Clin Exp Vaccine Res.
2018 Jan;7(1):70-75. 10.7774/cevr.2018.7.1.70.
Outbreak investigation of pertussis in an elementary school: a case-control study among vaccinated students
- Affiliations
-
- 1Division of Infectious Disease Control, Gyeonggi Provincial Government, Suwon, Korea.
- 2Department of Epidemiology and Medical Informatics, Graduate School of Public Health, Korea University, Seoul, Korea. chun@korea.ac.kr
- 3Office of Preventive Medicine, Centers for Disease Control, Taipei, Taiwan.
- 4Department of Public Health Policy, Osan Public Health Center, Osan, Korea.
- 5Division of Infectious Disease Research, Gyeonggi Province Institute of Health and Environment, Suwon, Korea.
- 6Department of Preventive Medicine, Korea University College of Medicine, Seoul, Korea.
- KMID: 2402540
- DOI: http://doi.org/10.7774/cevr.2018.7.1.70
Abstract
- PURPOSE
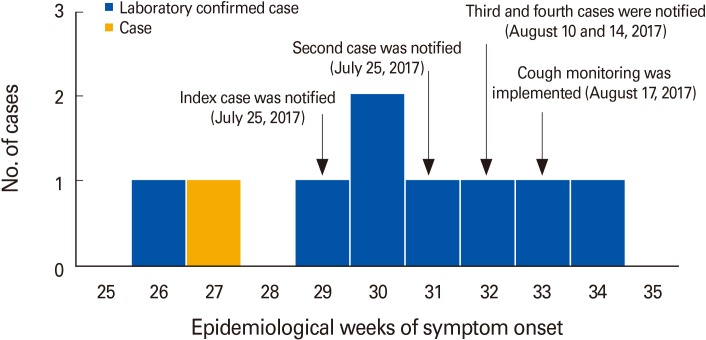
A pertussis patient from an elementary school, in Gyeonggi Province, Korea, was notified to public health authority on July 25, 2017. Epidemiologic investigation was conducted to identify the magnitude, possible source of infection and risk factors for this outbreak on August 17, 2017.
MATERIALS AND METHODS
A case was defined as the school student experiencing cough for more than two weeks with or without paroxysmal, whoop, or post-tussive vomiting. Control was defined as the student polymerase chain reaction-negative at the school. School based surveillance was implemented to identify additional cases.
RESULTS
From June 29 to August 27, 2017, nine patients of pertussis were identified from an elementary school. Among nine cases, eight were confirmed by polymerase chain reaction positive. All cases had cough, one (11%) had post-tussive vomiting, and one (11%) had fever. Eight cases had macrolide for 7 days in outpatient clinic, and one case admitted in a hospital. There was no significant difference of demographic factors including gender (p=0.49), age group (p=0.97), number of series of vaccination of pertussis (p=0.52), the number of participation of after school activity (p=0.28), and the time elapsed since last vaccination (p=0.42). However, we found the history of contact within the classroom or after-school activity was only the independent risk factor among all the demographic factors collected (odds ratio, 63.61; 95% confidence interval, 4.35 to 930.79).
CONCLUSION
The contributing factor for transmission is associated with the case-contact. Immediate identification of pertussis with use of appropriate diagnostic test may help to avoid a large number of cases.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Seroprevalence of Pertussis in Healthcare Workers without Adult Pertussis Vaccine Use at a University Hospital in Korea
Won Suk Choi, Su Hyun Kim, Dae Won Park
J Korean Med Sci. 2018;33(50):. doi: 10.3346/jkms.2018.33.e321.Immunogenicity and Safety of a Newly Developed Tetanus-Diphtheria Toxoid (Td) in Healthy Korean Adolescents: a Multi-center, Randomized, Double-blind, Active-Controlled Phase 3 Trial
Ui Yoon Choi, Ki Hwan Kim, Jin Lee, Byung Wook Eun, Hwang Min Kim, Kyung-Yil Lee, Dong Ho Kim, Sang Hyuk Ma, Jina Lee, Jong-Hyun Kim
J Korean Med Sci. 2021;36(49):e313. doi: 10.3346/jkms.2021.36.e313.
Reference
-
1. Crowcroft NS, Stein C, Duclos P, Birmingham M. How best to estimate the global burden of pertussis? Lancet Infect Dis. 2003; 3:413–418. PMID: 12837346.
Article2. Heymann DL. Control of communicable diseases manual. Washington, DC: American Public Health Association;2008.3. Choe YJ, Park YJ, Jung C, Bae GR, Lee DH. National pertussis surveillance in South Korea 1955–2011: epidemiological and clinical trends. Int J Infect Dis. 2012; 16:e850–e854. PMID: 22921258.
Article4. Roush SW, Murphy TV. Vaccine-Preventable Disease Table Working Group. Historical comparisons of morbidity and mortality for vaccine-preventable diseases in the United States. JAMA. 2007; 298:2155–2163. PMID: 18000199.
Article5. Lee SY, Han SB, Kang JH, Kim JS. Pertussis prevalence in Korean adolescents and adults with persistent cough. J Korean Med Sci. 2015; 30:988–990. PMID: 26130965.
Article6. Korea Centers for Disease Control and Prevention. 2013 Korea National Immunization Survey. Cheongju: Korea Centers for Disease Control and Prevention;2013.7. Korea Centers for Disease Control and Prevention. Disease Web Statistics System [Internet]. Cheongju: Korea Centers for Disease Control and Prevention;2017. cited 2017 Nov 12. Available from: http://is.cdc.go.kr.8. Wendelboe AM, Van Rie A, Salmaso S, Englund JA. Duration of immunity against pertussis after natural infection or vaccination. Pediatr Infect Dis J. 2005; 24(5 Suppl):S58–S61. PMID: 15876927.
Article9. Khetsuriani N, Bisgard K, Prevots DR, et al. Pertussis outbreak in an elementary school with high vaccination coverage. Pediatr Infect Dis J. 2001; 20:1108–1112. PMID: 11740314.
Article10. Korea Centers for Disease Control and Prevention. Case definition for national notifiable infectious disease. Cheongju: Korea Centers for Disease Control and Prevention;2017.11. Korea Centers for Disease Control and Prevention. Guideline for the laboratory diagnosis for national notifiable infectious disease. Cheongju: Korea Centers for Disease Control and Prevention;2016.12. He Q, Viljanen MK, Olander RM, et al. Antibodies to filamentous hemagglutinin of Bordetella pertussis and protection against whooping cough in schoolchildren. J Infect Dis. 1994; 170:705–708. PMID: 8077734.
Article13. Brennan M, Strebel P, George H, et al. Evidence for transmission of pertussis in schools, Massachusetts, 1996: epidemiologic data supported by pulsed-field gel electrophoresis studies. J Infect Dis. 2000; 181:210–215. PMID: 10608769.
Article14. Wang K, Fry NK, Campbell H, et al. Whooping cough in school age children presenting with persistent cough in UK primary care after introduction of the preschool pertussis booster vaccination: prospective cohort study. BMJ. 2014; 348:g3668. PMID: 24961836.
Article15. McNamara LA, Skoff T, Faulkner A, et al. Reduced severity of pertussis in persons with age-appropriate pertussis vaccination-United States, 2010–2012. Clin Infect Dis. 2017; 65:811–818. PMID: 29017283.
Article16. Alamaw SD, Kassa AW, Gelaw YA. Pertussis outbreak investigation of Mekdela district, South Wollo zone, Amhara region, North-West Ethiopia. BMC Res Notes. 2017; 10:420. PMID: 28830538.
Article17. Pawloski LC, Queenan AM, Cassiday PK, et al. Prevalence and molecular characterization of pertactin-deficient Bordetella pertussis in the United States. Clin Vaccine Immunol. 2014; 21:119–125. PMID: 24256623.
Article18. Centers for Disease Control and Prevention (CDC). Schoolassociated pertussis outbreak: Yavapai County, Arizona, September 2002–February 2003. MMWR Morb Mortal Wkly Rep. 2004; 53:216–219. PMID: 15029116.19. Mooi FR, Van Der, De Melker HE. Pertussis resurgence: waning immunity and pathogen adaptation: two sides of the same coin. Epidemiol Infect. 2014; 142:685–694. PMID: 23406868.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Epidemiologic Investigation of a Mumps Outbreak in a Middle School in Pohang, Korea: Effect of vaccination during outbreak
- Update on pertussis and pertussis immunization
- Effects of a Cell Phone Use Education Program on Knowledge, Attitude, Self-efficacy, and Self-control of Cell Phone Use in Elementary School Students
- The Changed Parenting Experiences of Mothers of Elementary School Students in the Face of the COVID-19 Pandemic
- Epidemiological Investigation of a Measles Outbreak in a Preschool in Incheon, Korea, 2006