J Korean Ophthalmol Soc.
2010 Dec;51(12):1584-1589.
Comparison of the Stability Between Three-piece and Single-piece Aspheric Intraocular Lenses
- Affiliations
-
- 1Department of Ophthalmology, SahmYook Seoul Hospital, Seoul, Korea.
- 2Department of Ophthalmology, St, Mary's Hospital, The Catholic University of Korea School of Medicine, Seoul, Korea. eyedoc@catholic.ac.kr
Abstract
- PURPOSE
The goal of the present study was to compare the stability of the 3-piece (Tecnis ZA9003) and single-piece (AcrySof IQ) aspheric intraocular lenses (IOL) by testing decentration, tilt, anterior chamber depth, and refraction.
METHODS
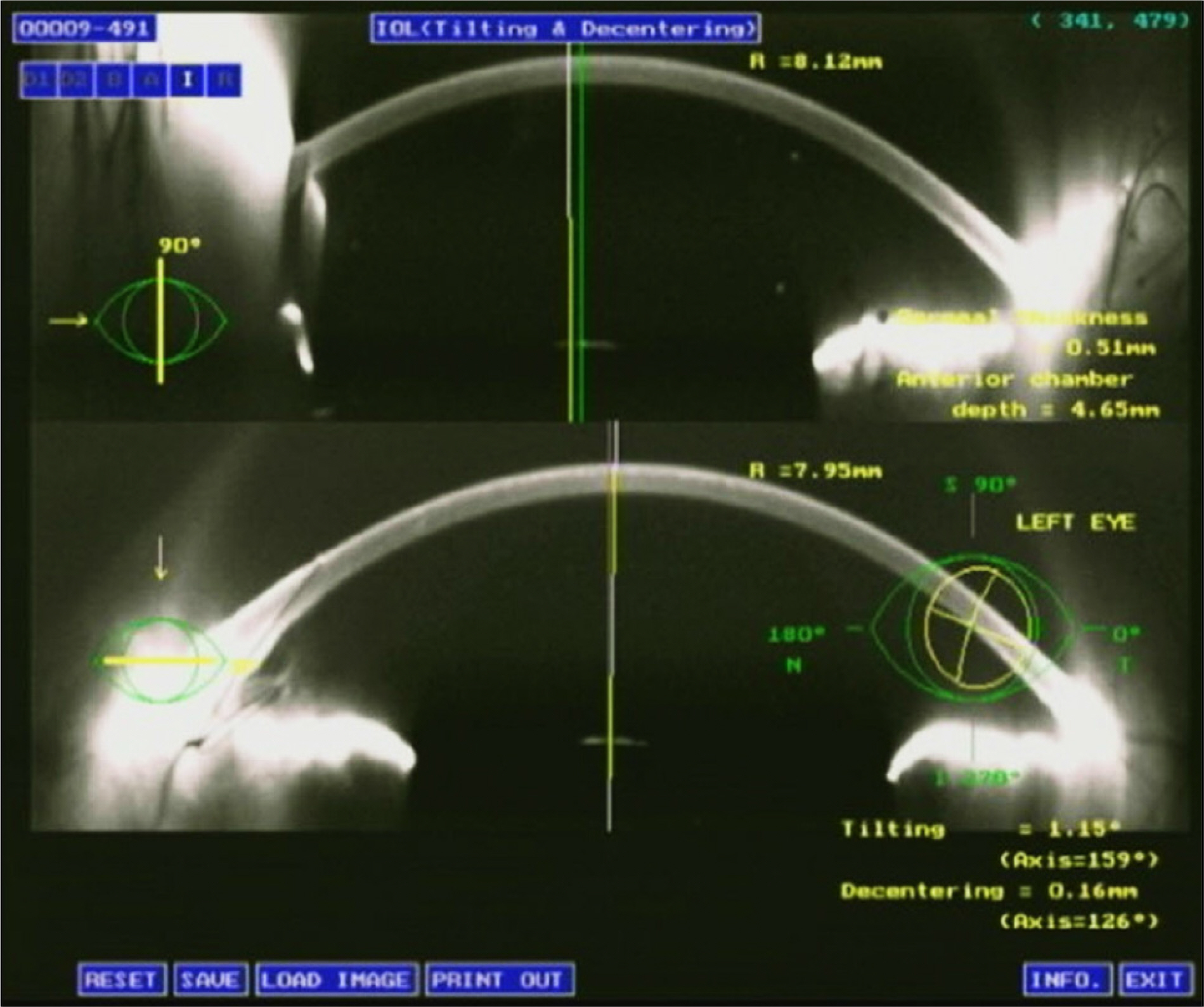
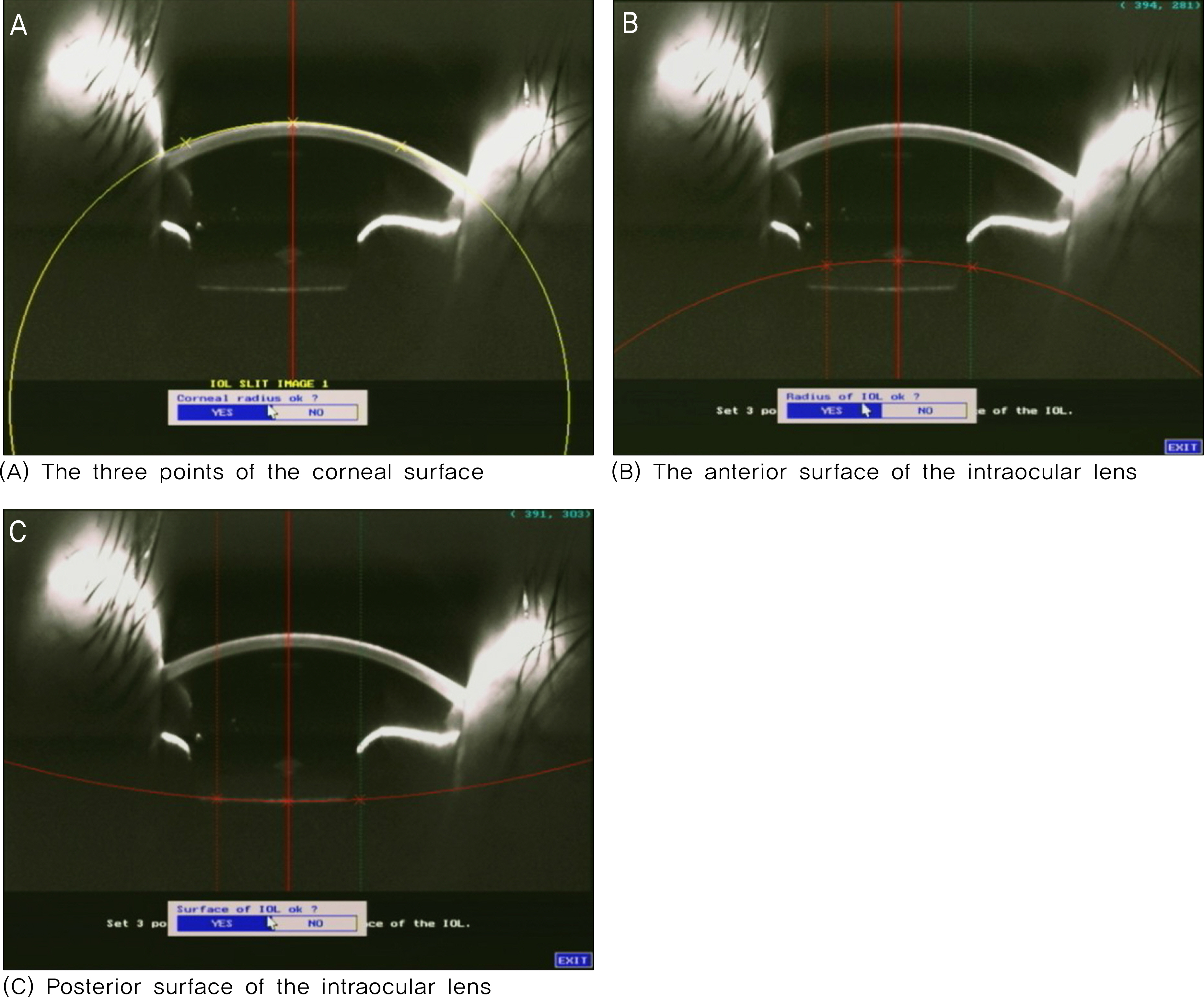
The subjects of this study consisted of 101 eyes who had undergone cataract surgeries with a 3-piece aspheric IOL (54 eyes) and with a single-piece aspheric IOL (47 eyes). The decentration, tilt, anterior chamber depth, and refraction were measured on postoperative day 1, 1 month, and 2 months, using an anterior eye segment analysis system (EAS-1000, Nidek, Japan).
RESULTS
There was a statistically significant difference in the decentration on the postoperative day 1 (p = 0.04). However, there was no statistically significant difference on postoperative 1 month (p = 0.15) and 2 months (p = 0.13). There was no statistically significant difference in the tilt on postoperative day 1, 1 month, and 2 months. There was no statistically significant difference in the anterior chamber depth on postoperative day 1, 1 month, and 2 months. There was a statistically significant difference in the refraction on postoperative day 1 (p = 0.03). However, there was no statistically significant difference on postoperative 1 month (p = 0.07) and 2 months (p = 0.07).
CONCLUSIONS
There was no statistically significant difference in the decentration, anterior chamber depth, and refraction between the 3-piece and single-piece aspheric IOL. Therefore, there is no difference between the 3-piece and single-piece aspheric IOL in the capsular bag stability until 2 months postoperatively.
Keyword
Figure
Reference
-
References
1. Brandser R, Haaskjold E, Drolsum L. Accuracy of IOL calculation in cataract surgery. Acta Ophthalmol Scand. 1997; 75:162–5.
Article2. Zaldivar R, Shultz MC, Davidorf JM, Holladay JT. Intraocular lens power calculation in patients with extreme myopia. J Cataract Refract Surg. 2000; 26:668–4.3. Olsen T, Corydon L, Gimbel H. Intraocular lens power calculation with an improved anterior chamber prediction algorithm. J Cataract Refract Surg. 1995; 21:313–9.4. Minassian DC, Rosen P, Dart JK, et al. Extracapsular cataract extraction compared with small incision surgery by phacoemulsification: a randomized trial. Br J Ophthalmol. 2001; 85:822–9.5. Kondrot EC. Keratometric cylinder and visual recovery following Phacoemulsification and intraocular lens implantation using a self-sealing cataract incision. J Cataract Refract Surg. 1991; 17:731–3.
Article6. Merriam JC, Zheng L, Merriam JE, et al. The effect of incisions for cataract curvature. Ophthalmology. 2003; 110:1807–13.7. Long DA, Monica ML. A prospective evaluation of corneal curvature changes with 3.0 to 3.5 mm corneal tunnel phacoemulsification. Ophthalmology. 1996; 103:226–32.8. Ali JL, Rodfiguez-Prats JL, Gala A, Ramzy M. Outcomes of microincision cataract surgery versus coaxial phacoemulsification. Ophthalmology. 2005; 112:1997–2003.
Article9. Drews RC. Five year study of astigmatic stability after cataract surgery with intraocular lens implantation: comparison of wound sizes. J Cataract Refract Surg. 2000; 26:250–3.
Article10. Nemeth J, Fekete O, Pesztenlehrer N. Optical and ultrasound measurement of axial length and anterior chamber depth for intraocular lens power calculation. J Cataract Refract Surg. 2003; 29:85–8.11. Olsen T, Nielsen PJ. Immersion versus contact technique in the measurement of axial length by ultrasound. Acta Ophthalmol (Copenh). 1989; 67:101–2.
Article12. Watson A, Armstrong R. Contact or immersion technique for axial length measurement. Aust N Z J Ophthalmol. 1999; 27:49–51.13. Rose LT, Moshegov CN. Comparison of Zeiss IOL master and application A-scan ultrasound: biometry for intraocular lens calculation. Clin Experiment Ophthalmol. 2003; 31:121–4.14. Brint SF, Ostrick DM, Bryan JE. Keratometric cylinder and visual performance following phacoemulsification and implantation with silicon small incision or poly(methylmethacrylate) intraocular lenses. J Cataract Refract Surg. 1991; 17:32–6.15. Guirao A, Redondo M, Geraghty E, et al. Corneal optical aberrations and retinal image quality in patients in whom monofocal intraocular lenses were implanted. Arch Ophthalmol. 2002; 120:1143–51.
Article16. Werner L, Mamalis N. Wavefront corrections of intraocular lenses. Ophthalmol Clin North Am. 2004; 17:233–45.
Article17. Chalita MR, Krueger RR. Correlation of aberrations with visual acuity and symptoms. Ophthalmol Clin North Am. 2004; 17:135–42.
Article18. Chae JK, Jang JW, Choi TH, Lee HB. Changes in refraction and anterior chamber depth according to type of intraocular lenes. J Korean Ophthalmol Soc. 2006; 47:1935–42.19. Kim HS, Kim SW, Ha BJ, et al. Ocular aberrations and contrast sensitivity in eyes implanted with aspheric and spherical intraocular lenses. J Korean Ophthalmol Soc. 2008; 49:1256–62.
Article20. Lee J-Y, Lee SH, Chung SK. Decentration, tilt and anterior chamber depth: aspheric vs spheric acrylic intraocular lens. J Korean Ophthalmol Soc. 2009; 50:852–7.
Article21. Ahn HS, Kim SW, Kim EK, Kim TI. Wavefront and visual analysis after aspherical and spherical intraocular lenses implantation. J Korean Ophthalmol Soc. 2008; 49:1248–55.22. Kang IS, You IC, Pack YG, Yoon KC. Comparision of visual function among aspheric intraocular lenes. J Korean Ophthalmol Soc. 2009; 50:691–7.23. Wirtitsch MG, Findl O, Menapace R, et al. Effect of haptic design on change in axial lens position after cataract surgery. J Cataract Refract Surg. 2004; 30:45–51.
Article24. Kim JS, Shyn KH. Periodic Biometry in Three Types of Posteriorly Implanted IOLs: PMMA, Silicone, and Acrylic Soft, by EAS-1000 Scheimpflug Photography. J Korean Ophthalmol Soc. 2000; 41:2205–10.25. Dietze HH, Cox MJ. Limitations of correcting spherical aberration with aspheric intraocular lenses. J Refract Surg. 2005; 31:574–85.
Article26. Mutlu FM, Erdurman C, Sobaci G, Bayraktar MZ. Comparision of tilt and decentration of 1-piece and 3-piece hydrophobic acrylic intraocular lenses. J Cataract Refract Surg. 2005; 31:343–7.27. Cha YD, Oh SH, Lee DH. Comparative assessment of clinical results in various acrylate IOLs. J Korean Ophthalmol Soc. 2006; 47:740–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Anterior Chamber Parameter and Refractive Change between Three-Piece and Single-Piece Aspheric Intraocular Lenses
- Clinical Outcomes of Aspheric 1-Piece (Tecnis(R) ZCB00) and 3-Piece (Tecnis(R) ZA9003) Aspheric Intraocular Lens for 12 Months
- Comparisons of Clinical Results after Implantation of Three Aspheric Intraocular Lenses
- Comparison of Clinical Long-Term Outcomes with Two Types of One-Piece Aspheric Intraocular Lenses after Cataract Surgery
- Assessing Refractive Stability after Cataract Surgery in Axial Myopes: One-piece and Three-piece Intraocular Lenses