Korean J Urol.
2012 Mar;53(3):194-199.
Efficacy of Hydrodistention Implantation Technique in Treating High-Grade Vesicoureteral Reflux
- Affiliations
-
- 1Department of Urology, Korea University Guro Hospital, Seoul, Korea. dgmoon@korea.ac.kr
Abstract
- PURPOSE
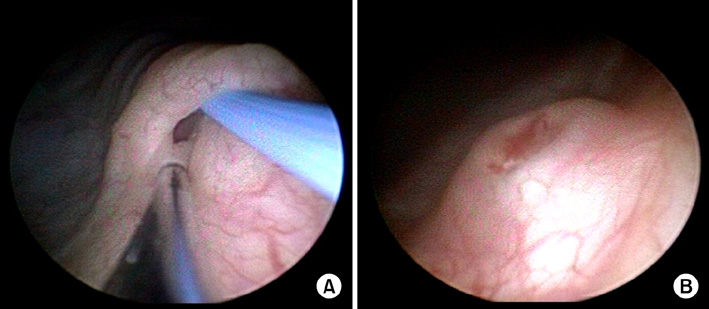
In the endoscopic treatment of vesicoureteral reflux, the relatively high rate of success, the simplicity of the procedure, high patient compliance, and a lack of complications has led to the increased development of injection materials and techniques. We report a method of identifying and maintaining a clear visual field during ureteral and bladder submucosal wall injection of a dextranomer/hyaluronic acid copolymer (Deflux, Oceana, Therapeutics Inc.) by use of the hydrodistention implantation technique (HIT) with the aid of temporary ureteral catheter insertion.
MATERIALS AND METHODS
We prospectively reviewed patients with grade IV or V reflux who received an endoscopic injection of Deflux. Reflux grade was evaluated before and after treatment (3 months) by use of voiding cystourethrograms. Conventional sub-trigonal injection (STING) was performed with injection of Deflux underneath the bladder mucosa at the 6 o'clock position. HIT was performed either with hydrodistention or with guidewire insertion. These techniques increase visualization of the intramural portion of the distal ureteral wall. Patients with treatment failures were offered reinjection up to three times.
RESULTS
Sixty-three patients completed endoscopic injection and follow-up of 3 months. The overall resolution rate for conventional STING was 58%, i.e., 67% for grade IV and 43% for grade V. The overall resolution rate for HIT was 80%, i.e., 93% for grade IV and 66% for grade V. The modified methods showed higher resolution rates for overall cure owing to the success in patients with grade IV reflux (p=0.026). Although the success of grade V treatment was higher with the modified method, the success rate was not statistically significant (p=0.27).
CONCLUSIONS
HIT with the use of either hydrodistention or a guidewire to aid in visualization of the intramural portion of the distal ureter is an effective treatment for high-grade vesico-ureteral reflux.
MeSH Terms
Figure
Reference
-
1. Hodson EM, Wheeler D, Vimalchandra D, Smith G, Craig JC. Interventions for primary vesicoureteric reflux. Cochrane Database Syst Rev. 2007. (3):CD001532.2. Cooper CS. Diagnosis and management of vesicoureteral reflux in children. Nat Rev Urol. 2009. 6:481–489.3. Jacobson SH, Hansson S, Jakobsson B. Vesico-ureteric reflux: occurrence and long-term risks. Acta Paediatr Suppl. 1999. 88:22–30.4. Smellie JM, Jodal U, Lax H, Möbius TT, Hirche H, Olbing H, et al. Outcome at 10 years of severe vesicoureteric reflux managed medically: report of the International Reflux Study in Children. J Pediatr. 2001. 139:656–663.5. Jodal U, Smellie JM, Lax H, Hoyer PF. Ten-year results of randomized treatment of children with severe vesicoureteral reflux. Final report of the International Reflux Study in Children. Pediatr Nephrol. 2006. 21:785–792.6. Elder JS, Peters CA, Arant BS Jr, Ewalt DH, Hawtrey CE, Hurwitz RS, et al. Pediatric vesicoureteral reflux guidelines panel summary report on the management of primary vesicoureteral reflux in children. J Urol. 1997. 157:1846–1851.7. Puri P, Granata C. Multicenter survey of endoscopic treatment of vesicoureteral reflux using polytetrafluoroethylene. J Urol. 1998. 160(3 Pt 2):1007–1011.8. Puri P, Chertin B, Velayudham M, Dass L, Colhoun E. Treatment of vesicoureteral reflux by endoscopic injection of dextranomer/hyaluronic acid copolymer: preliminary results. J Urol. 2003. 170(4 Pt 2):1541–1544.9. Capozza N, Lais A, Nappo S, Caione P. The role of endoscopic treatment of vesicoureteral reflux: a 17-year experience. J Urol. 2004. 172(4 Pt 2):1626–1628.10. Dave S, Lorenzo AJ, Khoury AE, Braga LH, Skeldon SJ, Suoub M, et al. Learning from the learning curve: factors associated with successful endoscopic correction of vesicoureteral reflux using dextranomer/hyaluronic acid copolymer. J Urol. 2008. 180:4 Suppl. 1594–1599.11. Kirsch AJ, Perez-Brayfield MR, Scherz HC. Minimally invasive treatment of vesicoureteral reflux with endoscopic injection of dextranomer/hyaluronic acid copolymer: the Children's Hospitals of Atlanta experience. J Urol. 2003. 170:211–215.12. O'Donnell B, Puri P. Treatment of vesicoureteric reflux by endoscopic injection of Teflon. Br Med J (Clin Res Ed). 1984. 289:7–9.13. Kirsch AJ, Perez-Brayfield M, Smith EA, Scherz HC. The modified sting procedure to correct vesicoureteral reflux: improved results with submucosal implantation within the intramural ureter. J Urol. 2004. 171(6 Pt 1):2413–2416.14. Cerwinka WH, Scherz HC, Kirsch AJ. Endoscopic treatment of vesicoureteral reflux associated with paraureteral diverticula in children. J Urol. 2007. 178(4 Pt 1):1469–1473.15. Kobelt G, Canning DA, Hensle TW, Läckgren G. The cost-effectiveness of endoscopic injection of dextranomer/hyaluronic acid copolymer for vesicoureteral reflux. J Urol. 2003. 169:1480–1485.16. Stenberg A, Lackgren G. Treatment of vesicoureteral reflux in children using stabilized non-animal hyaluronic acid/dextranomer gel (NASHA/DX): a long-term observational study. J Pediatr Urol. 2007. 3:80–85.17. Stenberg A, Läckgren G. A new bioimplant for the endoscopic treatment of vesicoureteral reflux: experimental and short-term clinical results. J Urol. 1995. 154(2 Pt 2):800–803.18. Yu RN, Roth DR. Treatment of vesicoureteral reflux using endoscopic injection of nonanimal stabilized hyaluronic acid/dextranomer gel: initial experience in pediatric patients by a single surgeon. Pediatrics. 2006. 118:698–703.19. Kirsch A, Hensle T, Scherz H, Koyle M. Injection therapy: advancing the treatment of vesicoureteral reflux. J Pediatr Urol. 2006. 2:539–544.20. Lavelle MT, Conlin MJ, Skoog SJ. Subureteral injection of Deflux for correction of reflux: analysis of factors predicting success. Urology. 2005. 65:564–567.21. Higham-Kessler J, Reinert SE, Snodgrass WT, Hensle TW, Koyle MA, Hurwitz RS, et al. A review of failures of endoscopic treatment of vesicoureteral reflux with dextranomer microspheres. J Urol. 2007. 177:710–714.22. Henly DR, Barrett DM, Weiland TL, O'Connor MK, Malizia AA, Wein AJ. Particulate silicone for use in periurethral injections: local tissue effects and search for migration. J Urol. 1995. 153:2039–2043.23. Bhatti HA, Khattak H, Boston VE. Efficacy and causes of failure of endoscopic subureteric injection of Teflon in the treatment of primary vesicoureteric reflux. Br J Urol. 1993. 71:221–225.24. Malizia AA Jr, Reiman HM, Myers RP, Sande JR, Barham SS, Benson RC Jr, et al. Migration and granulomatous reaction after periurethral injection of polytef (Teflon). JAMA. 1984. 251:3277–3281.25. Yurtçu M, Gürbüzer N, Findik S, Avunduk MC, Günel E. Investigation of histopathologic changes in the ureter walls in vesicoureteral reflux. J Pediatr Surg. 2009. 44:802–805.26. Lee BR, Silver RI, Partin AW, Epstein JI, Gearhart JP. A quantitative histologic analysis of collagen subtypes: the primary obstructed and refluxing megaureter of childhood. Urology. 1998. 51:820–823.27. Kirsch A, Elmore J, Molitierno J, Scherz H, editors. The double HIT methodology for the endoscopic correction of vesicoureteral reflux. Proceedings of the Annual Meeting of the American Urological Association. 2006 May 20-25; Atlanta, USA. Linthicum: American Urological Association.