and image quality for diagnostic cerebral angiography using an in-vitro model and in-vivo patient groups.
MATERIALS AND METHODS
Radiation dose and image quality were analyzed by varying the filtration and focal spot size on digital subtraction angiography exposure protocols (1, inherent filtration + large focus; 2, inherent + small; 3, copper + large; 4, copper + small). For the in-vitro analysis, a phantom was used for comparison of radiation dose. For the in-vivo analysis, bilateral paired injections, and patient cohort groups were compared for radiation dose and image quality. Image quality analysis was performed in terms of contrast, sharpness, noise, and overall quality.
RESULTS
In the in-vitro analysis, the mean air kerma (AK) and dose area product (DAP)/frame were significantly lower with added copper filtration (protocols 3 and 4). In the in-vivo bilateral paired injections, AK and DAP/frame were significantly lower with filtration, without significant difference in image quality. The patient cohort groups with added filtration (protocols 3 and 4) showed significant reduction of total AK and DAP/patient without compromise to the image quality. Variations in focal spot size showed no significant differences in radiation dose and image quality.
CONCLUSION
Addition of filtration for angiographic exposure studies can result in significant total radiation dose reduction without loss of image quality. Focal spot size does not influence radiation dose and image quality. The routine angiographic protocol should be judiciously investigated and implemented.
Keyword
MeSH Terms
Figure
Cited by 4 articles
-
Age of Data in Contemporary Research Articles Published in Representative General Radiology Journals
Ji Hun Kang, Dong Hwan Kim, Seong Ho Park, Jung Hwan Baek
Korean J Radiol. 2018;19(6):1172-1178. doi: 10.3348/kjr.2018.19.6.1172.Low-Dose Fluoroscopy Protocol for Diagnostic Cerebral Angiography
Yunsun Song, Seongsik Han, Byung Jun Kim, Seong Heum Oh, Jin Su Kim, Tae Il Kim, Deok Hee Lee
Neurointervention. 2020;15(2):67-73. doi: 10.5469/neuroint.2020.00129.Recent Radiation Reduction Strategies for Neurointerventionists
Jae Ho Shin
Neurointervention. 2020;15(3):167-170. doi: 10.5469/neuroint.2020.00346.Reducing frame rate and pulse rate for routine diagnostic cerebral angiography: ALARA principles in practice
Arvin R. Wali, Sarath Pathuri, Michael G. Brandel, Ryan W. Sindewald, Brian R. Hirshman, Javier A. Bravo, Jeffrey A. Steinberg, Scott E. Olson, Jeffrey S. Pannell, Alexander Khalessi, David Santiago-Dieppa
J Cerebrovasc Endovasc Neurosurg. 2024;26(1):46-50. doi: 10.7461/jcen.2023.E2023.01.007.
Reference
-
1. Alexander MD, Oliff MC, Olorunsola OG, Brus-Ramer M, Nickoloff EL, Meyers PM. Patient radiation exposure during diagnostic and therapeutic interventional neuroradiology procedures. J Neurointerv Surg. 2010; 2:6–10. PMID: 21990551.
Article2. Cohnen M, Wittsack HJ, Assadi S, Muskalla K, Ringelstein A, Poll LW, et al. Radiation exposure of patients in comprehensive computed tomography of the head in acute stroke. AJNR Am J Neuroradiol. 2006; 27:1741–1745. PMID: 16971627.3. Miller DL, Balter S, Cole PE, Lu HT, Schueler BA, Geisinger M, et al. Radiation doses in interventional radiology procedures: the RAD-IR study: part I: overall measures of dose. J Vasc Interv Radiol. 2003; 14:711–727. PMID: 12817038.
Article4. O'Brien B, van der Putten W. Quantification of risk-benefit in interventional radiology. Radiat Prot Dosimetry. 2008; 129:59–62. PMID: 18287187.5. Orbach DB, Stamoulis C, Strauss KJ, Manchester J, Smith ER, Scott RM, et al. Neurointerventions in children: radiation exposure and its import. AJNR Am J Neuroradiol. 2014; 35:650–656. PMID: 24157736.
Article6. Kei Ma W, Hogg P, Norton S. Effects of kilovoltage, milliampere seconds, and focal spot size on image quality. Radiol Technol. 2014; 85:479–485. PMID: 24806050.7. Goh YP, Lau KK, Low K, Buchan K, Oh LC, Kuganesan A, et al. Fine focal spot size improves image quality in computed tomography abdomen and pelvis. Eur Radiol. 2016; 26:4545–4550. PMID: 26973145.
Article8. Söderman M, Mauti M, Boon S, Omar A, Marteinsdóttir M, Andersson T, et al. Radiation dose in neuroangiography using image noise reduction technology: a population study based on 614 patients. Neuroradiology. 2013; 55:1365–1372. PMID: 24005833.
Article9. Mahesh M. Fluoroscopy: patient radiation exposure issues. Radiographics. 2001; 21:1033–1045. PMID: 11452079.
Article10. Aichinger H. Radiation exposure and image quality in X-ray diagnostic radiology: physical principles and clinical applications. 2nd ed. Heidelberg: Springer;2012.11. Kahn EN, Gemmete JJ, Chaudhary N, Thompson BG, Chen K, Christodoulou EG, et al. Radiation dose reduction during neurointerventional procedures by modification of default settings on biplane angiography equipment. J Neurointerv Surg. 2016; 8:819–823. PMID: 26245735.
Article12. Honarmand AR, Shaibani A, Pashaee T, Syed FH, Hurley MC, Sammet CL, et al. Subjective and objective evaluation of image quality in biplane cerebral digital subtraction angiography following significant acquisition dose reduction in a clinical setting. J Neurointerv Surg. 2017; 9:297–301. PMID: 27053704.
Article13. Nicholson R, Tuffee F, Uthappa MC. Skin sparing in interventional radiology: the effect of copper filtration. Br J Radiol. 2000; 73:36–42. PMID: 10721318.
Article14. Kohn ML, Gooch AW Jr, Keller WS. Filters for radiation reduction: a comparison. Radiology. 1988; 167:255–257. PMID: 3347728.
Article15. Law J. The influence of focal spot size on image resolution and test phantom scores in mammography. Br J Radiol. 1993; 66:441–446. PMID: 8319066.
Article16. Chun CW, Kim BS, Lee CH, Ihn YK, Shin YS. Patient radiation dose in diagnostic and interventional procedures for intracranial aneurysms: experience at a single center. Korean J Radiol. 2014; 15:844–849. PMID: 25469098.
Article17. Bushberg J, Seibert J, Leidholdt J, Boone J. essential physics of medical imaging. 3rd ed. Philadelphia: Lippincott Willians & Wilkins;2012.18. Wagner LK, Eifel PJ, Geise RA. Potential biological effects following high X-ray dose interventional procedures. J Vasc Interv Radiol. 1994; 5:71–84. PMID: 8136601.
Article19. Balter S, Hopewell JW, Miller DL, Wagner LK, Zelefsky MJ. Fluoroscopically guided interventional procedures: a review of radiation effects on patients’ skin and hair. Radiology. 2010; 254:326–341. PMID: 20093507.
Article20. Sanchez RM, Vano E, Fernández JM, Moreu M, Lopez-Ibor L. Brain radiation doses to patients in an interventional neuroradiology laboratory. AJNR Am J Neuroradiol. 2014; 35:1276–1280. PMID: 24627454.
Article21. Stecker MS, Balter S, Towbin RB, Miller DL, Vañó E, Bartal G, et al. Guidelines for patient radiation dose management. J Vasc Interv Radiol. 2009; 20(7 Suppl):S263–S273. PMID: 19560006.
Article22. Söderman M, Holmin S, Andersson T, Palmgren C, Babic D, Hoornaert B. Image noise reduction algorithm for digital subtraction angiography: clinical results. Radiology. 2013; 269:553–560. PMID: 23737536.
Article23. Schneider T, Wyse E, Pearl MS. Analysis of radiation doses incurred during diagnostic cerebral angiography after the implementation of dose reduction strategies. J Neurointerv Surg. 2016; 4. 07. [Epub ahead of print]. DOI: 10.1136/neurintsurg-2015-012204.
Article24. Pearl MS, Torok C, Wang J, Wyse E, Mahesh M, Gailloud P. Practical techniques for reducing radiation exposure during cerebral angiography procedures. J Neurointerv Surg. 2015; 7:141–145. PMID: 24489125.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Image quality assessments of focal spot size on radiographic images in dogs
- Attenuation-Based Automatic Tube Potential Selection in Cerebral Computed Tomography Angiography: Effects on Radiation Exposure and Image Quality
- Spot Sign on Initial Brain Computed Tomography Angiography Source Image to Predict Large Hemorrhagic Transformation after Middle Cerebral Artery Infarction
- Reduction of Radiation Dose to Eye Lens in Cerebral 3D Rotational Angiography Using Head Off-Centering by Table Height Adjustment: A Prospective Study
- Low-Dose Three-Dimensional Rotational Angiography for Evaluating Intracranial Aneurysms: Analysis of Image Quality and Radiation Dose