J Korean Acad Nurs.
2017 Oct;47(5):613-623. 10.4040/jkan.2017.47.5.613.
Effects of Education about Action Plans according to Self-Monitoring on Self-Management Adherence, Knowledge, Symptom Control, and Quality of Life among Adult Asthma Patients: A Randomized Controlled Trial
- Affiliations
-
- 1College of Nursing, Chonnam National University, Gwangju, Korea. yrk@jnu.ac.kr
- KMID: 2394256
- DOI: http://doi.org/10.4040/jkan.2017.47.5.613
Abstract
- PURPOSE
This study was conducted to identify the effects of education regarding action plans according to a self-monitoring program on self-management adherence, knowledge, symptom control, and health-related quality of life (HRQoL) among adults with asthma.
METHODS
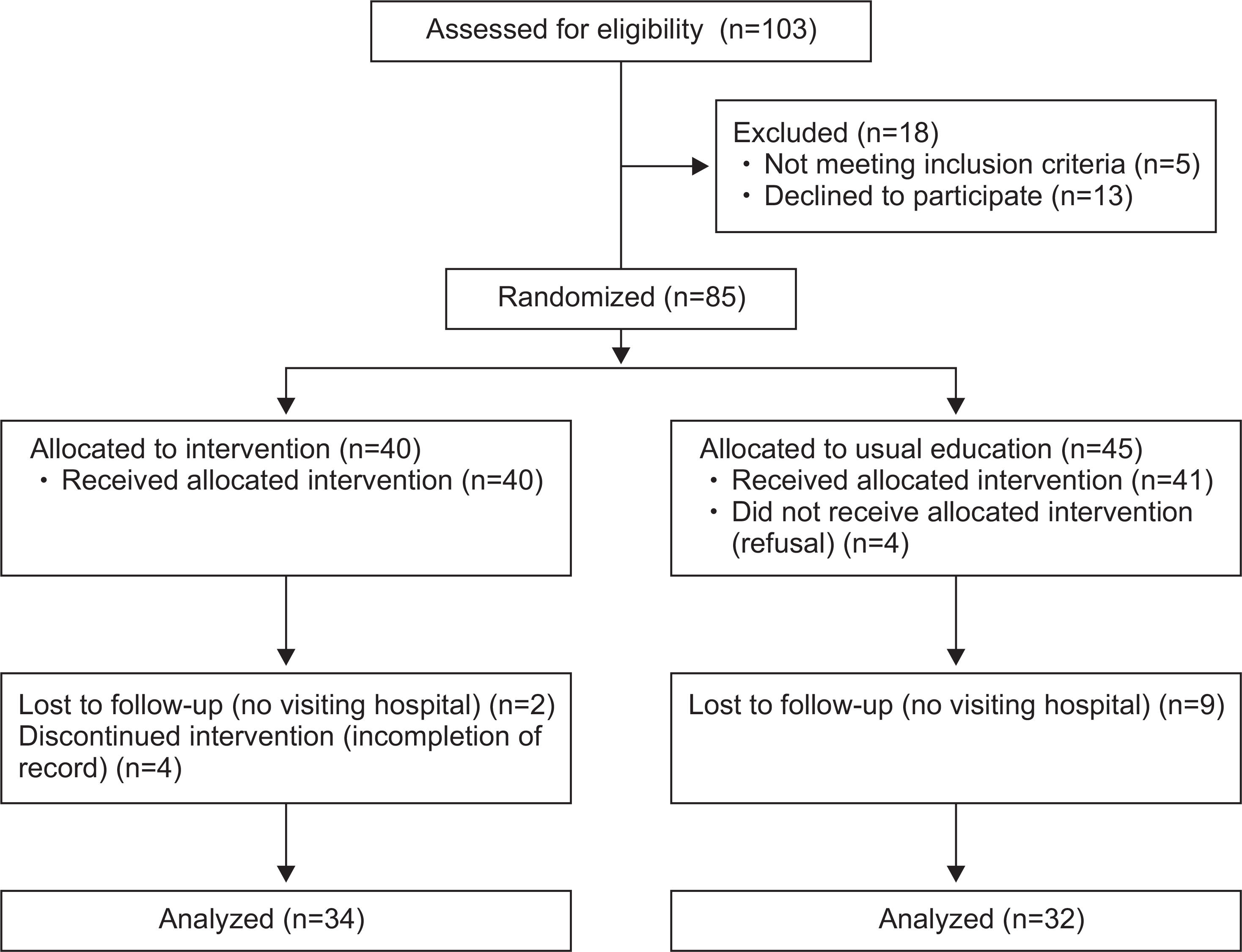
Thirty-four patients were randomly assigned to the intervention group and thirty-two to the control group in this study. A tailored 50-minute intervention based on the contents of self-monitoring and action plans developed by the National Heart Lung and Blood Institute was provided to the intervention group. Structured and well developed questionnaires were used to measure the dependent variables.
RESULTS
There were no differences in all general and clinical characteristics, and the dependent variables between two groups in the pre-test. In the post-test, there were differences in the level of self-management adherence (t=4.41, p<.001), knowledge (t=2.26, p=.027), symptom control (t=-2.56, p=.013), and total HRQoL (t=2.14, p=.036) between the two groups, although there was a difference only in the sub-domain of emotion (t=2.03, p=.047) in HRQoL.
CONCLUSION
This study found that action plans according to self-monitoring that enhance a participatory interaction in the treatment and care could help patients with moderate to severe asthma to engagead equately in self-care, to control their symptoms, and to improve their HRQoL. Further studies are still needed to identify longitudinal effects of this program.
Keyword
Figure
Reference
-
References
1. To T, Stanojevic S, Moores G, Gershon AS, Bateman ED, Cruz AA, et al. Global asthma prevalence in adults: Findings from the cross-sectional world health survey. BMC Public Health. 2012; 12:204. https://doi.org/10.1186/1471-2458-12-204.
Article2. Ministry of Health & Welfare. Korean Centers for Disease Control & Prevention. Korea National Health Statistics 2015: Korea National Health and Nutrition Examination Survey (KNHANES VI-3). Seoul: Korea Centers for Disease Control and Prevention;2016. Dec. Report No.: KNHANES 11-1351159-000027-10.3. Masoli M, Fabian D, Holt S, Beasley R. Global Initiative for Asthma (GINA) Program. The global burden of asthma: Executive summary of the GINA Dissemination Committee report. Allergy. 2004; 59(5):469–478. https://doi.org/10.1111/j.1398-9995.2004.00526.x.4. D’Amato G, Vitale C, Molino A, Stanziola A, Sanduzzi A, Va-trella A, et al. Asthma-related deaths. Multidisciplinary Respiratory Medicine. 2016; 11:37. https://doi.org/10.1186/s40248-016-0073-0.
Article5. Clark NM, Griffiths C, Keteyian SR, Partridge MR. Educational and behavioral interventions for asthma: Who achieves which outcomes? A systematic review. Journal of Asthma and Allergy. 2010; 3:187–197. https://doi.org/10.2147/JAA.S14772.6. Peytremann-Bridevaux I, Arditi C, Gex G, Bridevaux PO, Burnand B. Chronic disease management programmes for adults with asthma. Cochrane Database of Systematic Reviews. 2015; (5). CD007988. https://doi.org/10.1002/14651858.CD007988.pub2.
Article7. Kim DK, Park YB, Oh YM, Jung KS, Yoo JH, Yoo KH, et al. Korean asthma guideline 2014: Summary of major updates to the Korean asthma guideline 2014. Tuberculosis and Respiratory Diseases. 2016; 79(3):111–120. https://doi.org/10.4046/trd.2016.79.3.111.
Article8. Reddel HK, Levy ML. Global Initiative for Asthma Scientific Committee and Dissemination and Implementation Committee. The GINA asthma strategy report: What’s new for primary care? NPJ Primary Care Respiratory Medicine. 2015; 25:15050. https://doi.org/10.1038/npjpcrm.2015.50.9. Adams RJ, Appleton S, Wilson DH, Ruffin RE. Participatory decision making, asthma action plans, and use of asthma medication: A population survey. Journal of Asthma. 2005; 42(8):673–678. https://doi.org/10.1080/02770900500265041.
Article10. Taylor DR, Bateman ED, Boulet LP, Boushey HA, Busse WW, Casale TB, et al. A new perspective on concepts of asthma severity and control. European Respiratory Journal. 2008; 32(3):545–554. https://doi.org/10.1183/09031936.00155307.
Article11. van der Meer V, van Stel HF, Bakker MJ, Roldaan AC, As-sendelft WJ, Sterk PJ, et al. Weekly self-monitoring and treatment adjustment benefit patients with partly controlled and uncontrolled asthma: An analysis of the SMASHING study. Respiratory Research. 2010; 11:74. https://doi.org/10.1186/1465-9921-11-74.
Article12. National Heart Lung and Blood Institute. National asthma education and prevention program expert panel report 3: Guidelines for the diagnosis and management of asthma-summary report 2007 [Internet]. Bethesda (MD): National Heart Lung and Blood Institute;c2007. [cited 2017 Jan 1]. Available from:. https://www.nhlbi.nih.gov/files/docs/guidelines/asthsumm.pdf.13. Arora NK, Weaver KE, Clayman ML, Oakley-Girvan I, Po-tosky AL. Physicians’ decision-making style and psychosocial outcomes among cancer survivors. Patient Education and Counseling. 2009; 77(3):404–412. https://doi.org/10.1016/j.pec.2009.10.004.
Article14. Kwon YS, Choi JY. Effect of self-monitoring rehabilitation program after stroke on physical function, self-efficacy and quality of life. Korean Journal of Rehabilitation Nursing. 2015; 18(2):107–117. https://doi.org/10.7587/kjrehn.2015.107.
Article15. Yun KS, Choi JY. Effects of dietary program based on self-efficacy theory on dietary adherence, physical indices and quality of life for hemodialysis patients. Journal of Korean Academy of Nursing. 2016; 46(4):598–609. https://doi.org/10.4040/jkan.2016.46.4.598.
Article16. Bandura A. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs (NJ): Prentice-Hall;1986. p. 248–287.17. Powell H, Gibson PG. Options for self-management education for adults with asthma. Cochrane Database of Systematic Reviews. 2003; (1). CD004107. https://doi.org/10.1002/14651858.CD004107.
Article18. Mancuso CA, Sayles W, Allegrante JP. Development and testing of the asthma self-management questionnaire. Annals of Allergy, Asthma & Immunology. 2009; 102(4):294–302. https://doi.org/10.1016/S1081-1206(10)60334-1.
Article19. Allen RM, Jones MP. The validity and reliability of an asthma knowledge questionnaire used in the evaluation of a group asthma education self-management program for adults with asthma. Journal of Asthma. 1998; 35(7):537–545.
Article20. Choi JY, Cho Chung HI. Effect of an individualised education programme on asthma control, inhaler use skill, asthma knowledge and health-related quality of life among poorly compliant Korean adult patients with asthma. Journal of Clinical Nursing. 2011; 20(1-2):119–126. https://doi.org/10.1111/j.1365-2702.2010.03420.x.
Article21. Juniper EF, O’Byrne PM, Guyatt GH, Ferrie PJ, King DR. Development and validation of a questionnaire to measure asthma control. European Respiratory Journal. 1999; 14(4):902–907.
Article22. Park JW, Cho YS, Lee SY, Nahm DH, Kim YK, Kim DK, et al. Multi-center study for the utilization of quality of life questionnaire for adult Korean asthmatics (QLQAKA). Journal of Allergy and Clinical Immunology. 2000; 20(3):467–479.23. Patel MR, Valerio MA, Sanders G, Thomas LJ, Clark NM. Asthma action plans and patient satisfaction among women with asthma. Chest. 2012; 142(5):1143–1149. https://doi.org/10.1378/chest.11-1700.
Article24. Kim MY, Lee SY, Jo EJ, Lee SE, Kang MG, Song WJ, et al. Feasibility of a smartphone application based action plan and monitoring in asthma. Asia Pacific Allergy. 2016; 6(3):174–180. https://doi.org/10.5415/apallergy.2016.6.3.174.
Article25. Kelso JM. Do written asthma action plans improve outcomes? Pediatric Allergy, Immunology, and Pulmonology. 2016; 29(1):2–5. https://doi.org/10.1089/ped.2016.0634.
Article26. Yin HS, Gupta RS, Mendelsohn AL, Dreyer B, van Schaick L, Brown CR, et al. Use of a low-literacy written action plan to improve parent understanding of pediatric asthma management: A randomized controlled study. Journal of Asthma. 2017; Forthcoming. https://doi.org/10.1080/02770903.2016.1277542.
Article27. Raju JD, Soni A, Aziz N, Tiemstra JD, Hasnain M. A patient-centered telephone intervention using the asthma action plan. Family Medicine. 2012; 44(5):348–350.28. Plaza V, Peiró M, Torrejón M, Fletcher M, López-Viña A, Ignacio JM, et al. A repeated short educational intervention improves asthma control and quality of life. European Respiratory Journal. 2015; 46(5):1298–1307. https://doi.org/10.1183/13993003.00458-2015.
Article29. Gosavi S, Nadig P, Haran A. Factors contributing towards poor asthma control in patients on regular medication. Journal of Clinical and Diagnostic Research. 2016; 10(6):OC31–OC35. https://doi.org/10.7860/JCDR/2016/18670.8052.
Article30. Pur Ozyigit L, Ozcelik B, Ozcan Ciloglu S, Erkan F. The effectiveness of a pictorial asthma action plan for improving asthma control and the quality of life in illiterate women. Journal of Asthma. 2014; 51(4):423–428. https://doi.org/10.3109/02770903.2013.863331.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Symptom Experiences and Quality of Life in People with Asthma
- Written Asthma Action Plan Improves Asthma Control and the Quality of Life among Pediatric Asthma Patients in Malaysia: A Randomized Control Trial
- Effects of an intensive asthma education program on asthmatic children and their caregivers
- The Effects of Smart Program for Patients Who Underwent Percutaneous Coronary Intervention (SP-PCI) on Disease-Related Knowledge, Health Behavior, and Quality of Life: A Non-Randomized Controlled Trial
- Structural Equation Model of Health-Related Quality of Life in School Age Children with Asthma