J Korean Ophthalmol Soc.
2007 Dec;48(12):1711-1715.
A Case of Ocular Adnexal Benign Reactive Lymphoid Hyperplasia Recurred as Systemic Malignant Lymphoma
- Affiliations
-
- 1Department of Ophthalmology, College of Medicine, Chungnam National University, Daejeon, Korea. sblee@cnu.ac.kr
- 2Research Institute for Medical Science, College of Medicine, Chungnam National University, Daejeon, Korea.
Abstract
-
PURPOSE: We report a case of recurred systemic malignant lymphoma developed after the treatment for ocular adnexal benign reactive lymphoid hyperplasia.
CASE SUMMARY
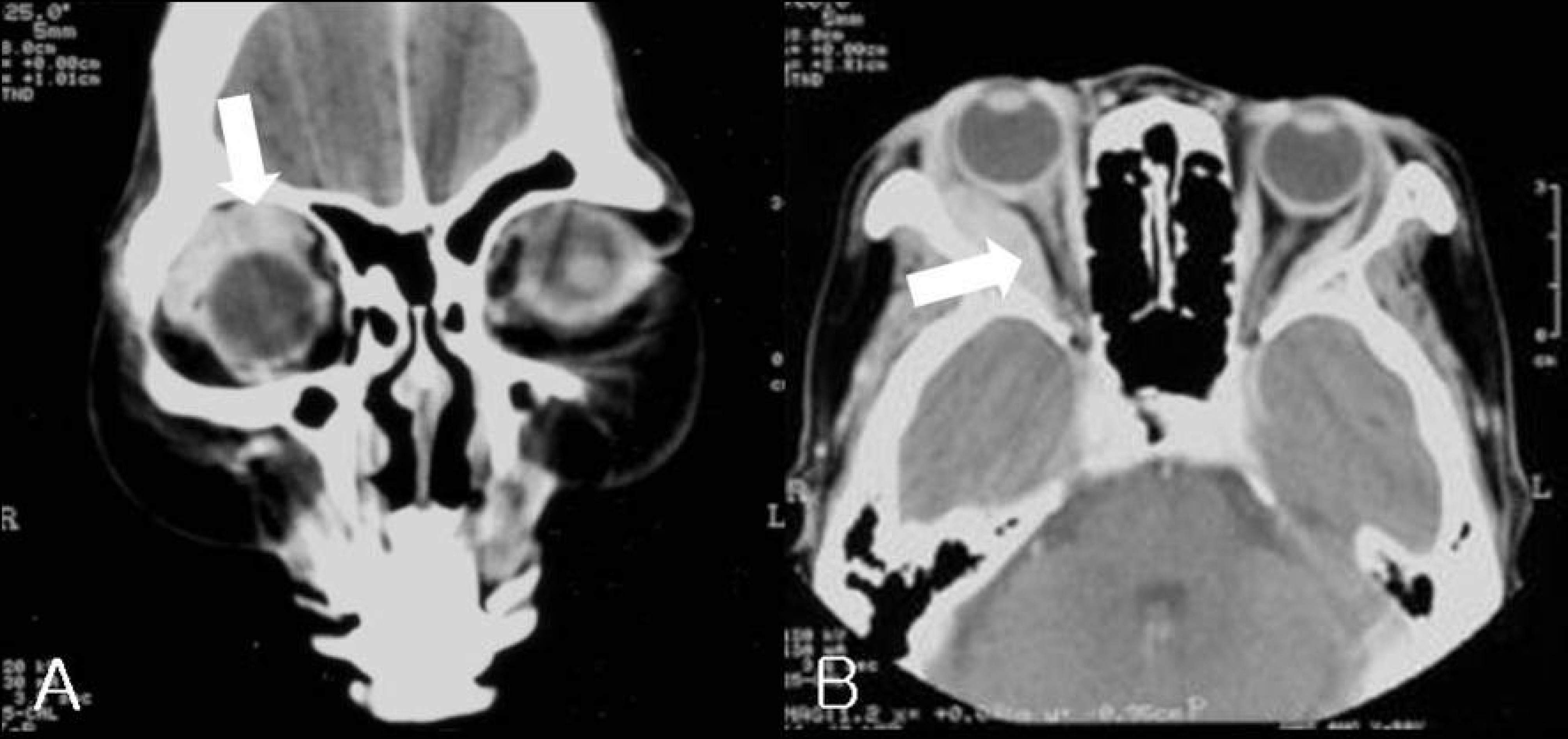
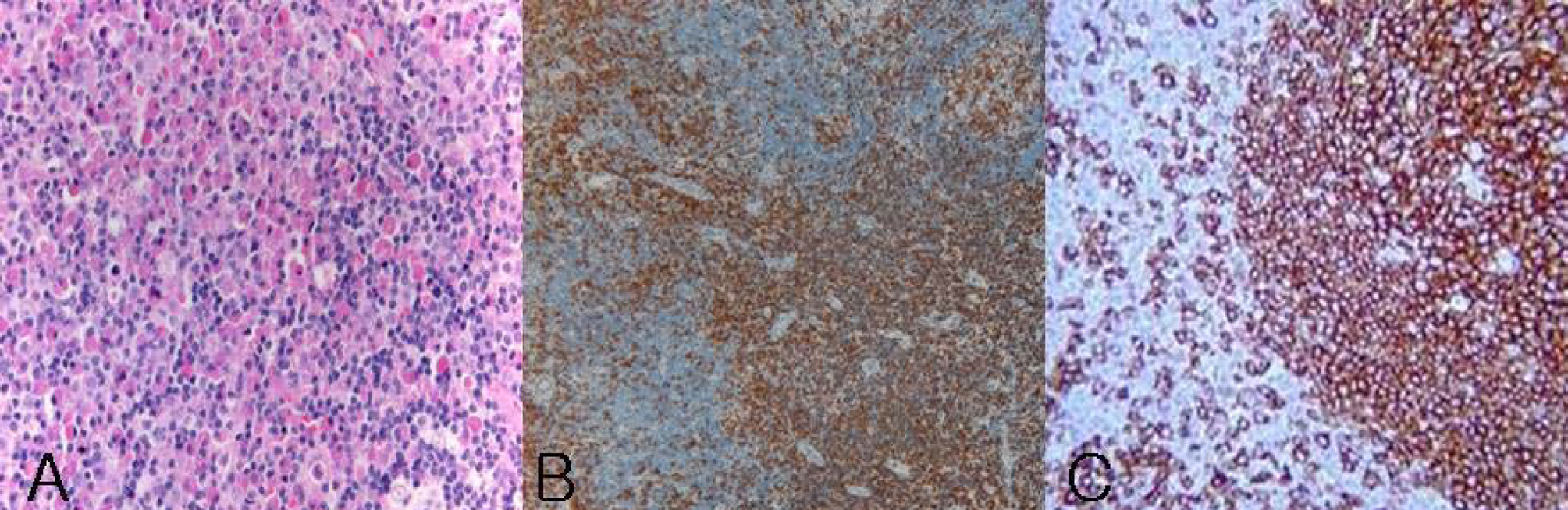
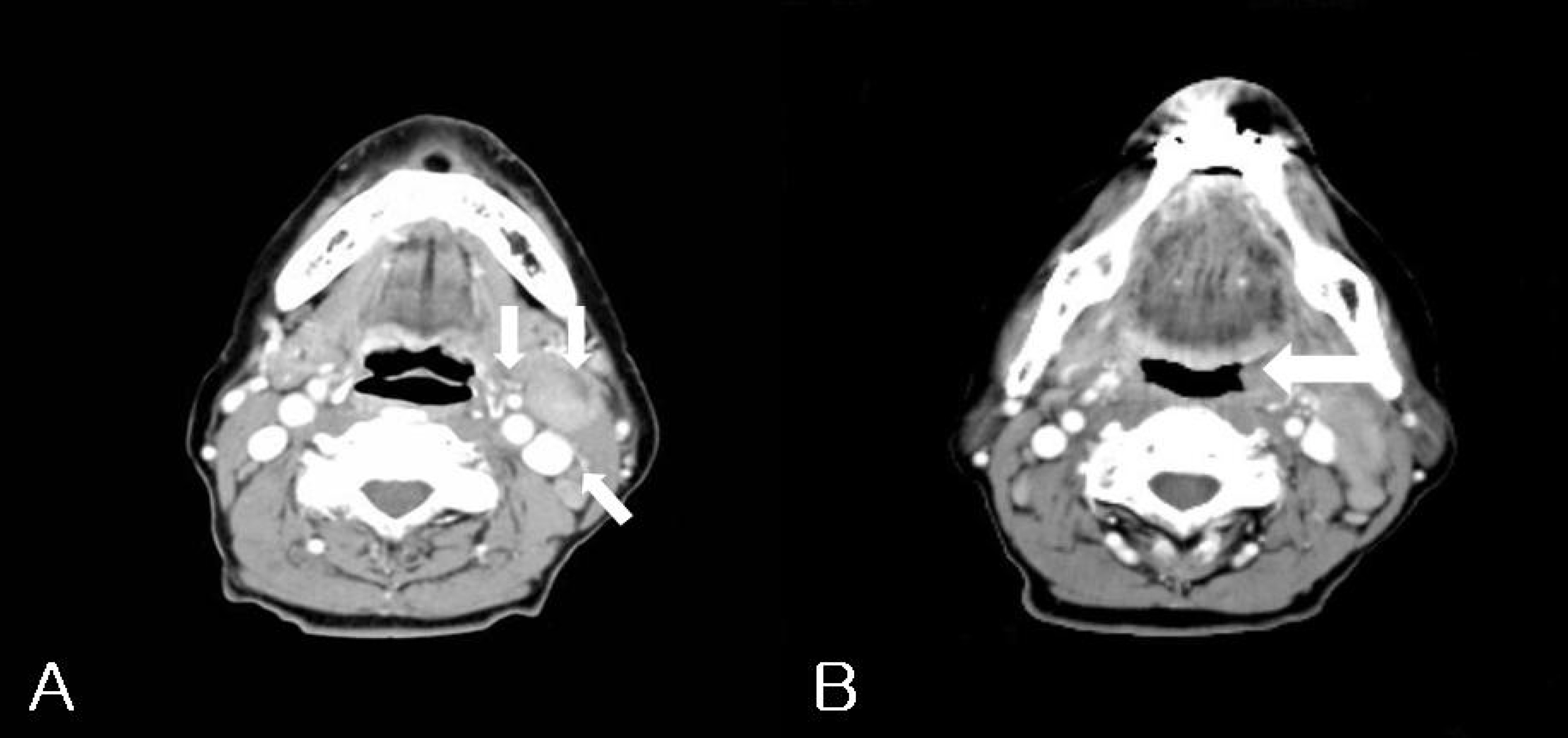
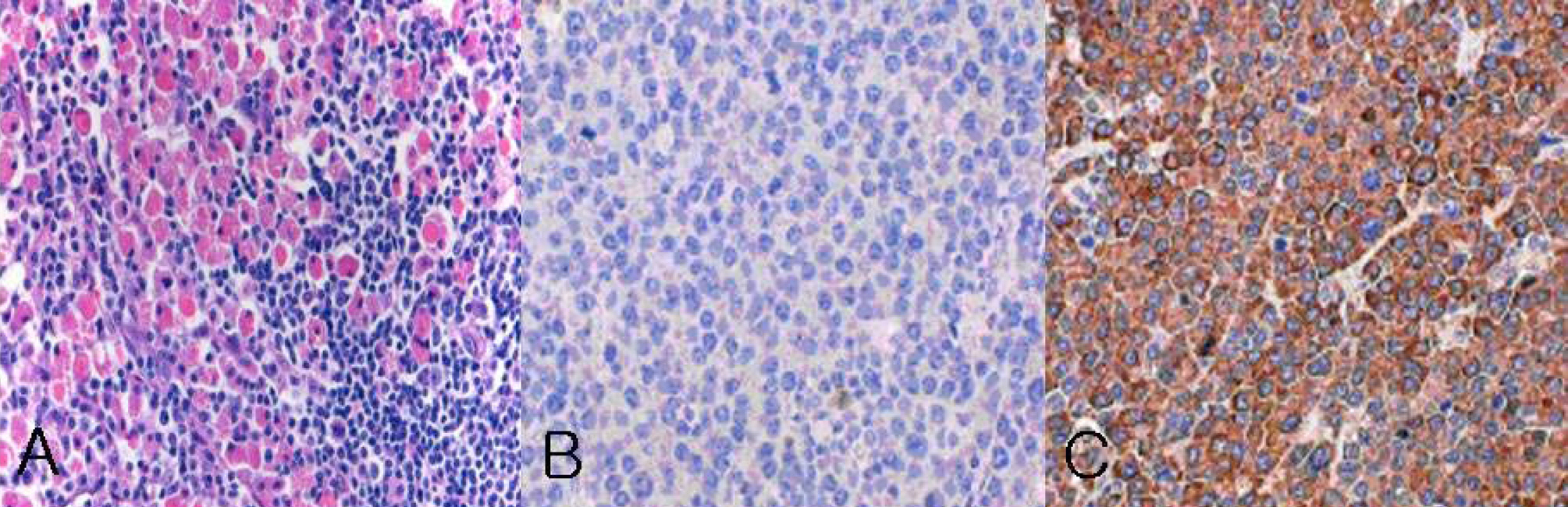
A 71-year-old female visited our hospital for right upper eyelid swelling and proptosis that had been progressing slowly for 4 years. Orbital computed tomography (CT) showed enlargement of the bellies of lateral and superior rectus muscles in the right orbit, but other abnormal findings were not detected in the systemic evaluation. Through incisional biopsy, benign reactive lymphoid hyperplasia was diagnosed on histopathologic examination. Upper eyelid swelling and proptosis resolved after radiation therapy. Fifty-one months after the treatment of benign reactive lymphoid hyperplasia, the patient visited our hospital again for a painful mass that had developed in the left neck. On neck CT, it showed enlargement of the left cervical lymph node and asymmetrical thickening of the left oropharyngeal wall. Systemic MALT lymphoma was confirmed, and radiation therapy was performed. According to neck CT, four months after radiation therapy, the enlargement and thickening resolved.
CONCLUSIONS
Because there is a possibility of systemic malignant lymphoma after benign reactive lymphoid hyperplasia, continuous follow-up and repeated systemic evaluation should be required after treatment of ocular adnexal benign reactive lymphoid hyperplasia.
MeSH Terms
Figure
Reference
-
References
1. Freeman C, Berg JW, Cutler SJ. Occurrence and prognosis of extranodal lymphomas. Cancer. 1972; 29:252–60.
Article2. Knowles DM, Jakobiec FA. Orbital lymphoid neoplasms: A clinicopathologic study of 60 cases. Cancer. 1980; 46:576–89.3. Coupland SE, Krause L, Delecluse HJ, et al. Lympho-proliferative lesions of the ocular adnexa. Analysis of 112 cases. Ophthalmology. 1998; 105:1430–41.4. Knowles DM, Jakobiec FA, McNally L, Burke JS. Lymphoid hyperplasia and malignant lymphoma occurring in the ocular adnexa (orbit, conjunctiva, and eyelids): a prospective multiparametric analysis of 108 cases during 1977 to 1987. Hum Pathol. 1990; 21:959–73.
Article5. Sullivan TJ, Whitehead K, Williamson R, et al. Lympho-proliferative disease of the ocular adnexa: A clinical and pathologic study with statistical analysis of 69 patients. Ophthalmic Plast Reconstr Surg. 2005; 21(3):177–88.
Article6. White WL, Ferry JA, Harris NL, Grove AS Jr. Ocular adnexal lymphoma: A clinicopathologic study with identification of lymphomas of mucosa associated lymphoid tissue type. Ophthalmology. 1995; 102:1994–2006.7. Bessell EM, Henk JM, Wright JE, Whitelocke RA. Orbital and conjunctival lymphoma treatment and prognosis. Radiother Oncol. 1988; 13:237–44.
Article8. Jakobiec FA, McLean I, Font RL. Clinicopathologic characteristics of orbital lymphoid hyperplasia. Ophthalmology. 1979; 86:948–66.
Article9. Johnson TE, Tse DT, Byrne GE Jr, et al. Ocular-adnexal lymphoid tumors: A clinicopathologic and molecular genetic study of 77 patients. Ophthalmic Plast Reconstr Surg. 1999; 15:171–9.10. Lee JW, Chung WS. Treatment of orbital and adnexal malignant lymphoma. J Korean Ophthalmol Soc. 2003; 44:800–5.11. Jo YJ, Yim JH, Park KS. MALT (mucosa associated lymphoid tissue) type lymphoma of the ocular adnexa. J Korean Ophthalmol Soc. 2002; 43:357–62.12. Ji JY, Ahn YC, Kim YD. Radiotherapy for malignant lymphoma of orbit and ocular adnexa. J Korean Ophthalmol Soc. 2005; 46:201–14.13. Lee YS, Lee MI, Park TS, Lee SY. The prognosis of ocular-adnexal lympholiferative lesions. J Korean Ophthalmol Soc. 2003; 44:1260–7.14. Lim DW, Im SK, Yoon KC. Clinical features and treatment results of conjunctival lymphoproliferative lesions. J Korean Ophthalmol Soc. 2004; 45:1820–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Clinicopathologic Characteristics of Lymphoid Tumor of The Orbit and Ocular Adnexa
- The Prognosis of Ocular-adnexal Lymphoproliferative Lesions
- A Case of Primary Jejunal Malignant Lymphoma Associated with Nodular Lymphoid Hyperplasia
- Comparison of Ocular Adnexal Mantle Cell Lymphoma and MALT Lymphoma
- Lymphoid Polyp in the Rectum