J Clin Neurol.
2018 Jan;14(1):73-80. 10.3988/jcn.2018.14.1.73.
Partial Conduction Block as an Early Nerve Conduction Finding in Neurolymphomatosis
- Affiliations
-
- 1Department of Neurology, Mokdong Hospital, College of Medicine, Ewha Womans University, Seoul, Korea. pkd1165@ewha.ac.kr
- 2Department of Neurology, Yonsei University College of Medicine, Seoul, Korea. kimsm@yuhs.ac
- 3Department of Pathology, Yonsei University College of Medicine, Seoul, Korea.
- 4Department of Neurology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2399602
- DOI: http://doi.org/10.3988/jcn.2018.14.1.73
Abstract
- BACKGROUND AND PURPOSE
Neurolymphomatosis is a rare manifestation of hematological malignancy and is characterized by direct infiltration of the peripheral nervous system. The objective of this study was to identify the clinical and electrophysiological features of neurolymphomatosis.
METHODS
We retrospectively analyzed the medical records of 13 patients with neurolymphomatosis. Seven (54%) of the patients were men, and the median age at symptom onset was 60.0 years.
RESULTS
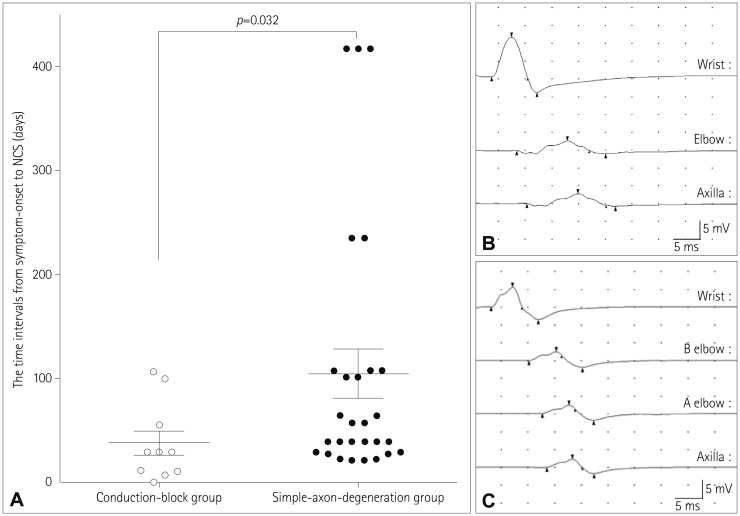
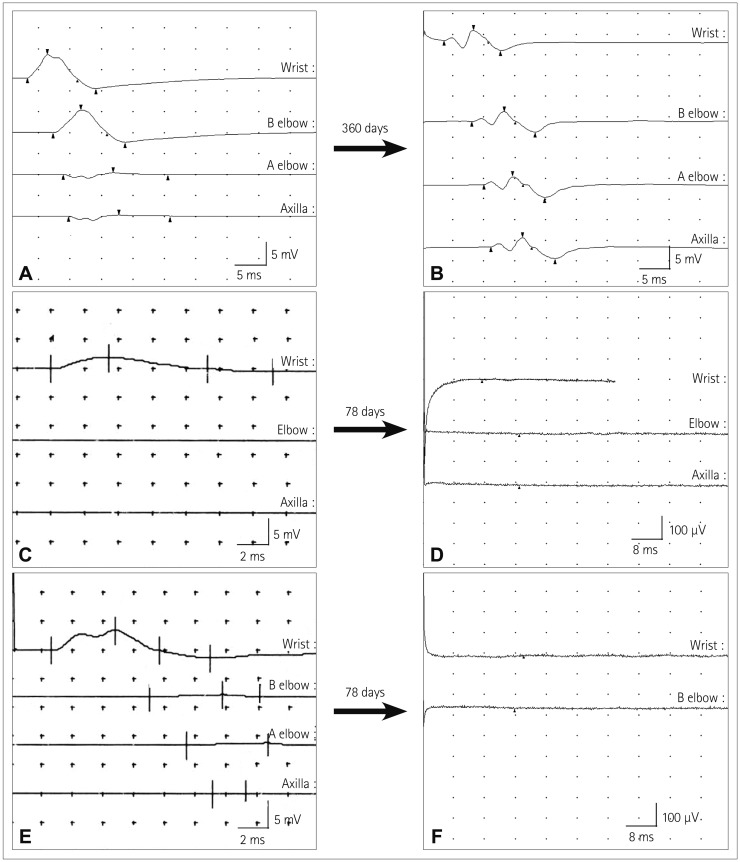
The most common type of underlying malignancy was diffuse large B-cell lymphoma (69%). Twelve patients had painful asymmetric neuropathies. The median survival time after diagnosis was 7 months, and 12 patients died during the study period. Thirty-eight motor nerve conduction studies (NCSs) were performed in the affected nerves. Ten and 28 motor nerves were classified into the conduction-block and simple-axon-degeneration groups, respectively. The median time interval between symptom onset and the NCS was significantly shorter in the conduction-block group than in the simple-axon-degeneration group (p=0.032). However, no significant differences in the motor nerve conduction velocities, terminal latencies, and distal compound muscle action potential amplitudes were identified between the conduction-block and simple-axon-degeneration groups. The conduction-block group showed excessive temporal dispersion in only five of the ten NCSs (50%). Follow-up NCSs revealed that partial conduction blocks had changed into axonal degeneration patterns.
CONCLUSIONS
This is the first study to analyze the electrophysiological features of patients with neurolymphomatosis. Our findings showed that a partial conduction block is not rare and is an early nerve conduction abnormality in neurolymphomatosis.
MeSH Terms
Figure
Reference
-
1. Grisariu S, Avni B, Batchelor TT, van den Bent MJ, Bokstein F, Schiff D, et al. Neurolymphomatosis: an International Primary CNS Lymphoma Collaborative Group report. Blood. 2010; 115:5005–5011. PMID: 20368468.
Article2. Jellinger K, Radiaszkiewicz T. Involvement of the central nervous system in malignant lymphomas. Virchows Arch A Pathol Anat Histol. 1976; 370:345–362. PMID: 826017.
Article3. Matsue K, Hayama BY, Iwama K, Koyama T, Fujiwara H, Yamakura M, et al. High frequency of neurolymphomatosis as a relapse disease of intravascular large B-cell lymphoma. Cancer. 2011; 117:4512–4521. PMID: 21448935.
Article4. Pillay PK, Hardy RW Jr, Wilbourn AJ, Tubbs RR, Lederman RJ. Solitary primary lymphoma of the sciatic nerve: case report. Neurosurgery. 1988; 23:370–371. PMID: 3226515.
Article5. Hughes RA, Britton T, Richards M. Effects of lymphoma on the peripheral nervous system. J R Soc Med. 1994; 87:526–530. PMID: 7932460.6. Kelly JJ, Karcher DS. Lymphoma and peripheral neuropathy: a clinical review. Muscle Nerve. 2005; 31:301–313. PMID: 15543550.
Article7. Chang GY. Evolution of neurolymphomatosis to lymphomatosis cerebri. J Clin Neurol. 2017; 13:203–204. PMID: 28176503.
Article8. von Falck C, Rodt T, Joerdens S, Waldeck S, Kiesel H, Knapp WH, et al. F-18 2-fluoro-2-deoxy-glucose positron emission tomography/computed tomography for the detection of radicular and peripheral neurolymphomatosis: correlation with magnetic resonance imaging and ultrasound. Clin Nucl Med. 2009; 34:493–495. PMID: 19617723.9. Gan HK, Azad A, Cher L, Mitchell PL. Neurolymphomatosis: diagnosis, management, and outcomes in patients treated with rituximab. Neuro Oncol. 2010; 12:212–215. PMID: 20150388.
Article10. Kinoshita H, Yamakado H, Kitano T, Kitamura A, Yamashita H, Miyamoto M, et al. Diagnostic utility of FDG-PET in neurolymphomatosis: report of five cases. J Neurol. 2016; 263:1719–1726. PMID: 27286845.
Article11. Sekiya H, Sekiguchi K, Noda Y, Kowa H, Kanda F, Toda T. Conduction block in neurolymphomatosis. Muscle Nerve. 2015; 52:S117.12. Tomita M, Koike H, Kawagashira Y, Iijima M, Adachi H, Taguchi J, et al. Clinicopathological features of neuropathy associated with lymphoma. Brain. 2013; 136(Pt 8):2563–2578. PMID: 23884813.
Article13. Oh SJ. Clinical Electromyography: Nerve Conduction Studies. 3rd ed. Philadelphia (PA): Lippincott Williams & Wilkins;2003.14. American Association of Electrodiagnostic Medicine. Olney RK. Guidelines in electrodiagnostic medicine. Consensus criteria for the diagnosis of partial conduction block. Muscle Nerve Suppl. 1999; 8:S225–S229. PMID: 16921636.15. Baehring JM, Damek D, Martin EC, Betensky RA, Hochberg FH. Neurolymphomatosis. Neuro Oncol. 2003; 5:104–115. PMID: 12672282.
Article16. Shima K, Ishida C, Okino S, Kotani T, Higashi K, Yamada M. A linear lesion along the brachial plexus on FDG-PET in neurolymphomatosis. Intern Med. 2008; 47:1159–1160. PMID: 18552480.
Article17. Oztürk E, Arpaci F, Kocaoğlu M, Arslan N, Bulakbaşi N, Ozgüven M. Detection of widespread neurolymphomatosis with 18F-FDG PET. Eur J Nucl Med Mol Imaging. 2006; 33:975–976. PMID: 16703365.
Article18. Groth CL, Nevel KS, Gwathmey KG, Bafakih F, Jones DE. Splenic marginal zone lymphoma: an indolent malignancy leading to the development of neurolymphomatosis. Muscle Nerve. 2017; 55:440–444. PMID: 27625159.
Article19. Lagarde S, Tabouret E, Matta M, Franques J, Attarian S, Pouget J, et al. Primary neurolymphomatosis diagnosis and treatment: a retrospective study. J Neurol Sci. 2014; 342(1-2):178–181. PMID: 24831985.
Article20. Shree R, Goyal MK, Modi M, Gaspar BL, Radotra BD, Ahuja CK, et al. The diagnostic dilemma of neurolymphomatosis. J Clin Neurol. 2016; 12:274–281. PMID: 27449910.
Article21. Kokubun N, Nishibayashi M, Uncini A, Odaka M, Hirata K, Yuki N. Conduction block in acute motor axonal neuropathy. Brain. 2010; 133:2897–2908. PMID: 20855419.
Article22. McCluskey L, Feinberg D, Cantor C, Bird S. “Pseudo-conduction block” in vasculitic neuropathy. Muscle Nerve. 1999; 22:1361–1366. PMID: 10487901.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Conduction Block in Hereditary Motor Sensory Neuropathy
- Transient Conduction Block in Vasculitic Neuropathy Caused by Churg-strauss Syndrome: Transient Conduction Block in Vasculitic Neuropathy
- Consecutive Reversible Changes of Peripheral Nerve Conduction in Tetrodotoxification
- Anti-GM1 Antibody Associated Acute Motor Conduction Block Neuropathy Presenting With Reversible Conduction Failure
- Conduction Studies of the Saphenous Nerve in Normal Subjects and Patients with Femoral Neuropathy