Korean J Hematol.
2010 Dec;45(4):247-252. 10.5045/kjh.2010.45.4.247.
Role of p16 in the pathogenesis of Langerhans cell histiocytosis
- Affiliations
-
- 1Department of Pediatrics, College of Medicine, Hanyang University Hospital, Seoul, Korea.
- 2Department of Laboratory Medicine & Genetics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Division of Pediatric Hematology/Oncology, Department of Pediatrics, University of Ulsan College of Medicine & Asan Medical Center, Seoul, Korea. jjseo@amc.seoul.kr
- 4Department of Medical Genetics, College of Medicine, Hanyang University, Seoul, Korea.
- KMID: 2252035
- DOI: http://doi.org/10.5045/kjh.2010.45.4.247
Abstract
- BACKGROUND
It has been hypothesized that genetic alteration at the cellular level may have a significant effect on cellular mechanisms controlling the proliferation and apoptosis of Langerhans cells (LCs).
METHODS
We examined whether p16 protein expression can be used to predict the outcome of Langerhans cell histiocytosis (LCH). Archival paraffin blocks from children diagnosed with LCH and followed at the Asan Medical Center and Chungnam National University Hospital between March 1998 and February 2008 were studied.
RESULTS
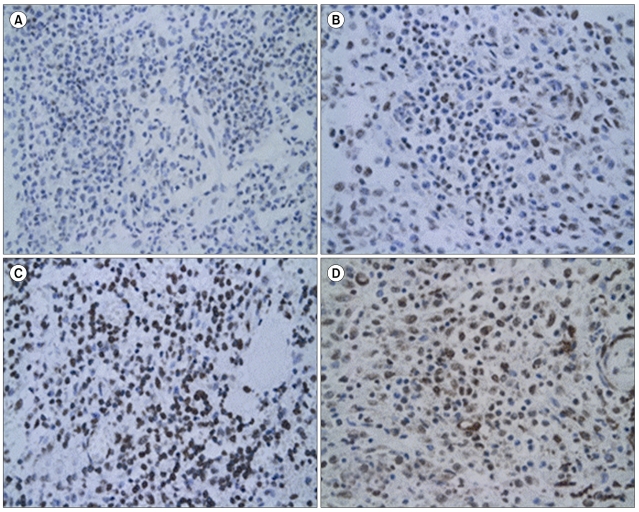
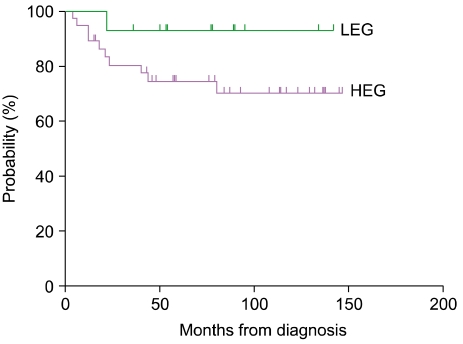
Slides were stained with p16 antibody and evaluated semi-quantitatively using the following scale: negative, no staining; +/-, weakly positive; 1+, staining similar to lymphocytes surrounding the LCs; 2+, stronger staining than lymphocytes; 3+, much stronger staining than lymphocytes. Negative and +/- groups were assigned to a lower expression group (LEG) and the 1+, 2+, and 3+ groups were assigned to a higher expression group (HEG). The median age of the 51 patients (24 girls, 27 boys) was 49 (range, 0.6-178) months, and LCH was diagnosed based on CD1a positivity. p16 protein was expressed to varying degrees in all but one specimen. There was a greater tendency toward multisystem disease, risk organ involvement, and relapse in the HEG than in the LEG.
CONCLUSION
The p16 protein may have a significant effect on cellular mechanisms controlling the proliferation and apoptosis of LCs, and thus may influence the clinical outcome and prognosis of LCH.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Prognostic significance of gelsolin and MMP12 in Langerhans cell histiocytosis
Jong-Jin Seo, Taeshik Cho, Sun-Young Kim, Ibrahim Nassour, Hee-Jin Kim, Yeon-Jung Lim, Kyung-Nam Koh, Ho-Joon Im
Korean J Hematol. 2012;47(4):267-272. doi: 10.5045/kjh.2012.47.4.267.
Reference
-
1. Satter EK, High WA. Langerhans cell histiocytosis: a review of the current recommendations of the Histiocyte Society. Pediatr Dermatol. 2008; 25:291–295. PMID: 18577030.
Article2. Amir G, Weintraub M. Association of cell cycle-related gene products and NF-kappaB with clinical parameters in Langerhans cell histiocytosis. Pediatr Blood Cancer. 2008; 50:304–307. PMID: 17455317.
Article3. Weitzman S, Egeler RM. Langerhans cell histiocytosis: update for the pediatrician. Curr Opin Pediatr. 2008; 20:23–29. PMID: 18197035.
Article4. Petersen BL, Rengtved P, Bank MI, Carstensen H. High expression of markers of apoptosis in Langerhans cell histiocytosis. Histopathology. 2003; 42:186–193. PMID: 12558751.
Article5. Schouten B, Egeler RM, Leenen PJ, Taminiau AH, van den Broek LJ, Hogendoorn PC. Expression of cell cycle-related gene products in Langerhans cell histiocytosis. J Pediatr Hematol Oncol. 2002; 24:727–732. PMID: 12468913.
Article6. Bank MI, Rengtved P, Carstensen H, Petersen BL. p53 expression in biopsies from children with Langerhans cell histiocytosis. J Pediatr Hematol Oncol. 2002; 24:733–736. PMID: 12468914.
Article7. Guo SX, Taki T, Ohnishi H, et al. Hypermethylation of p16 and p15 genes and RB protein expression in acute leukemia. Leuk Res. 2000; 24:39–46. PMID: 10634644.
Article8. Chim CS, Wong AS, Kwong YL. Epigenetic inactivation of the CIP/KIP cell-cycle control pathway in acute leukemias. Am J Hematol. 2005; 80:282–287. PMID: 16315255.
Article9. Chim CS, Wong KY, Loong F, Lam WW, Srivastava G. Frequent epigenetic inactivation of Rb1 in addition to p15 and p16 in mantle cell and follicular lymphoma. Hum Pathol. 2007; 38:1849–1857. PMID: 17900658.
Article10. Drexler HG. Review of alterations of the cyclin-dependent kinase inhibitor INK4 family genes p15, p16, p18 and p19 in human leukemia-lymphoma cells. Leukemia. 1998; 12:845–859. PMID: 9639410.
Article11. Psofaki V, Kalogera C, Tzambouras N, et al. Promoter methylation status of hMLH1, MGMT, and CDKN2A/p16 in colorectal adenomas. World J Gastroenterol. 2010; 16:3553–3560. PMID: 20653064.12. de Snoo FA, Bishop DT, Bergman W, et al. Increased risk of cancer other than melanoma in CDKN2A founder mutation (p16-Leiden)-positive melanoma families. Clin Cancer Res. 2008; 14:7151–7157. PMID: 18981015.
Article13. Suga Y, Miyajima K, Oikawa T, et al. Quantitative p16 and ESR1 methylation in the peripheral blood of patients with non-small cell lung cancer. Oncol Rep. 2008; 20:1137–1142. PMID: 18949413.
Article14. Glotzbecker MP, Carpentieri DF, Dormans JP. Langerhans cell histiocytosis: clinical presentation, pathogenesis, and treatment from the LCH etiology research group at the Children's Hospital of Philadelphia. UPOJ. 2002; 15:67–73.15. Alston RD, Tatevossian RG, McNally RJ, Kelsey A, Birch JM, Eden TO. Incidence and survival of childhood Langerhans cell histiocytosis in Northwest England from 1954 to 1998. Pediatr Blood Cancer. 2007; 48:555–560. PMID: 16652350.
Article16. Willman CL, McClain KL. An update on clonality, cytokines, and viral etiology in Langerhans cell histiocytosis. Hematol Oncol Clin North Am. 1998; 12:407–416. PMID: 9561909.
Article17. Weiss LM, Wood GS, Trela M, Warnke RA, Sklar J. Clonal T-cell populations in lymphomatoid papulosis. Evidence of a lymphoproliferative origin for a clinically benign disease. N Engl J Med. 1986; 315:475–479. PMID: 3488502.18. Chikwava KR, Hunt JL, Mantha GS, Murphy JE, Jaffe R. Analysis of loss of heterozygosity in single-system and multisystem Langerhans' cell histiocytosis. Pediatr Dev Pathol. 2007; 10:18–24. PMID: 17378622.
Article19. Bechan GI, Egeler RM, Arceci RJ. Biology of Langerhans cells and Langerhans cell histiocytosis. Int Rev Cytol. 2006; 254:1–43. PMID: 17147996.
Article20. Bringold F, Serrano M. Tumor suppressors and oncogenes in cellular senescence. Exp Gerontol. 2000; 35:317–329. PMID: 10832053.
Article21. Basu A, Haldar S. The relationship between BcI2, Bax and p53: consequences for cell cycle progression and cell death. Mol Hum Reprod. 1998; 4:1099–1109. PMID: 9872359.
Article22. Reed JC. Regulation of apoptosis by bcl-2 family proteins and its role in cancer and chemoresistance. Curr Opin Oncol. 1995; 7:541–546. PMID: 8547403.
Article23. Savell VH Jr, Sherman T, Scheuermann RH, Siddiqui AM, Margraf LR. Bcl-2 expression in Langerhans' cell histiocytosis. Pediatr Dev Pathol. 1998; 1:210–215. PMID: 10463280.
Article24. Kataoka M, Wiehle S, Spitz F, Schumacher G, Roth JA, Cristiano RJ. Down-regulation of bcl-2 is associated with p16INK4-mediated apoptosis in non-small cell lung cancer cells. Oncogene. 2000; 19:1589–1595. PMID: 10734319.
Article25. Modesitt SC, Ramirez P, Zu Z, Bodurka-Bevers D, Gershenson D, Wolf JK. In vitro and in vivo adenovirus-mediated p53 and p16 tumor suppressor therapy in ovarian cancer. Clin Cancer Res. 2001; 7:1765–1772. PMID: 11410518.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recent Updates in Langerhans Cell Histiocytosis
- Spontaneous Pneumothorax due to Pulmonary Invasion in Multisystemic Langerhans Cell Histiocytosis: A case report
- Pulmonary Langerhans Cell Histiocytosis Accompanied by Active Pulmonary Tuberculosis
- A Case of Orbital Langerhans' cell histiocytosis
- A Case of Pulmonary Langerhans Cell Histiocytosis with Pneumothorax