J Korean Ophthalmol Soc.
2011 Sep;52(9):1099-1103.
Temporary Severe Neurogenic Blepharoptosis after Reconstruction of Orbital Medial Wall Fracture
- Affiliations
-
- 1Department of Ophthalmology, St. Vincent's Hospital, The Catholic University of Korea College of Medicine, Suwon, Korea. laty@catholic.ac.kr
Abstract
- PURPOSE
To report two cases of temporary severe neurogenic blepharoptosis after successful reconstruction of orbital medial wall fracture.
CASE SUMMARY
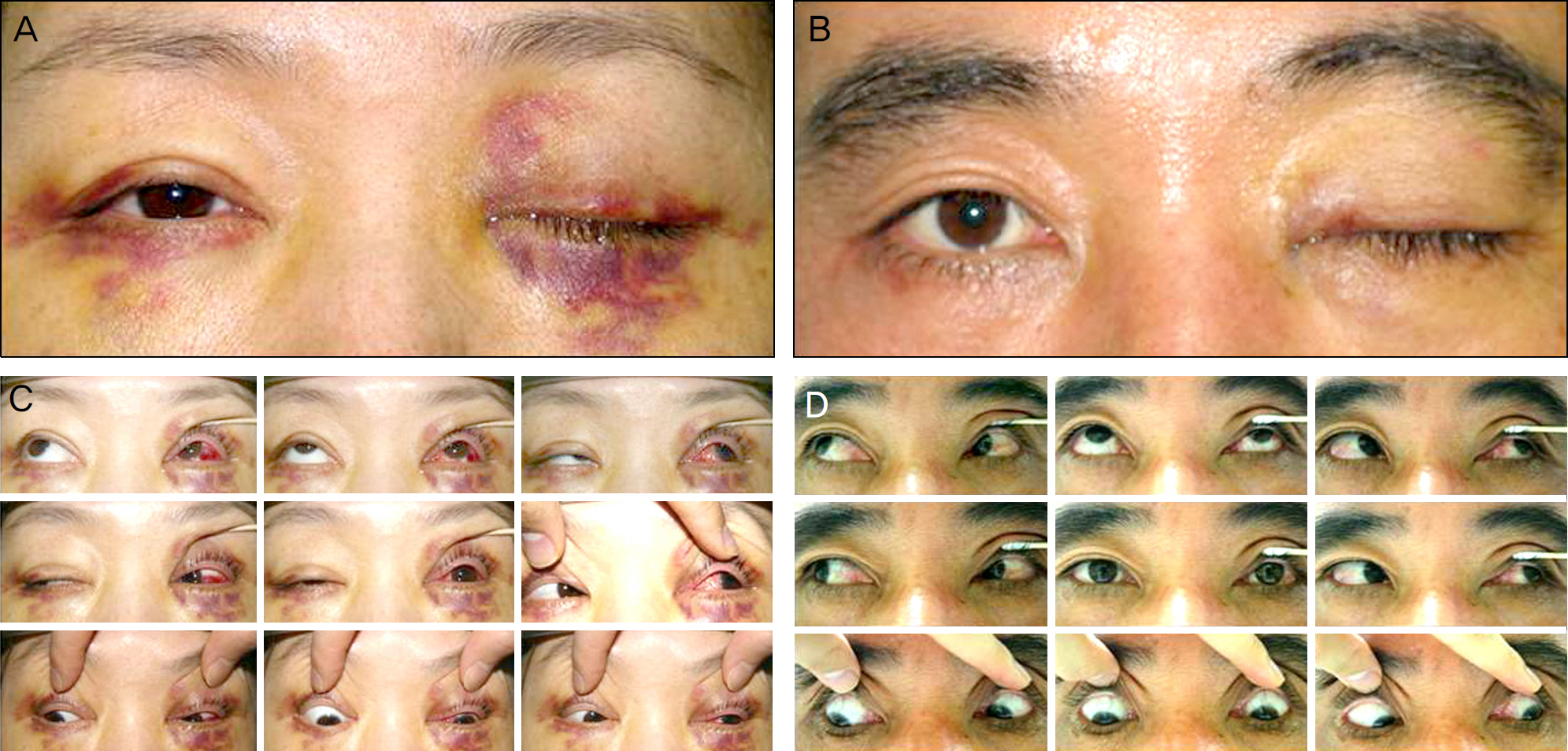
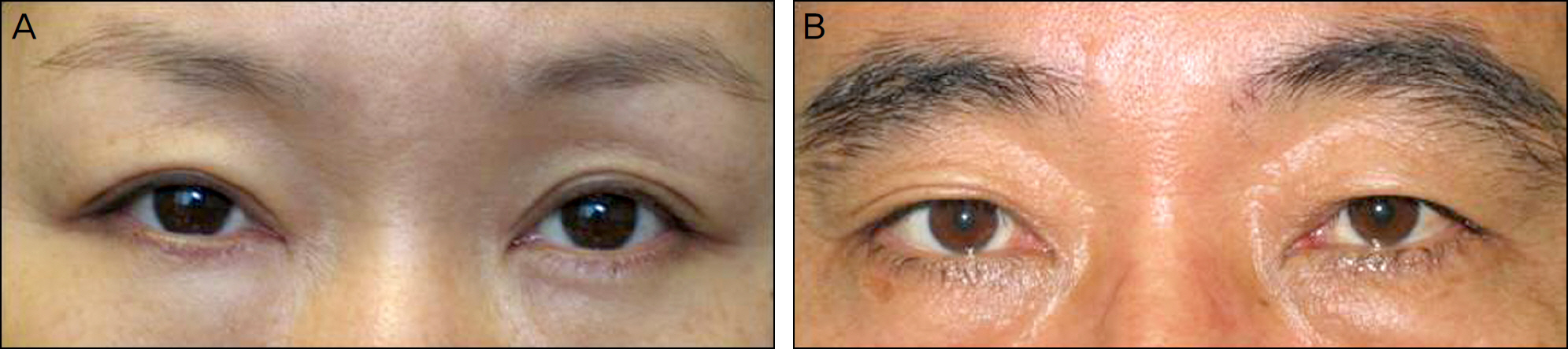
A 36-year-old woman and a 52-year-old man received orbital medial wall reconstruction with Medpor(R) for large fractures. Before the operation, the patients had only moderate swelling of the lid and periorbital ecchymosis. There were no limitations of extraocular muscles or ptosis. The operations were successful, although the patients developed unilateral complete ptosis with totally impaired levetor muscle function immediately after recovering from anesthesia. There were no anisocoria or limitations of the extraocular muscles. After oral steroid therapy, the patients began to improve on postoperative day 4 and after one month, respectively, and recovered to normal lid height and levator function after two months.
CONCLUSIONS
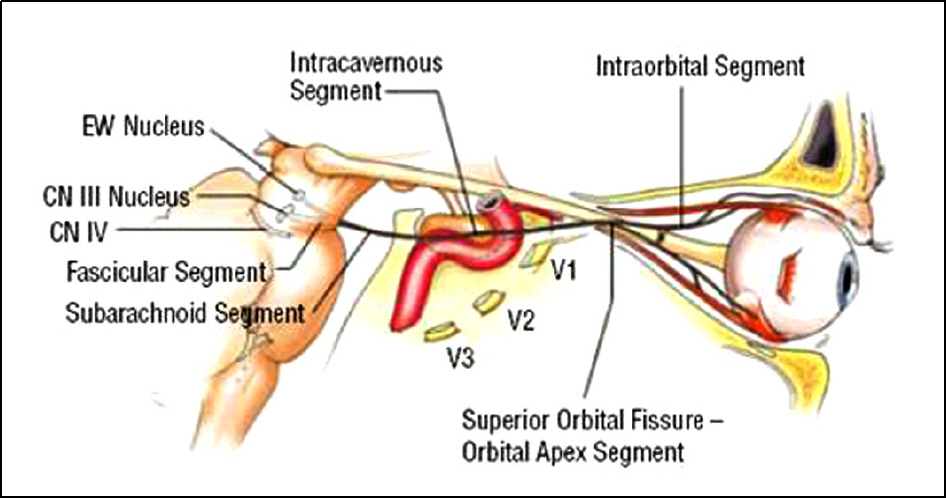
Blepharoptosis after orbital medial wall reconstruction may result from ischemic damage at the end of the superior branch of the oculomotor nerve in the orbit due to compressive and tractional manipulation. Although very rare and temporary, this complication should be considered important because the occurrence can be unpredictable and may cause dissatisfaction to the surgeon and the patient after a successful operation.
MeSH Terms
Figure
Reference
-
References
1. Jung JW, Chi MJ. Temporary unilateral neurogenic blepharoptosis after orbital medial wall reconstruction: 3 cases. Ophthalmologica. 2008; 222:360–2.
Article2. McCulley TJ, Kersten RC, Yip CC, Kulwin DR. Isolated unilateral neurogenic blepharoptosis secondary to eyelid trauma. Am J Ophthalmol. 2002; 134:626–7.
Article3. Stefanis L, Przedborski S. Isolated palsy of the superior branch of the oculomotor nerve due to chronic erosive sphenoid sinusitis. Journal of clinical neuro-ophthalmology. 1993; 13:229–31.4. Small KW, Buckley EG. Recurrent blepharoptosis secondary to a pituitary tumor. Am J Ophthalmol. 1988; 106:760–1.
Article5. Yen MY, Liu JH, Jaw SJ. Ptosis as a early manifestation of pituitary tumor. Br J Ophthalmol. 1990; 74:188–91.6. Bhatti MT, Eisenschenk S, Roper SN, Guy JR. Superior divisional third cranial nerve paresis: clinical and anatomical observations of 2 unique cases. Arch Neurol. 2006; 63:771–6.7. Derakhshan I. Superior branch palsy of the oculomotor nerve with spontaneous recovery. Ann Neurol. 1978; 4:478–9.
Article8. Foroozan R, Bhatti MT, Rhoton AL. Transsphenoidal diplopia. Surv Ophthalmol. 2004; 49:349–58.
Article9. Peter NM, Pearson AR. Orbital apex syndrome from blunt ocular trauma. Orbit. 2010; 29:42–4.
Article10. Brent BD, May DR. Orbital apex syndrome after penetrating orbital trauma. Ann Ophthalmol. 1990; 22:267–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Postoperative Neurogenic Blepharoptosis after Repair of a Medial Orbital Wall Fracture Using the Transcaruncular Approach
- Treatment of Severe Blepharoptosis after Blow Out Fracture
- Management Of Medial Orbital Wall Fracture
- Comparison of Titanium Micro Mesh(R) with Titanium Mesh Screen 1.3(R) in the Reconstruction of Medial Orbital wall Fracture
- Reconstruction of Isolated Medial Orbital Wall Fracture Using a Transcaruncular Approach