Ann Rehabil Med.
2011 Oct;35(5):648-657. 10.5535/arm.2011.35.5.648.
Peroneal Neuropathy after Tibio-Fibular Fracture
- Affiliations
-
- 1Department of Rehabilitation Medicine, Kyung-pook National University College of Medicine, Daegu 700-721, Korea.
- 2Department of Rehabilitation Medicine, Kyung-pook National University Medical Center, Daegu 700-721, Korea.
- KMID: 2267226
- DOI: http://doi.org/10.5535/arm.2011.35.5.648
Abstract
OBJECTIVE
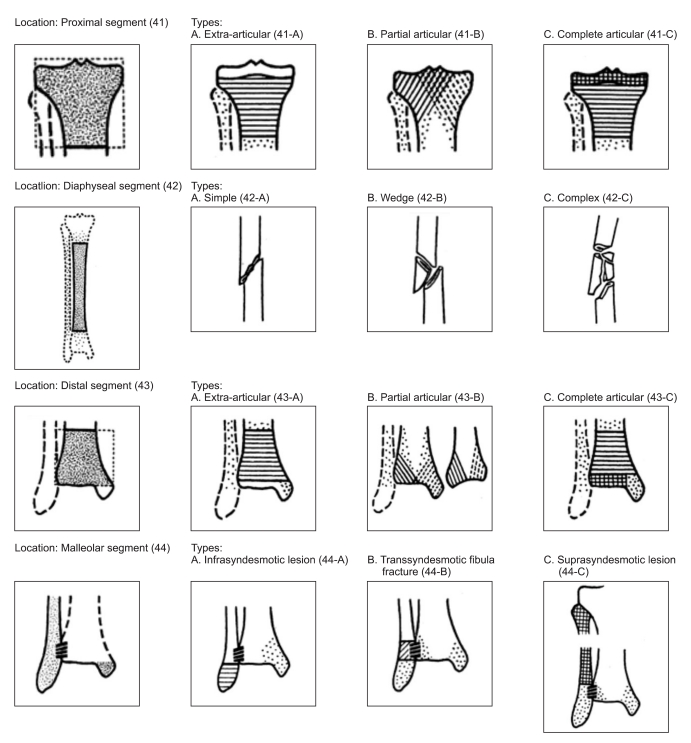
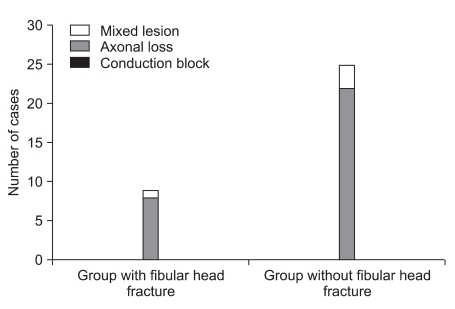
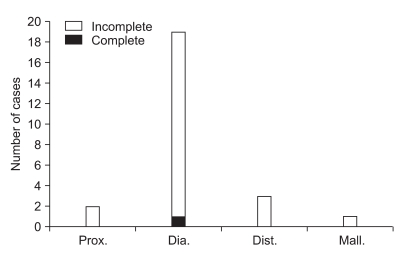
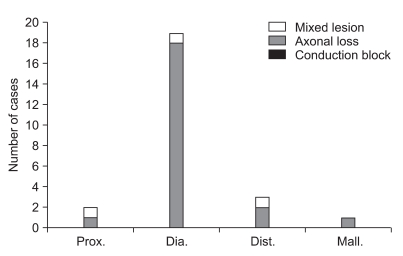
To investigate the injury mechanism in patients who had peroneal neuropathy after a tibio-fibular fracture and the correlation between tibio-fibular fracture location and the severity of the peroneal neuropathy by using electrodiagnosis. METHOD: Thirty-four patients with peroneal neuropathy after a tibio-fibular fracture were recruited for this study. Their medical records, radiologic and electrodiagnostic findings were investigated retrospectively. They were divided into 2 groups according to the existence of a fibular head fracture. The group of patients without the fibular head fracture was further classified according to the criteria of Orthopedic Trauma Association (OTA) classification. The differences between the two groups in the severity of the neuropathy and electrodiagnostic findings were evaluated.
RESULTS
Nine cases (26.5%) had tibio-fibular fractures with a coexisting fibular-head fracture and 25 cases (73.5%) had tibio-fibular fractures without fractures in the fibular-head area. There was no statistical significance in the correlation between the existence of the fibular head fracture and the severity of the electrodiagnostic findings. Neither was there any statistically significant relationship between the site of the tibio-fibular fracture and the severity of the peroneal neuropathy (p>0.05).
CONCLUSION
This study showed there were numerous cases with common peroneal neuropathy after tibiofibular fracture without a coexisting fibular-head fracture, which shows the importance of indirect nerve injury mechanisms as well as that of direct nerve injury as a cause of peroneal neuropathy. In addition, this study showed that there was no statistically significant correlation between the site of tibio-fibular fracture and the severity of peroneal neuropathy.
Keyword
MeSH Terms
Figure
Reference
-
1. Clawson DK, Seddon HJ. The late consequences of sciatic nerve injury. J Bone Joint Surg Br. 1960; 42:213–225. PMID: 13849404.
Article2. Katirji MB, Wilbourn AJ. Common peroneal mononeuropathy: a clinical and electrophysiologic study of 116 lesions. Neurology. 1988; 38:1723–1728. PMID: 2847078.
Article3. Berry H, Richardson PM. Common peroneal nerve palsy: a clinical and electrophysiological review. J Neurol Neurosurg Psychiatry. 1976; 39:1162–1171. PMID: 1011026.
Article4. Smith T, Trojaborg W. Clinical and electrophysiological recovery from peroneal palsy. Acta Neurol Scand. 1986; 74:328–335. PMID: 3811839.
Article5. Oh SJ, Demirci M, Dajani B, Melo AC, Claussen GC. Distal sensory nerve conduction of the superficial peroneal nerve: new method and its clinical application. Muscle Nerve. 2001; 24:689–694. PMID: 11317280.
Article6. Marciniak C, Armon C, Wilson J, Miller R. Practice parameter: utility of electrodiagnostic techniques in evaluating patients with suspected peroneal neuropathy: an evidence-based review. Muscle Nerve. 2005; 31:520–527. PMID: 15768387.
Article7. Ayyar R. MR imaging of the lower leg versus clinical electrophysiologic examination in the differential diagnosis of neurogenic foot drop. AJNR Am J Neuroradiol. 2003; 24:1273–1274. PMID: 12917110.8. Singh H, Behse F, Buchthal F. Electrophysiological study of peroneal palsy. J Neurol Neurosurg Psychiatry. 1974; 37:1202–1213. PMID: 4376162.
Article9. Masakado Y, Kawakami M, Suzuki K, Abe L, Ota T, Kimura A. Clinical neurophysiology in the diagnosis of peroneal nerve palsy. Keio J Med. 2008; 57:84–89. PMID: 18677088.
Article10. Kiechl S. Peer S, Bodner G, editors. Clinical and Electrodiagnostic Work-Up of Peripheral Nerve Lesions. High resolution sonography of the peripheral nervous system. 2008. 2nd ed. Berlin: Springer;p. 52–53.
Article11. Dumitru D, Amato AA, Zwarts MJ. Dumitru D, Amato AA, Zwarts MJ, editors. Peripheral nervous system's reaction to injury. Electrodiagnostic medicine. 2002. 2nd ed. Philadelphia: Hanley & Belfus;p. 129.
Article12. Dumitru D, Amato AA, Zwarts MJ. Dumitru D, Amato AA, Zwarts MJ, editors. Nerve conduction studies. Electrodiagnostic medicine. 2002. 2nd ed. Philadelphia: Hanley & Belfus;p. 159–223.
Article13. Kim DH, Yim SK, Kwon HK, Lee HJ. Clinical and electrophysiologic review of patients with common peroneal mononeuropathy. J Korean Assoc EMG-Electrodiagn Med. 2000; 2:17–23.15. Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, Prokuski L, Sirkin MS, Ziran B, Henley B, et al. Fracture and dislocation classification compendium - 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007; 21:S1–S133. PMID: 18277234.16. Meals RA. Peroneal-nerve palsy complicating ankle sprain. Report of two cases and review of the literature. J Bone Joint Surg Am. 1977; 59:966–968. PMID: 409719.
Article17. Johnston EC, Howell SJ. Tension neuropathy of the superficial peroneal nerve: associated conditions and results of release. Foot Ankle Int. 1999; 20:576–582. PMID: 10509685.
Article18. Stoff MD, Greene AF. Common peroneal nerve palsy following inversion ankle injury: a report of two cases. Phys Ther. 1982; 62:1463–1464. PMID: 7122703.19. Haftek J. Stretch injury of peripheral nerve. Acute effects of stretching on rabbit nerve. J Bone Joint Surg Br. 1970; 52:354–365. PMID: 5445417.20. Nobel W. Peroneal palsy due to hematoma in the common peroneal nerve sheath after distal torsional fractures and inversion ankle sprains. J Bone Joint Surg Am. 1966; 48:1484–1495. PMID: 4289139.
Article21. Whitesides TE, Heckman MM. Acute Compartment Syndrome: Update on Diagnosis and Treatment. J Am Acad Orthop Surg. 1996; 4:209–218. PMID: 10795056.
Article22. Baima J, Krivickas L. Evaluation and treatment of peroneal neuropathy. Curr Rev Musculoskelet Med. 2008; 1:147–153. PMID: 19468889.
Article23. Vural M, Arslantas A. Delayed radial nerve palsy due to entrapment of the nerve in the callus of a distal third humerus fracture. Turk Neurosurg. 2008; 18:194–196. PMID: 18597237.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationship of Tibial Nonunion with Fibular Nonunion in the Tibio-fibular Shaft Fracture
- The effects of the flbular stabilization in the treatment of tibio-fibula shaft fracture
- Congenital Distal Tibio-fibular Synostosis: Case Report
- Common peroneal neuropathy after surgery in the lithotomy position : A case report
- The Common Peroneal Nerve Injuries