Intest Res.
2016 Oct;14(4):322-332. 10.5217/ir.2016.14.4.322.
Surgical management of inflammatory bowel disease in China: a systematic review of two decades
- Affiliations
-
- 1Department of Gastroenterology, The First Affiliated Hospital of Sun Yat-sen University, Guangzhou, China. chenminhu@vip.163.com maoren2023@163.com
- 2Department of Colorectal Surgery, The Sixth Affiliated Hospital of Sun Yat-sen University, Guangzhou, China.
- 3Department of Medicine and Therapeutics, Institute of Digestive Disease, State Key Laboratory of Digestive Diseases, Chinese University of Hong Kong, Hong Kong, China.
- 4Department of General Surgery, The First Affiliated Hospital of Sun Yat-sen University, Guangzhou, China.
- 5IBD Service, Department of Gastroenterology, Sheba Medical Center & Sackler School of Medicine, Tel-Aviv University, Tel Hashomer, Israel.
- KMID: 2354950
- DOI: http://doi.org/10.5217/ir.2016.14.4.322
Abstract
- BACKGROUND/AIMS
The past decades have seen increasing incidence and prevalence of inflammatory bowel disease (IBD) in China. This article aimed to summarize the current status and characteristics of surgical management for IBD in China.
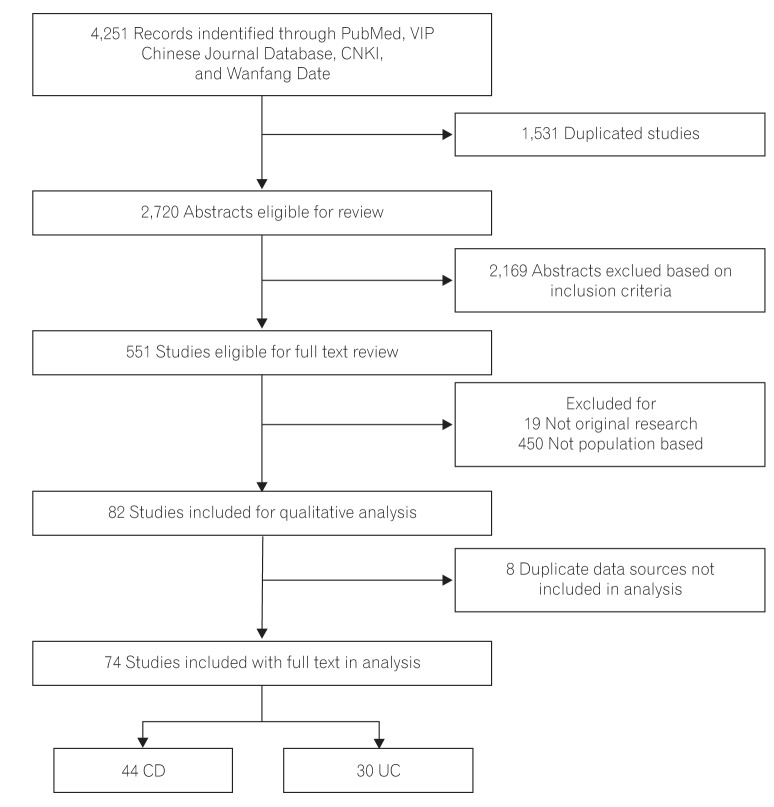
METHODS
We searched PubMed, Embase, and Chinese databases from January 1, 1990 to July 1, 2014 for all relevant studies on the surgical treatment IBD in China. Eligible studies with sufficient defined variables were further reviewed for primary and secondary outcome measures.
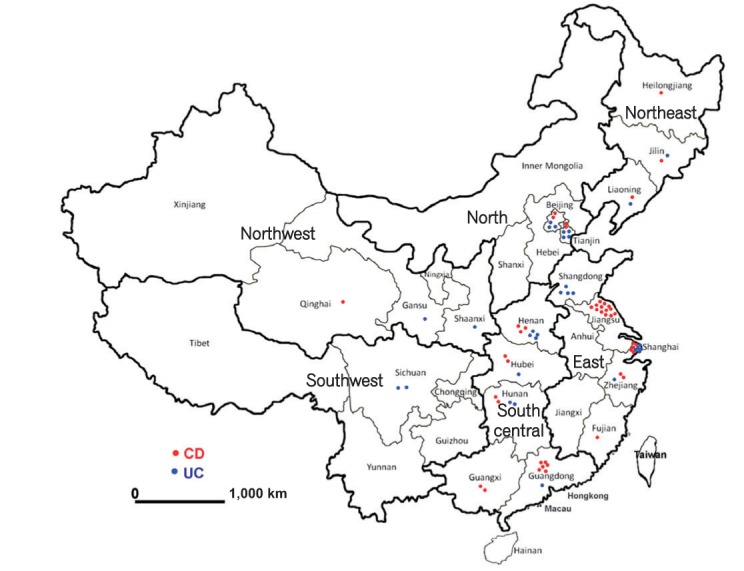
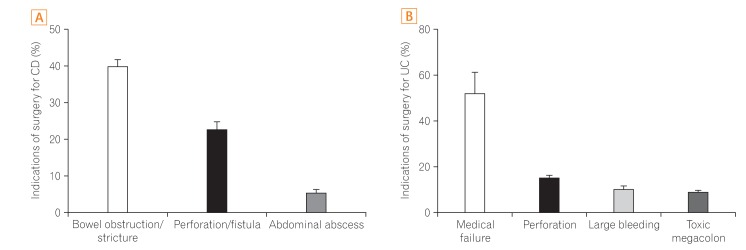
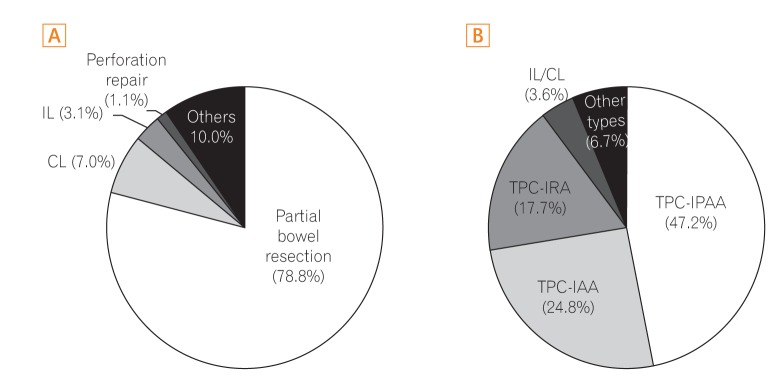
RESULTS
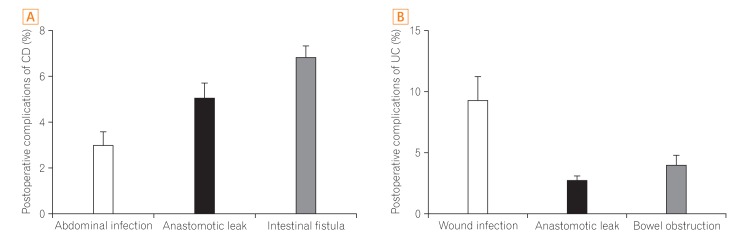
A total of 74 studies comprising 2,007 subjects with Crohn's disease (CD) and 1,085 subjects with ulcerative colitis (UC) were included. The percentage of CD patients misdiagnosed before surgery, including misdiagnosis as appendicitis or UC, was 50.8%±30.9% (578/1,268). The overall postoperative complication rate was 22.3%±13.0% (267/1,501). For studies of UC, the overall postoperative complication rate was 22.2%±27.9% (176/725). In large research centers (n>50 surgical cases), the rates of emergency operations for CD (P=0.032) and in-hospital mortalities resulting from both CD and UC were much lower than those in smaller research centers (n≤50 surgical cases) (P=0.026 and P <0.001, respectively). Regarding the changes in CD and UC surgery over time, postoperative complications (P=0.045 for CD; P=0.020 for UC) and postoperative in-hospital mortality (P=0.0002 for CD; P=0.0160 for UC) both significantly improved after the year 2010.
CONCLUSIONS
The surgical management of IBD in China has improved over time. However, the rates of misdiagnosis and postoperative complications over the past two decades have remained high. Large research centers were found to have relatively better capacity for surgical management than the smaller ones. Higher quality prospective studies are needed in China.
MeSH Terms
Figure
Cited by 1 articles
-
Laparoscopic surgery contributes to a decrease in short-term complications in surgical ulcerative colitis patients during 2008–2017: a multicenter retrospective study in China
Zerong Cai, Xiaosheng He, Jianfeng Gong, Peng Du, Wenjian Meng, Wei Zhou, Jinbo Jiang, Bin Wu, Weitang Yuan, Qi Xue, Lianwen Yuan, Jinhai Wang, Jiandong Tai, Jie Liang, Weiming Zhu, Ping Lan, Xiaojian Wu
Intest Res. 2023;21(2):235-243. doi: 10.5217/ir.2022.00012.
Reference
-
2. Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012; 142:46–54.e42. PMID: 22001864.
Article3. Ng SC, Tang W, Ching JY, et al. Incidence and phenotype of inflammatory bowel disease based on results from the Asia-pacific Crohn's and colitis epidemiology study. Gastroenterology. 2013; 145:158–165.e2. PMID: 23583432.
Article4. Ouyang Q, Wang YF, Hu RW. Epidemiology of inflammatory bowel disease in China. Chung Hua Hsiao Hua Tsa Chih. 2008; 28:814–818.
Article5. Zeng Z, Zhu Z, Yang Y, et al. Incidence and clinical characteristics of inflammatory bowel disease in a developed region of Guangdong province, China: a prospective population-based study. J Gastroenterol Hepatol. 2013; 28:1148–1153. PMID: 23432198.
Article6. Zhao J, Ng SC, Lei Y, et al. First prospective, population-based inflammatory bowel disease incidence study in mainland of China: the emergence of "Western" disease. Inflamm Bowel Dis. 2013; 19:1839–1845. PMID: 23669403.7. Dignass A, Lindsay JO, Sturm A, et al. Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 2: current management. J Crohns Colitis. 2012; 6:991–1030. PMID: 23040451.
Article8. Rutgeerts P, Geboes K, Vantrappen G, Kerremans R, Coenegrachts JL, Coremans G. Natural history of recurrent Crohn's disease at the ileocolonic anastomosis after curative surgery. Gut. 1984; 25:665–672. PMID: 6735250.
Article9. Frolkis AD, Dykeman J, Negrón ME, et al. Risk of surgery for inflammatory bowel diseases has decreased over time: a systematic review and meta-analysis of population-based studies. Gastroenterology. 2013; 145:996–1006. PMID: 23896172.
Article10. Li XF, Lu FG, Zou YY, Ouyang CH, Ye LJ, Wang ZG. Analysis of clinical characteristics of 43 surgical patients with Crohn disease using the Montreal classification. Zhonghua Wei Chang Wai Ke Za Zhi. 2010; 13:210–212. PMID: 20336541.11. Zhou J, Wang JP, Wang J, et al. Analysis of surgical treatment of Crohn's disease: a report of 85 cases. Chin J Pract Surg. 2007; 27:211–213.12. Pan Y, Ouyang Q, Hu RW. Analysis of surgical treatment for severe ulcerative colitis. Zhonghua Wei Chang Wai Ke Za Zhi. 2010; 13:430–432. PMID: 20577922.13. Inflammatory Bowel Disease Cooperation Group of China. Wang YF, Ouyang Q. A retrospective study of 3100 inpatients with ulcerative colitis in China. Chung Hua Hsiao Hua Tsa Chih. 2006; 26:368–372.14. Bernstein CN, Loftus EV Jr, Ng SC, Lakatos PL, Moum B. Epidemiology and Natural History Task Force of the International Organization for the Study of Inflammatory Bowel Disease (IOIBD). Hospitalisations and surgery in Crohn's disease. Gut. 2012; 61:622–629. PMID: 22267595.
Article15. Gao X, Yang RP, Chen MH, et al. Risk factors for surgery and postoperative recurrence: analysis of a south China cohort with Crohn's disease. Scand J Gastroenterol. 2012; 47:1181–1191. PMID: 22845663.
Article16. Peyrin-Biroulet L, Harmsen WS, Tremaine WJ, Zinsmeister AR, Sandborn WJ, Loftus EV Jr. Surgery in a population-based cohort of Crohn's disease from Olmsted County, Minnesota (1970-2004). Am J Gastroenterol. 2012; 107:1693–1701. PMID: 22945286.
Article17. Truelove SC, Witts LJ. Cortisone in ulcerative colitis; final report on a therapeutic trial. Br Med J. 1955; 2:1041–1048. PMID: 13260656.18. Inflammatory Bowel Disease Cooperation Group of China. Recommendation of inflixmab treatment for Crohn's disease. Chung Hua Hsiao Hua Tsa Chih. 2008; 28:847–849.19. Li SR, Lu XJ, Sheng JQ, Fan J, Li S, Zhao X. Comparison of the treating effects of infliximab in Crohn's disease and ulcerative colitis. Weichangbingxue He Ganbingxue Zazhi. 2010; 19:644–647.20. Sun YY, Wu YF, Xu C, et al. Efficacy of infliximab in treatment of patients with Crohn's disease. Acad J Second Mil Med Univ. 2010; 31:338–339.
Article21. Wang YJ, Li ZY, Sun L, Peng Q, Liu L. Clinical observation for the combination of intestinal probiotics and infliximab in treatment of refractory Crohn's disease. China Mod Dr. 2010; (22):119.22. Wu DP, Zheng P. Efficacy infliximab of treatment in 11 patients with Crohn's disease. Int J Dig Dis. 2010; 30:314–318.23. Zhou AC, Jin HY. Application of infliximab in treating Crohn's disease. Med Recapitulate. 2010; 16:3786–3788.24. Leong RW, Lau JY, Sung JJ. The epidemiology and phenotype of Crohn's disease in the Chinese population. Inflamm Bowel Dis. 2004; 10:646–651. PMID: 15472528.
Article25. Jiang L, Xia B, Li J, et al. Retrospective survey of 452 patients with inflammatory bowel disease in Wuhan city, central China. Inflamm Bowel Dis. 2006; 12:212–217. PMID: 16534423.
Article26. Brant SR, Nguyen GC. Is there a gender difference in the prevalence of Crohn's disease or ulcerative colitis? Inflamm Bowel Dis. 2008; 14(Suppl 2):S2–S3. PMID: 18816735.
Article27. Bernstein CN, Blanchard JF, Rawsthorne P, Wajda A. Epidemiology of Crohn's disease and ulcerative colitis in a central Canadian province: a population-based study. Am J Epidemiol. 1999; 149:916–924. PMID: 10342800.
Article28. Ng SC, Bernstein CN, Vatn MH, et al. Geographical variability and environmental risk factors in inflammatory bowel disease. Gut. 2013; 62:630–649. PMID: 23335431.
Article29. Vind I, Riis L, Jess T, et al. Increasing incidences of inflammatory bowel disease and decreasing surgery rates in Copenhagen City and County, 2003-2005: a population-based study from the Danish Crohn colitis database. Am J Gastroenterol. 2006; 101:1274–1282. PMID: 16771949.
Article30. Moum B, Vatn MH, Ekbom A, et al. Incidence of ulcerative colitis and indeterminate colitis in four counties of southeastern Norway, 1990-93: a prospective population-based study: the Inflammatory Bowel South-Eastern Norway (IBSEN) Study Group of gastroenterologists. Scand J Gastroenterol. 1996; 31:362–366. PMID: 8726304.
Article31. Lehtinen P, Ashorn M, Iltanen S, et al. Incidence trends of pediatric inflammatory bowel disease in Finland, 1987-2003, a nationwide study. Inflamm Bowel Dis. 2011; 17:1778–1783. PMID: 21744433.
Article32. Yang H, Li Y, Wu W, et al. The incidence of inflammatory bowel disease in Northern China: a prospective population-based study. PLoS One. 2014; 9:e101296. DOI: 10.1371/journal.pone.0101296. PMID: 25029440.
Article33. Infections Bowel. The consensus on diagnosis and management of inflammatory bowel disease (2012 Guangzhou). Chin J Gastroenterol. 2012; (12):763–781.34. Rungoe C, Langholz E, Andersson M, et al. Changes in medical treatment and surgery rates in inflammatory bowel disease: a nationwide cohort study 1979-2011. Gut. 2014; 63:1607–1616. PMID: 24056767.
Article35. Clemente V, Aratari A, Papi C, Vernia P. Short term colectomy rate and mortality for severe ulcerative colitis in the last 40 years: has something changed? Dig Liver Dis. 2016; 48:371–375. PMID: 26854257.
Article36. Caprilli R, Viscido A, Latella G. Current management of severe ulcerative colitis. Nat Clin Pract Gastroenterol Hepatol. 2007; 4:92–101. PMID: 17268544.
Article37. Bernell O, Lapidus A, Hellers G. Risk factors for surgery and recurrence in 907 patients with primary ileocaecal Crohn's disease. Br J Surg. 2000; 87:1697–1701. PMID: 11122187.
Article38. Michelassi F, Melis M, Rubin M, Hurst RD. Surgical treatment of anorectal complications in Crohn's disease. Surgery. 2000; 128:597–603. PMID: 11015093.
Article39. Han Y, Lin MB, He YG, et al. Laparoscopic surgery for inflammmatory bowel disease: the experience in China. J Invest Surg. 2013; 26:180–185. PMID: 23514051.
Article40. Fazio VW, Marchetti F. Recurrent Crohn's disease and resection margins: bigger is not better. Adv Surg. 1999; 32:135–168. PMID: 9891742.41. Dietz DW, Laureti S, Strong SA, et al. Safety and longterm efficacy of strictureplasty in 314 patients with obstructing small bowel Crohn's disease. J Am Coll Surg. 2001; 192:330–337. PMID: 11245375.
Article42. Cohen JL, Strong SA, Hyman NH, et al. Practice parameters for the surgical treatment of ulcerative colitis. Dis Colon Rectum. 2005; 48:1997–2009. PMID: 16258712.
Article43. Camilleri-Brennan J, Munro A, Steele RJ. Does an ileoanal pouch offer a better quality of life than a permanent ileostomy for patients with ulcerative colitis? J Gastrointest Surg. 2003; 7:814–819. PMID: 13129563.
Article44. MacLean AR, Cohen Z, MacRae HM, et al. Risk of small bowel obstruction after the ileal pouch-anal anastomosis. Ann Surg. 2002; 235:200–206. PMID: 11807359.
Article45. Heuschen UA, Hinz U, Allemeyer EH, et al. Risk factors for ileoanal J pouch-related septic complications in ulcerative colitis and familial adenomatous polyposis. Ann Surg. 2002; 235:207–216. PMID: 11807360.
Article46. Galandiuk S, Scott NA, Dozois RR, et al. Ileal pouch-anal anastomosis: reoperation for pouch-related complications. Ann Surg. 1990; 212:446–452. PMID: 2171442.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Systematic Review of Recent Lipidomics Approaches Toward Inflammatory Bowel Disease
- Nutritional concerns in pediatric inflammatory bowel disease
- A Comprehensive Review of Inflammatory Bowel Disease Focusing on Surgical Management
- The Pharmacotherapy of Inflammatory Bowel Disease in Child and Adolescence
- Inflammatory Bowel Disease in Pediatric Age